
Cardiovascular
Question 1:
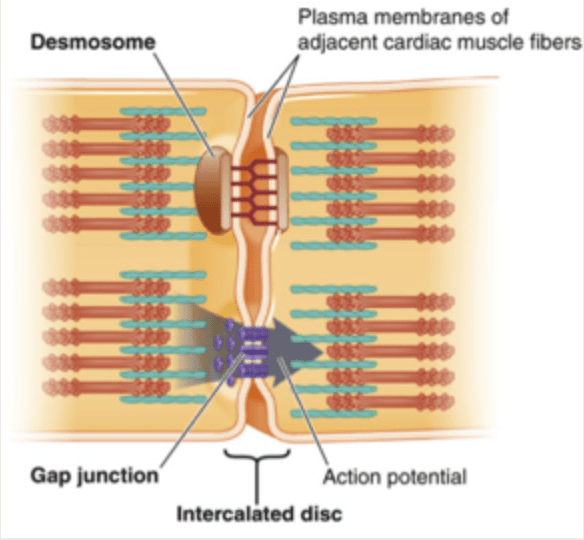
Answer: B) Contains intercalated discs
Explanation: Heart muscle, unlike skeletal muscle, contains intercalated discs, which are specialised cell-cell junctions that allow for coordinated & synchronised contractions in cardiac tissue. Intercalated discs are composed of: gap junctions, desmosomes & fascia adherens.
Option A is incorrect because skeletal muscles are unbranched and are multinucleated, unlike cardiac muscles which are branched and have a single nucleus per cell.
Option C is incorrect because cardiac muscle cells are uninucleated, meaning they typically have a single nucleus.
Option D is incorrect because cardiac muscles are striated due to the organised arrangement of actin and myosin filaments. The presence of striations is a key histological feature of cardiac muscle.
Option E is incorrect because although cardiac muscles do contain desmosomes, this is not the most specific and defining feature of cardiac muscle histology. Desmosomes are part of the intercalated discs but do not uniquely describe cardiac muscle as compared to other muscle types.
Question 2:
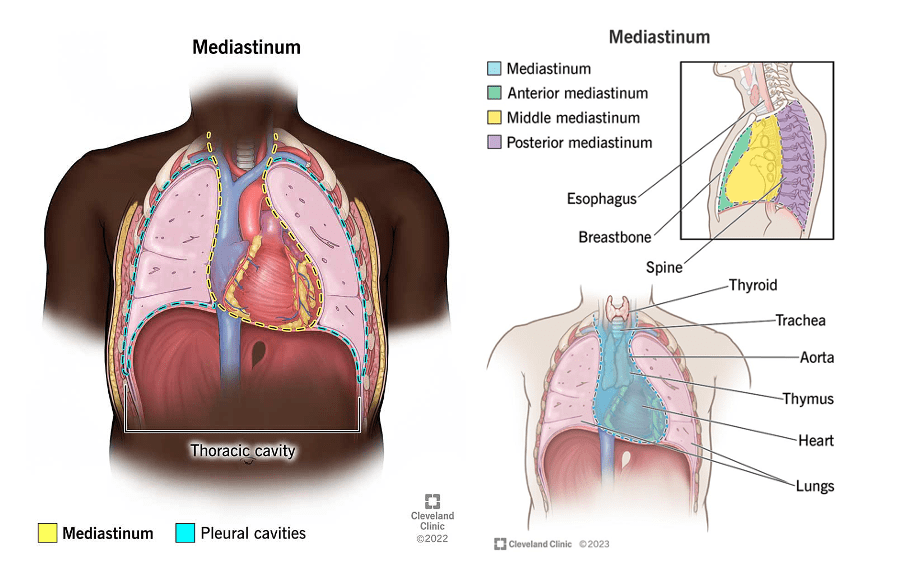
Answer: B) The central compartment of the thoracic cavity; contains the heart and major blood vessels.
Explanation: The mediastinum is the central compartment of the thoracic cavity, housing vital structures such as the heart, major blood vessels, oesophagus, and trachea.
Option D is incorrect because the mediastinum does not contain the lungs. The lungs are located in the pleural cavities on either side of the mediastinum.
Question 3:
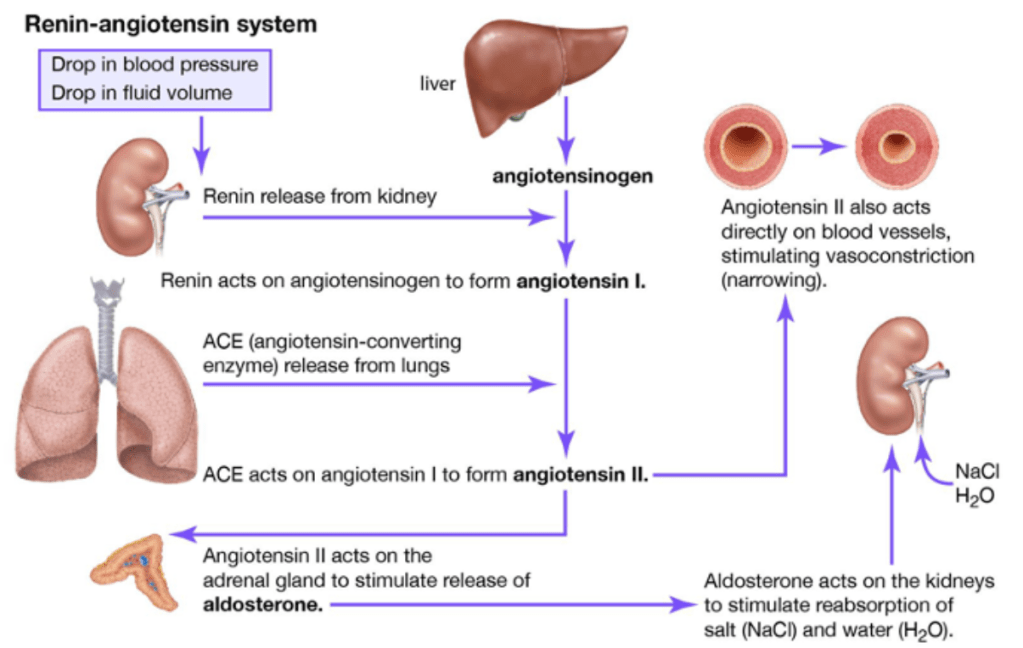
Answer: B) Decreased blood pressure in the kidneys
Explanation: Renin is released by the kidneys when they sense decreased blood pressure (low sodium concentration) or blood volume. This triggers the renin-angiotensin-aldosterone system, leading to increased blood pressure and volume to restore homeostasis.
Option A is incorrect because a low concentration of sodium in the distal convoluted tubule detected by macula densa cells triggers the release of renin, not a high concentration of sodium.
Option C is incorrect because renin release is primarily influenced by factors such as blood pressure and sodium concentration, not potassium levels.
Option D is incorrect because renin release is stimulated by the sympathetic nervous system, particularly through beta-adrenergic receptor activation not parasympathetic nervous system.
Option E is incorrect because hormones released by the kidneys such as erythropoietin, do not trigger the release of renin. Instead, renin release is a response to decreased blood pressure or volume, sensed by the juxtaglomerular cells in the kidneys or detected by macula densa cells in the distal convoluted tubule which signal to juxtaglomerular cells to secrete renin.
Question 4:
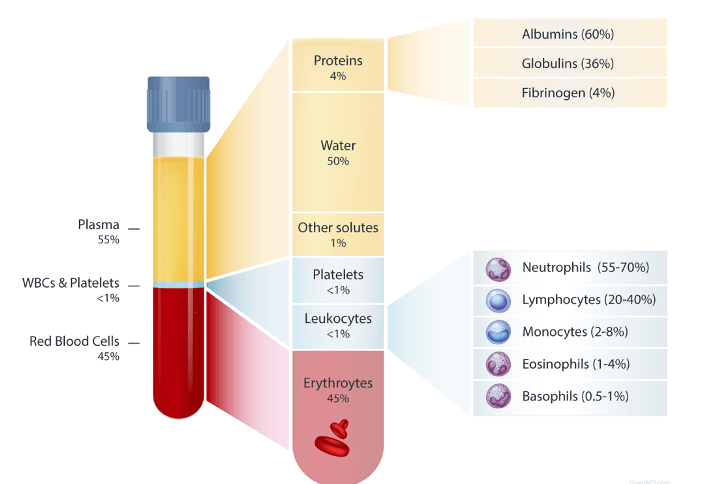
Answer: C) 55% plasma (proteins, water & gases) & 45% red blood cells (<1% white blood cells, platelets).
Explanation: Blood is composed of red and white blood cells, along with platelets that aid in clotting, all suspended in a liquid called plasma, which contains various essential substances like electrolytes and proteins.
Option E is incorrect because it lists haemoglobin as 45% of the blood, which is incorrect. Haemoglobin is a component within red blood cells, not a separate part of the blood composition.
Question 5:
Answer: E) Afterload
Explanation: Afterload refers to the resistance the left ventricle must overcome to eject blood during systole. It’s a critical factor in assessing cardiac performance.
Option A is incorrect because preload refers to the stretching of the ventricular muscle fibres at the end of diastole, just before contraction, due to the volume of blood returning from the body & filling the ventricle.
Option B is incorrect because contractility refers to the intrinsic ability of the heart muscle to contract independently of preload or afterload.
Option C is incorrect because loading phase is not a specific term used to describe the force the left ventricle pumps against during systole.
Option D is incorrect because mean arterial pressure (MAP) is a measure of the average pressure within the arteries not the cardiac cycle.
Question 6:
Answer: C) Free fatty acids
Explanation: The heart predominantly utilises free fatty acids as a source of energy because they provide a sustained and efficient supply of ATP, supporting the heart’s continuous work.
Option A is incorrect because although glucose is an important energy source for the heart especially following a meal containing a large volume of carbohydrates, what distinguishes the heart from other muscles in the body is that it favours free fatty acids over other energy sources.
Option B is incorrect because amino acids are not typically preferred by the heart for energy production under normal circumstances.
Option D is incorrect because although ketones can serve as an alternative energy source for the heart, they are not the preferred metabolite.
Option E is incorrect because phosphocreatine is primarily involved in providing rapid energy for muscle contraction and is not a preferred metabolic substrate for the heart.
Question 7:
Answer: C) It allows blood to bypass the pulmonary circulation by shunting blood from the right atrium to the left atrium.
Explanation: During fetal development, the lungs are not yet functioning, and the baby receives oxygenated blood from the mother through the placenta. To efficiently bypass the non-functional lungs, the foramen ovale acts as a “trapdoor” between the right and left atria, allowing oxygen-rich blood to flow from the right atrium directly into the left atrium. This shunts the blood away from the pulmonary circulation and into the systemic circulation, ensuring that the developing fetus receives oxygenated blood.
Option B is incorrect because it describes the function of the ductus arteriosus, not the foramen ovale.
Option D is incorrect because it describes the function of the ductus venosus, not the foramen ovale.
Option E is incorrect because it is the wrong direction in which blood is shunted in the foramen ovale.

Question 8:
Answer: C) SA node initiates heart beat & AV node coordinates heart beat
Explanation: The conduction system of the heart consists of specialised cells and structures that coordinate the heart’s electrical signals, ensuring its rhythmic contractions. The SA (sinoatrial) node, often called the heart’s natural pacemaker, generates electrical impulses. These impulses then travel to the AV (atrioventricular) node, which acts as a relay station, delaying the signal slightly to allow the atria to contract before the ventricles. This coordinated electrical activity ensures efficient blood pumping by the heart.
Option A is incorrect because while the SA node initiates the heartbeat, it is not solely responsible for coordinating heartbeats throughout the entire cardiac cycle.
Option B is incorrect because while the AV node delays the electrical impulse, it is not solely responsible for coordinating heartbeats throughout the entire cardiac cycle.
Option D is incorrect because the SA node, not the AV node, initiates the heartbeat by generating electrical impulses.
Question 9:
Answer: C) Calcium triggers the interaction between actin and myosin
Explanation: Calcium ions play a crucial role in cardiac muscle contraction. When an action potential travels down the cardiac muscle cell, it causes calcium to be released from storage within the cell. This calcium binds to the contractile proteins actin and myosin, allowing them to interact. As actin and myosin slide past each other, this results in muscle contraction, which is essential for pumping blood throughout the body.
Option A is incorrect because the maintenance of the resting membrane potential in cardiac cells primarily involves the movement of potassium and sodium ions.
Option B is incorrect because the depolarisation of the action potential in cardiac cells is primarily due to the influx of sodium ions.
Option D is incorrect because while calcium is involved in various cellular processes, including muscle contraction, it is not directly required for the formation of ATP (adenosine triphosphate).
Option E is incorrect because although NCX (sodium-calcium exchanger) does result in sodium entering the cell, the main function of this transporter is to remove calcium from the cell to prevent any contractions of cardiac muscle which may lead to arrythmias. The exchange of sodium into the cell typically involves voltage gated-sodium channels and sodium-potassium pumps.

Question 10:
Answer: C) The relationship between preload and stroke volume, indicating that an increase in preload results in a greater stroke volume.
Explanation: Starling’s law emphasises the relationship between the amount of blood filling the heart (preload) and the force of contraction (stroke volume). When the heart is filled with a larger volume of blood, the muscle fibres are stretched more, leading to a more forceful contraction. This ensures that the heart can adapt to varying venous return and maintain an adequate cardiac output to meet the body’s demands.
Question 11:
Answer: E) A condition characterised by the narrowing of blood vessels outside of the heart, typically in the legs.
Explanation: Peripheral vascular disease (PVD) refers to a group of disorders in which blood vessels outside the heart, primarily in the legs, become narrowed or blocked. This narrowing, often due to atherosclerosis, reduces blood flow to the affected areas. PVD can lead to symptoms such as leg pain during exercise (claudication) and, if severe, can result in tissue damage and even amputation. It underscores the importance of healthy peripheral circulation for overall well-being.
Question 12:
Answer: B) The three factors that contribute to thrombosis: stasis of blood flow, endothelial injury, and hypercoagulability.
Explanation: Virchow’s Triad outlines the three key factors that contribute to thrombosis (abnormal blood clot formation) in blood vessels. These factors include stasis of blood flow (when blood moves too slowly or not at all), endothelial injury (damage to the inner lining of blood vessels), and hypercoagulability (an increased tendency of the blood to clot). Understanding these factors is crucial for assessing the risk of thrombotic events.
Question 13:
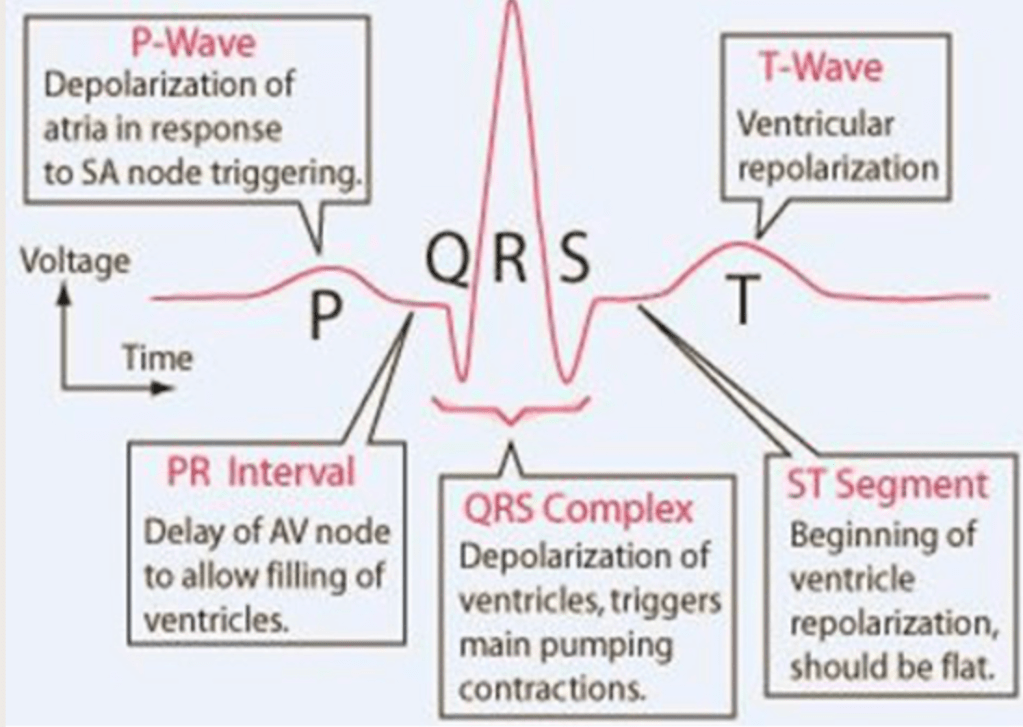
Answer: D) T wave
Explanation: In an electrocardiogram (ECG), the T wave represents ventricular repolarisation. This phase indicates the recovery and resetting of the cardiac muscle cells in the ventricles after contraction, preparing them for the next heartbeat.
Option A is incorrect because the P wave represents atrial depolarisation.
Option B is incorrect because the PR interval measures the time from atrial depolarisation to ventricular depolarisation. It represents the delay in the AV node.
Option C is incorrect because the QRS complex represents ventricular depolarisation.
Option E is incorrect because the QT interval measures the total time between ventricular depolarisation and repolarisation.

Question 14:
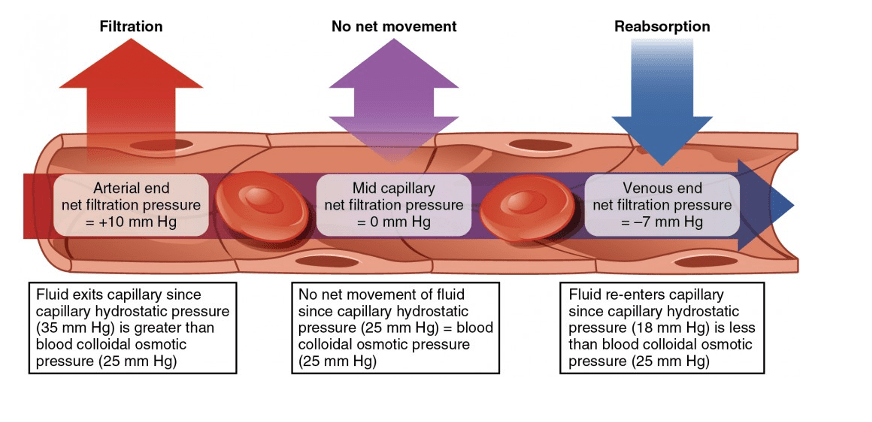
Answer: C) By returning excess interstitial fluid to the bloodstream.
Explanation: The lymphatic system plays a critical role in maintaining fluid balance by collecting excess interstitial fluid (the fluid surrounding cells) and returning it to the bloodstream. This process helps prevent the accumulation of tissue fluid and maintains overall fluid equilibrium in the body by absorbing any excess fluid in the interstitial space.
Option A is incorrect because regulating blood pressure is primarily the function of the cardiovascular system, not the lymphatic system.
Option E is incorrect because allowing movement of fluid from the bloodstream to interstitial fluid is regulated by the cardiovascular system. High hydrostatic pressure (caused by contraction of the left ventricle), forces fluid out of arterioles into the interstitial space surrounding cells.

Question 15:
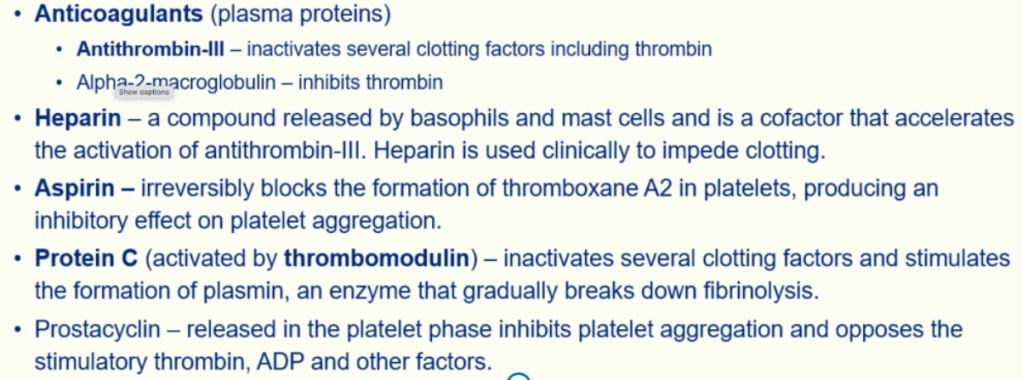
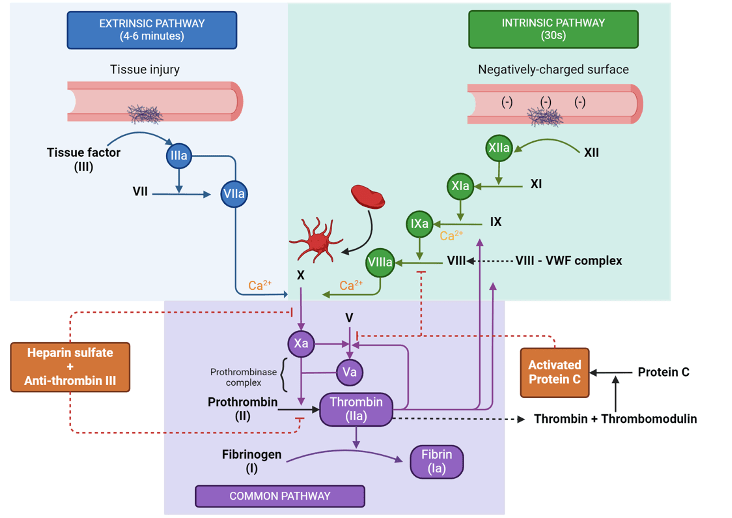
Answer: B) Thrombin activation
Explanation: Thrombin activation is a crucial step in the blood clotting process. Thrombin is an enzyme that converts soluble fibrinogen into insoluble strands of fibrin, forming a mesh-like structure that traps blood cells to create a stable blood clot in response to injury.
Option A is incorrect because vasoconstriction aka vascular spasms (1st stage blood damage) is required to reduce the size of the damaged blood vessel. Vasoconstriction is also not primarily involved in blood clot formation (2nd stage of blood damage).
Option C is incorrect because endothelin is a peptide that constricts blood vessels and is not essential for blood clot formation.
Option D is incorrect because Protein C is involved in inhibiting clotting factors and is anticoagulant, not procoagulant.
Option E is incorrect because prostacyclin (also known as prostaglandin I2) inhibits platelet aggregation and is antithrombotic.
Question 16:
Answer: C) Enhancing sodium reabsorption in the kidneys and facilitating potassium excretion.
Explanation: Aldosterone is a hormone that acts on the kidneys to regulate sodium and potassium balance in the body. It enhances sodium reabsorption by the kidneys, which leads to increased water retention, blood volume, and blood pressure, while also facilitating potassium excretion.
Option A is incorrect because accelerating heart rate by the sympathetic nervous system and hormonal influences like adrenaline (epinephrine) & noradrenaline.
Option B is incorrect because vasoconstriction of blood vessels is primarily mediated by angiotensin II.
Option D is incorrect because while aldosterone indirectly affects blood pressure through its effects on sodium and water reabsorption, its primary function is not directly to increase blood pressure. This is one of the main functions of angiotensin II.
Option E is incorrect because the release of antidiuretic hormone (ADH) is regulated by factors such as osmolarity, blood volume & angiotensin II release.
Question 17:
Answer: E) It decreases the diameter of arteries, increasing vascular resistance and raising blood pressure.
Explanation: Arterial vasoconstriction refers to the narrowing of arteries, reducing their diameter. This process increases vascular resistance, making it more challenging for blood to flow through the narrowed arteries and ultimately raising blood pressure.
Option A is incorrect because arterial vasoconstriction decreases blood flow to the tissues, rather than increasing it.
Option B is incorrect because arterial vasoconstriction decreases the diameter of arteries, thereby increasing vascular resistance and raising blood pressure, rather than increasing their diameter.
Option C is incorrect because vasoconstriction typically occurs in arterioles to regulate blood flow, not in response to damaged vessels specifically. Constriction in damaged blood vessels can occur in both arteries & veins not just arteries.
Option D is incorrect because venous return to the heart is primarily enhanced by mechanisms such as skeletal muscle pump, respiratory pump, and venoconstriction, not arterial vasoconstriction.
Question 18:
Answer: B) It converts soluble fibrinogen into insoluble strands of fibrin.
Explanation: Thrombin is a key enzyme in the blood clotting process. Its primary role is to convert soluble fibrinogen, found in the blood plasma, into insoluble strands of fibrin. These fibrin strands form a meshwork that traps blood cells, leading to the formation of a stable blood clot. This process is essential for wound healing and preventing excessive bleeding.
Option A is incorrect because endothelin is what promotes vascular spasms.
Option C is incorrect because thrombin does not inhibit platelet activation; instead, it activates platelets and promotes their aggregation.
Option D is incorrect because while thrombin does promote platelet aggregation, this is not its primary role in blood clot formation. Platelet aggregation is triggered by ADP, Calcium, Serotonin & platelet derived growth factor.
Option E is incorrect because thrombin itself is formed from prothrombin and does not activate prothrombinase; rather, it acts downstream in the clotting cascade.
Question 19:
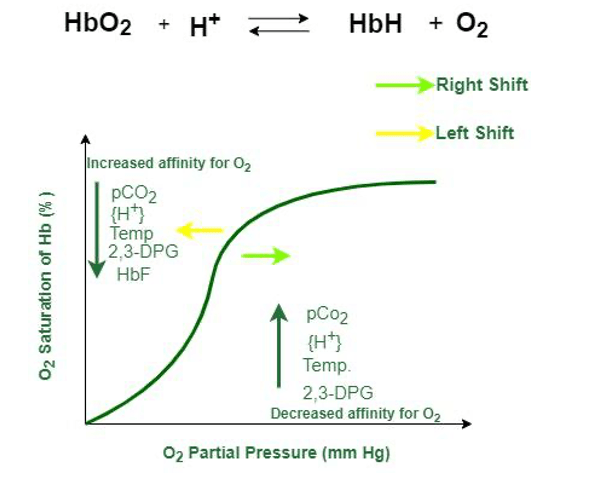
Answer: B) The curve depicts the relationship between oxygen saturation and partial pressure, influenced by factors like pH and temperature. It impacts oxygen unloading to tissues.
Explanation: The oxygen dissociation curve illustrates how the saturation of haemoglobin with oxygen is influenced by the partial pressure of oxygen in the blood. Factors such as pH and temperature can shift the curve, affecting how readily haemoglobin releases oxygen to tissues. A rightward shift indicates reduced oxygen affinity, promoting oxygen unloading to tissues, while a leftward shift indicates increased affinity, reducing oxygen release. This curve is crucial in understanding how the body adapts to varying oxygen demands in different tissues.
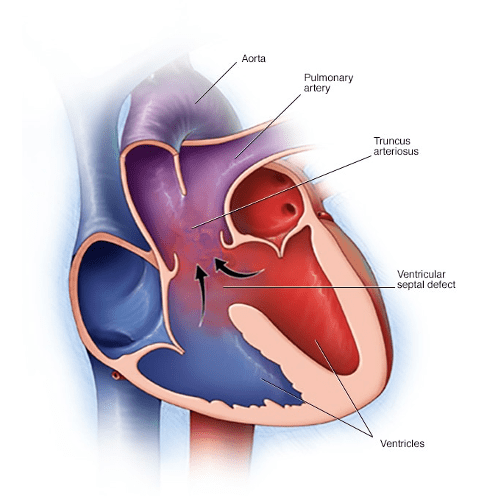
Question 20:
Answer: A) Closure of the ductus arteriosus, redirecting blood flow away from fetal pathways.
Explanation: During the transition from foetal to postnatal circulation, one key event is the closure of the ductus arteriosus. In foetal circulation, the ductus arteriosus allows blood to bypass the non-functioning foetal lungs. After birth, when the lungs begin functioning, this ductus closes to direct blood flow through the pulmonary circulation.
Option B is incorrect because the foramen ovale is a fetal anatomical feature that allows blood to bypass the pulmonary circulation by shunting blood from the right atrium to the left atrium. This shunt closes shortly after birth due to changes in pressure in the heart chambers and blood vessels.
Option C is incorrect because the umbilical vein is part of the fetal circulation that carries oxygenated blood from the placenta to the fetus. After birth, the umbilical vessels undergo closure and regress.
Option D is incorrect because the hepatic portal system is responsible for directing blood from the gastrointestinal tract to the liver for processing and detoxification. This system develops early in fetal life and does not undergo significant changes during the transition to postnatal circulation.
Option E is incorrect because the umbilical arteries carry deoxygenated blood from the fetus to the placenta during fetal life for exchange of gases and nutrients. After birth, these vessels undergo closure but do not direct blood to the internal iliac artery.
Question 21:
Answer: B) Increased pressure in the left atrium triggers its closure.
Explanation: The foramen ovale in fetal circulation allows blood to flow directly from the right atrium to the left atrium, bypassing the non-functional fetal lungs. After birth, as the baby takes its first breaths and the lungs expand, the pressure in the left atrium increases, causing the foramen ovale to close. This redirection of blood flow ensures that oxygenated blood is sent to the lungs for oxygenation.
Option A is incorrect because it is the increase in blood flow & pressure to the left atrium that triggers the closure of the foramen ovale, not blood flow in the lungs.
Option C is incorrect because elevated oxygen levels do not directly trigger the closure of the foramen ovale. Instead, the closure is primarily influenced by changes in pressure dynamics within the heart after birth.
Option D is incorrect because hormonal changes at birth such as a reduction in prostaglandin levels contribute to the closure of other fetal shunts like the ductus arteriosus & ductus venosus, but do not directly affect the closure of the foramen ovale.
Question 22:
Answer: B) It conducts impulses from the atria to the ventricles and is in the interventricular septum.
Explanation: The bundle of His is a vital part of the heart’s conduction system. It conducts electrical impulses from the atria to the ventricles, ensuring coordinated contraction. It is in the interventricular septum, a muscular wall that separates the left and right ventricles.
Option A is incorrect because the SA node initiates the heart’s electrical impulses not the bundle of His & is found in the right atrium.
Option C is incorrect because the bundle of His is not involved in regulating the heart’s response to sympathetic stimulation. This function is primarily carried out by the autonomic nervous system and specific receptors in the heart.
Option D is incorrect because controlling heart rate & rhythm is primarily controlled by the sinoatrial (SA) node & AV node.
Option E is incorrect because causing a delay in impulse transmission to allow the atria to fully empty into the ventricles is the role of the atrioventricular (AV) node.
Question 23:
Answer: C) Total blood volume
Explanation: Peripheral vascular resistance is primarily determined by three factors: vessel diameter, blood viscosity, and vessel length. Total blood volume, while important for overall circulatory function, is not directly related to peripheral vascular resistance.
Option A is incorrect because vessel diameter is directly related to peripheral vascular resistance. A smaller vessel diameter increases resistance, while a larger diameter decreases resistance.
Option B is incorrect because blood viscosity directly affects peripheral vascular resistance. Thicker blood (higher viscosity) increases resistance, while thinner blood (lower viscosity) decreases resistance.
Option D is incorrect because vessel length is directly related to peripheral vascular resistance. Longer vessels have more resistance, while shorter vessels have less resistance.
Option E is incorrect because blood vessel damage can lead to changes in the vessel wall, such as atherosclerosis, which directly impacts peripheral vascular resistance by altering the smoothness and diameter of the vessel lumen.
Question 24:
Answer: B) Troponin and tropomyosin allow myosin binding to actin, and increased calcium levels trigger muscle contraction.
Explanation: Troponin and tropomyosin work together to regulate cardiac muscle contraction. Normally, tropomyosin blocks the actin binding sites, preventing myosin attachment. When calcium levels rise, troponin binds to calcium, causing tropomyosin to move and expose the actin sites. This enables myosin to bind with actin, initiating muscle contraction. This precise control ensures the heart contracts effectively.
Option A is incorrect because increased calcium levels lead to muscle contraction, not relaxation. Troponin and tropomyosin block myosin binding sites, and when calcium levels increase, they shift to allow myosin binding and thus muscle contraction.
Option C is incorrect because troponin and tropomyosin do not break down myosin. Additionally, decreased calcium levels do not enhance muscle contraction; instead, they lead to muscle relaxation by preventing myosin binding to actin.
Option D is incorrect because troponin and tropomyosin are not involved in controlling heart rate. They are involved in regulating muscle contraction by controlling the access of myosin to actin binding sites in the presence of calcium.
Option E is incorrect because increased calcium levels result in muscle contraction, not relaxation. Troponin and tropomyosin block myosin binding sites, and increased calcium levels cause a shift that allows muscle contraction.

Question 25:
Answer: B) Calcium binds to troponin, causing tropomyosin to move and expose myosin binding sites on actin. The Na/K pump indirectly affects calcium levels by maintaining the sodium gradient necessary for the sodium-calcium exchanger to function.
Explanation: Calcium is a crucial regulator of cardiac muscle contraction. When calcium ions bind to troponin, it causes a conformational change that allows the myosin heads to interact with actin filaments. This interaction forms cross-bridges, leading to muscle contraction. The sodium-potassium pump (Na/K pump) helps maintain calcium gradients by actively transporting sodium out of and potassium into cardiac muscle cells, ensuring proper calcium levels for contraction and relaxation.
Option A is incorrect because calcium binds to troponin, not tropomyosin. Additionally, the Na/K pump does not directly remove calcium from the cytoplasm; it helps maintain the sodium gradient for the sodium-calcium exchanger, which removes calcium.
Option C is incorrect because calcium binds to troponin, not actin. The Na/K pump does not pump calcium into the sarcoplasmic reticulum; this is the role of the sarcoplasmic reticulum Ca²⁺-ATPase (SERCA).
Option D is incorrect because calcium binds to troponin, not myosin. The Na/K pump does not directly exchange calcium for sodium; this is done by the sodium-calcium exchanger (NCX), which relies on the gradient maintained by the Na/K pump.
Option E is incorrect because calcium binding to troponin causes tropomyosin to move and expose myosin binding sites, not inhibit them. The Na/K pump primarily maintains sodium and potassium gradients and does not directly control calcium influx.
Question 26:
Answer: C) Starling’s law states that increased preload results in increased stroke volume, enhancing cardiac output. It ensures optimal cardiac performance.
Explanation: Starling’s law describes the relationship between preload (the amount of blood in the ventricles before contraction) and stroke volume (the volume of blood ejected with each heartbeat). According to this law, an increase in preload leads to a more forceful contraction, resulting in an increased stroke volume. This mechanism ensures that the heart can adapt to changes in venous return, optimising cardiac output to meet the body’s demands.
Option A is incorrect because Starling’s law describes the relationship between preload and stroke volume, not heart rate and cardiac output. Preload impacts stroke volume, not heart rate.
Option B is incorrect because Starling’s law relates preload to stroke volume, not afterload, and it does not directly influence heart rate. Preload increases stroke volume, not contractility.
Option D is incorrect because Starling’s law does not indicate that afterload decreases stroke volume. Starling’s law specifically states that increased preload results in increased stroke volume. Preload and afterload are not inversely related.
Option E is incorrect because Starling’s law is directly related to stroke volume. It states that increased preload results in increased stroke volume, not that preload influences heart rate.
Question 27:
Answer: B) Adrenoreceptors promote calcium influx, enhancing heart rate and contractility. Sympathetic stimulation increases heart rate, while parasympathetic stimulation decreases heart rate.
Explanation: Adrenoreceptors, specifically beta-adrenergic receptors, stimulate calcium influx into cardiac muscle cells. This increased intracellular calcium enhances both heart rate and contractility. Sympathetic stimulation, often referred to as the “fight or flight” response, leads to increased heart rate and contractile force. In contrast, parasympathetic stimulation (vagal tone) decreases heart rate but has minimal impact on contractility.
Option A is incorrect because adrenoreceptors promote calcium influx, which enhances heart rate and contractility, not block it. Sympathetic stimulation increases heart rate, while parasympathetic stimulation decreases it.
Option C is incorrect because adrenoreceptors do affect calcium levels by promoting calcium influx. Sympathetic stimulation increases heart rate, while parasympathetic stimulation decreases it, not the other way around.
Option D is incorrect because adrenoreceptors do not inhibit calcium release from the sarcoplasmic reticulum; they promote calcium influx. Additionally, sympathetic stimulation increases heart rate, and parasympathetic stimulation does have an effect by decreasing heart rate.
Option E is incorrect because while adrenoreceptors do promote calcium influx, enhancing heart rate and contractility, parasympathetic stimulation decreases heart rate, but has no affect on contractility.
Question 28:
Answer: C) Claudication is due to inadequate arterial blood flow during exercise, causing muscle pain.
Explanation: Claudication is a symptom commonly associated with peripheral vascular disease (PVD). It occurs due to inadequate blood flow through the arteries to meet the oxygen demands of exercising muscles. This results in muscle pain or cramping during physical activity, as oxygen supply cannot keep up with demand. It is a hallmark sign of compromised arterial circulation, often affecting the legs.
Option A is incorrect because claudication is a result of inadequate arterial blood flow, not venous insufficiency. Venous insufficiency typically causes symptoms like swelling, heaviness, and skin changes, not exercise-induced leg pain.
Option B is incorrect because claudication is not caused by impaired lymphatic drainage. Impaired lymphatic drainage leads to oedema, characterised by swelling rather than exercise-induced muscle pain in the legs.
Option D is incorrect because claudication is related to peripheral arterial disease, not coronary artery stenosis. Coronary artery stenosis causes angina (chest pain), not claudication.
Option E is incorrect because claudication is characterised by muscle pain in the legs due to inadequate arterial blood flow, not chest pain. Chest pain is associated with cardiac conditions, not peripheral vascular disease.
Question 29:
Answer: E) Sinoatrial (SA) node cells
Explanation: Sinoatrial (SA) node cells, located in the right atrium of the heart, serve as the natural pacemakers of the heart. They generate electrical impulses that initiate each heartbeat by triggering atrial contraction. The SA node sets the rhythm for the entire heart.
Option A is incorrect because ventricular myocytes are responsible for the contraction of the ventricles.
Option B is incorrect because atrial myocytes are responsible for the contraction of the atria.
Option C is incorrect because Purkinje fibres conduct electrical impulses rapidly through the ventricles.
Option D is incorrect because the atrioventricular (AV) node helps to delay the electrical impulses before it passes to the ventricles. Although it can act as a pacemaker, it is not the primary pacemaker due to being slower than the SA node.
Question 30:
Answer: B) The T wave represents ventricular repolarisation & corresponds to stage 3 of myocardial action potential.
Explanation: The T wave in an electrocardiogram (ECG) represents ventricular repolarisation. It corresponds to the phase of the cardiac action potential when the ventricles are resetting their electrical state, preparing for the next contraction. This phase involves the recovery of ion channels and the restoration of the resting membrane potential in ventricular cells. Ventricular repolarisation corresponds to stage 3 of the myocardial action potential which involves repolarisation due to K+ efflux.
Option A is incorrect because the QRS complex represents ventricular depolarisation. Stage 2 of the myocardial action potential is the plateau phase which corresponds to ST segment of the ECG.
Option C is incorrect because, although the T wave represents ventricular repolarisation, it corresponds to stage 3 of the myocardial action potential, not stage 2.
Option D is incorrect because the T wave does not represent ventricular contraction; it represents repolarisation. Stage 2 of the myocardial action potential is the plateau phase and does not correspond to the T wave.
Option E is incorrect because the QRS complex represents contraction.

Question 31:
Answer: A) Haemoglobin’s affinity for oxygen decreases in acidic conditions and with increasing temperature, promoting oxygen unloading in metabolically active tissues. Carbon dioxide helps maintain proper pH.
Explanation: Haemoglobin’s affinity for oxygen decreases in response to increased acidity (decreased pH), higher temperatures & increased levels of 3-BPG. This phenomenon, known as the Bohr effect, promotes oxygen unloading in metabolically active tissues where oxygen is needed. Additionally, carbon dioxide indirectly plays a role by forming bicarbonate ions, which help buffer the blood and maintain a stable pH, further facilitating oxygen release. Increased pH (alkaline levels), decreased CO2 levels, decreased temperature & decreased levels of 3-BPG all increase haemoglobin’s affinity to oxygen decreasing unloading of oxygen. This phenomenon is known as the Haldane effect & occurs at the lungs. It promotes carbon dioxide dissociation from haemoglobin to replace it with oxygen.
Question 32:
Answer: B) MAP is mainly determined by diastolic pressure, with systolic pressure reflecting vascular resistance. MAP accounts for both cardiac output and vascular resistance, offering a better assessment of perfusion.
Explanation: Mean Arterial Pressure (MAP) is primarily determined by diastolic pressure and is a weighted average of systolic and diastolic pressures. It is considered clinically valuable because it accounts for both cardiac output (systolic pressure) and vascular resistance (diastolic pressure), providing a more comprehensive assessment of overall perfusion pressure, which is vital for organ function. MAP = DP + 1/3(SP-DP) or (2DP + SP)/3
Option A is incorrect because MAP is influenced by both cardiac output and systemic vascular resistance, not by heart rate alone. Systolic and diastolic pressures are related to cardiac output and vascular resistance, respectively.
Option C is incorrect because MAP is not dependent on blood viscosity, and systolic pressure relates to cardiac output and arterial pressure, not just arterial elasticity.
Option D is incorrect because MAP is influenced by cardiac output and systemic vascular resistance, not just venous return. Systolic and diastolic pressures indicate arterial pressure during contraction and relaxation of the heart.
Option E is incorrect because MAP is not determined by the carotid sinus. It is influenced by cardiac output and systemic vascular resistance and provides a better indication of tissue perfusion than systolic or diastolic pressure alone.
Question 33:
Answer: B) The PR interval reflects atrial depolarisation and the delay at the AV node, allowing the ventricles to fill.
Explanation: The PR interval on an ECG represents the time from atrial depolarisation (P wave) to the onset of ventricular depolarisation (QRS complex). During this interval, there is a deliberate delay at the atrioventricular (AV) node, allowing the ventricles to fill with blood from the atria before contracting. This delay ensures efficient and coordinated pumping of blood.
Option A is incorrect because the PR interval does not include ventricular depolarisation; it ends just before it starts.
Option C is incorrect because the PR interval ends before the QRS complex begins. The QRS complex indicates ventricular depolarisation.
Option D is incorrect because the PR interval represents the electrical delay at the AV node, not the physical movement of blood from the atria to the ventricles.
Option E is incorrect because the PR interval represents electrical activity, not mechanical events like isovolumetric contraction.
Question 34:
Answer: A) The ductus venosus allows oxygen-rich blood from the umbilical vein to bypass the liver and flow directly into the inferior vena cava.
Explanation: The ductus venosus is a fetal blood vessel that shunts a portion of oxygenated blood from the umbilical vein directly to the inferior vena cava, bypassing the liver. This allows a significant amount of oxygen-rich blood to reach the heart and be pumped to the rest of the body, ensuring that vital organs receive adequate oxygenation. This bypass is crucial because the fetal liver is not fully functional and does not need as much oxygen. This mechanism ensures that oxygenated blood is efficiently used by more critical organs.
Option B is incorrect because the foramen ovale shunts blood between the right atrium and the left atrium.
Option C is incorrect because the ductus arteriosus diverts blood from the pulmonary artery to the aorta.
Option D is incorrect because the umbilical artery carries deoxygenated blood from the fetus to the placenta, while the ductus venosus allows oxygenated blood from the umbilical vein to bypass the liver.
Option E is incorrect because the ductus venosus does not deal with oxygen-poor blood or the superior vena cava. It carries oxygen-rich blood from the umbilical vein to the inferior vena cava, bypassing the liver.
Question 35:
Answer: C) Preload
Explanation: Preload is the primary determinant of stroke volume. It represents the amount of blood that fills the ventricles during diastole (ventricular relaxation). An increase in preload, often due to an increase in venous return to the heart, leads to a greater stretch of the ventricular muscle fibres, resulting in a more forceful contraction and a higher stroke volume.
Option A is incorrect because blood pressure, although important, is not the primary determinant of stroke volume. Blood pressure is more a result of cardiac output and peripheral resistance than a direct influence on stroke volume.
Option B is incorrect because heart rate primarily affects cardiac output (the product of stroke volume and heart rate) rather than stroke volume directly. An increase in heart rate can decrease stroke volume if it shortens the diastolic filling time.
Option D is incorrect because afterload is the resistance the heart must overcome to eject blood. While it influences stroke volume, it is not the primary determinant. Increased afterload generally decreases stroke volume by making it harder for the heart to eject blood.
Option E is incorrect because contractility, the inherent strength of the heart’s contraction, influences stroke volume but is not the primary determinant. Preload has a more direct and consistent effect on stroke volume through the Frank-Starling mechanism.
Question 36:
Answer: C) Sympathetic stimulation decreases the duration of contraction of the heart by releasing noradrenaline.
Explanation: The sympathetic nervous system, activated during the “fight or flight” response, increases heart rate and the strength of contraction (inotropy) by releasing norepinephrine (noradrenaline). Norepinephrine acts on beta-adrenergic receptors in the heart, leading to increased depolarisation in the pacemaker cells of the sinoatrial (SA) node, which accelerates heart rate. Additionally, norepinephrine stimulates the phosphorylation of contractile proteins, including phospholamban, which enhances the reuptake of calcium ions into the sarcoplasmic reticulum (SR) via the SERCA pump. This action speeds up relaxation and prepares the heart for subsequent contractions. Noradrenaline also increases calcium influx into contractile cells (by phosphorylating ryanodine & L-type channels).
Option A is incorrect because acetylcholine is predominantly associated with the parasympathetic nervous system, where it slows heart rate by hyperpolarising the SA node and reducing its firing rate.
Option B is incorrect because sympathetic stimulation increases the speed of calcium reuptake into the sarcoplasmic reticulum via phosphorylation of phospholamban, which enhances SERCA pump activity. This action facilitates faster relaxation.
Option D is incorrect because sympathetic stimulation increases the strength of contraction (ionotropy) but decreases the length of contraction since the speed of electrical transmission through the heart (dromotropy) & heart rate (chronotropy) are faster & more frequent.
Question 37:
Answer: C) Myoglobin primarily stores oxygen in muscle tissues and is predominantly found in skeletal muscles.
Explanation: Myoglobin is a protein found in muscle tissues, particularly in skeletal muscles. Its primary role is to store oxygen within muscle cells. This stored oxygen can be readily released when the muscles require it during periods of increased activity.
Option A is incorrect because structural proteins in cardiac muscle cells include titin, myosin, actin, and others that are essential for muscle contraction.
Option B is incorrect because haemoglobin is the main oxygen carrier in the blood.
Option D is correct however it is not the main function of myoglobin.
Question 38:
Answer: C) Tunica media
Explanation: The tunica media is the middle layer of blood vessel walls and consists of smooth muscle fibres. This layer directly influences vascular resistance by contracting or relaxing. Contraction of the smooth muscle in the tunica media narrows the blood vessel (vasoconstriction), increasing vascular resistance. Relaxation of the smooth muscle widens the vessel (vasodilation), reducing vascular resistance.
Option A & D are incorrect because the tunica adventitia aka tunica externa, is the outermost layer of blood vessel walls primarily composed of connective tissue & collagen that provides structural support and protection.
Option B is incorrect because tunica intima is the innermost layer of blood vessel walls composed of endothelial cells and a thin layer of connective tissue. Its primary function is to provide a smooth surface for blood flow and regulate vascular permeability, not to regulate vascular resistance.
Option E is incorrect because tunica albuginea refers to the dense connective tissue layer surrounding the testes.
Question 39:
Answer: C) M2 – Muscarinic acetylcholine receptors
Explanation: M2 muscarinic acetylcholine receptors are primarily responsible for mediating the effects of the parasympathetic nervous system on the heart. When acetylcholine binds to M2 receptors in the heart (particularly in the sinoatrial node and atria), it leads to decreased heart rate (negative chronotropy). This pathway is a Gi pathway which decreases the formation of Protein Kinase A thus decreasing phosphorylation of proteins.
Option A is incorrect because alpha-1 adrenergic receptors cause vasoconstriction in blood vessels.
Option B is incorrect becasue beta-1 adrenergic receptors are responsible for mediating the effects of the sympathetic nervous system on the heart, leading to increased heart rate and contractility.
Option D is incorrect because M3 – Muscarinic acetylcholine receptors are primarily found in the enteric nervous system (specifically in smooth muscle cells) and mediate effects such as smooth muscle contraction and glandular secretion.
Option E is incorrect because beta-2 adrenergic receptors are mainly found in smooth muscle cells of bronchioles and blood vessels, where they mediate vasodilation and bronchodilation.
Question 40:
Answer: D) Preload is the volume of blood in the ventricles at the end of diastole, and an increase in preload generally leads to an increase in stroke volume.
Explanation: Preload is the degree of stretch of the ventricular muscle fibres at the end of diastole, just before ventricular contraction (systole). An increase in preload, often due to increased venous return, leads to greater stretching of the ventricles. This increased stretch results in a more forceful ventricular contraction, leading to an increase in stroke volume (the amount of blood ejected by the ventricle with each beat). Preload primarily influences the end-diastolic volume (EDV), which affects stroke volume through the Frank-Starling mechanism.
Option B is incorrect because the force exerted by the left ventricle during contraction is more closely related to afterload, which is the resistance the ventricles must overcome to eject blood into the systemic circulation.
Option C is incorrect because the resistance against which the ventricles pump is related to afterload, not preload. Afterload is influenced by factors such as systemic vascular resistance.
Option E is incorrect because preload itself does not directly increase the contractility of the ventricles. Instead, it influences stroke volume through the degree of myocardial fibre stretch and the subsequent force of contraction.
Question 41:
Answer: b) A fetal blood vessel that connects the pulmonary artery to the aorta, allowing blood to bypass the fetal lungs & becomes ligamentum arteriosum.
The ductus arteriosus is a fetal blood vessel that creates a direct connection between the pulmonary artery and the aorta in the developing fetus. This connection serves the vital function of bypassing the non-functional fetal lungs as there is high resistance to blood flow in lungs. This closes after birth allowing blood flow to lungs.
Option D is incorrect because it describes the function of the umbilical veins, not the ductus arteriosus.
Option E is incorrect because it the ligamentum arteriosum is the post-natal remnant, not the ductus arteriosus itself.
Question 42:
Answer: C) To promote fluid reabsorption from interstitial fluid back into venule end of capillaries.
Explanation: Oncotic pressure (colloid osmotic pressure) primarily functions to regulate the movement of fluid between the blood and surrounding tissues. It is created by the presence of large, non-diffusible proteins such as plasma proteins (albumin). This pressure helps draw fluid back into the capillaries and prevents excessive fluid loss from the bloodstream into the interstitial spaces.
Option A is incorrect because oncotic pressure primarily promotes fluid reabsorption from the interstitial fluid back into the venule end of capillaries, rather than promoting fluid filtration out of capillaries.
Option B is incorrect because the maintenance of blood pressure by constricting blood vessels is regulated by mechanisms involving arterial smooth muscle and the sympathetic nervous system,
Option D is incorrect because hydrostatic pressure due to ventricular contraction promotes fluid release from the arteriole end of capillaries.
Option E is incorrect because oncotic pressure primarily affects the movement of fluids, not the reabsorption of proteins into veins. Proteins generally are too big to be able to cross the membranes of capillaries, arteries or veins.
Question 43:
Answer: C) Chemoreceptors
Explanation: Option A is incorrect because mechanoreceptors primarily detect mechanical changes such as pressure or stretch in blood vessels or heart chambers, rather than changes in pH or gas concentrations.
Option B is incorrect because the carotid sinus receptors is the main detector of changes in blood pressure around the body.
Option D is incorrect because baroreceptors primarily detect changes in blood pressure, not changes in pH, oxygen saturation, or carbon dioxide concentration.
Option E is incorrect because aortic sinus receptors is the primarily detector of changes in blood pressure in the heart.
Question 44:
Answer: B) The pressure in the arteries during ventricular contraction.
Explanation: Systolic blood pressure is the pressure in the arteries during ventricular contraction (systole). It is the higher of the two values typically reported in blood pressure measurements (e.g., 120/80 mm Hg), representing the maximum pressure exerted by the heart as it pumps blood into the arteries.
Option A is incorrect because the pressure in the arteries during ventricular relaxation is known as diastolic blood pressure.
Option C is incorrect because the pressure in the atria during diastole is atrial pressure.
Option D is incorrect because the pressure in the veins during ventricular relaxation is venous pressure.
Question 45:
Answer: A) Erythrocytes (Red blood cells)
Explanation: Erythrocytes, or red blood cells, are primarily responsible for oxygen transport from the lungs to body tissues. They contain the protein haemoglobin, which binds to oxygen in the lungs and releases it in the tissues where oxygen is needed for metabolism.
Option B is incorrect because leukocytes are primarily involved in immune responses.
Option C is incorrect because megakaryocytes are responsible for producing platelets, which are involved in blood clotting.
Option D is incorrect because erythropoietin is a hormone produced by the kidneys that stimulates red blood cell production in bone marrow, but it does not directly transport oxygen.
Option E is incorrect because reticulocytes are immature red blood cells that eventually mature into erythrocytes, which then transport oxygen. Reticulocytes themselves do not transport oxygen.
Question 46:
Answer: D) Purkinje fibres
Explanation: The coordinated contraction of the ventricles is ensured by the purkinje fibres. Electrical stimulation begins in the SA node which conducts electrical impulses to the atrioventricular (AV) node, & from there to the Bundle of His. Bundle of His spreads electrical impulses to the right & left bundle branches (that pass through each ventricle) & then to Purkinje fibres, which then stimulate the ventricular muscle cells to contract simultaneously.
Option A is incorrect because the sinoatrial (SA) node is responsible for initiating the electrical impulse that starts each heartbeat by generating action potentials.
Option B is incorrect because the atrioventricular (AV) node is responsible for delaying the electrical impulse to allow the atria to contract fully before the ventricles are activated.
Option C is incorrect because the moderator band (septomarginal trabeculae) is a structure in the right ventricle that binds to the anterior papillary muscle ensuring that papillary muscles contract to close AV valves before ventricular contraction.
Option E is incorrect because the bundle of His (AV bundle) is responsible for transmitting the electrical impulse from the AV node to the Purkinje fibbers and then to the ventricles, but it alone does not ensure the coordinated contraction of the ventricles.
Question 47:
Answer: A) To conduct action potentials deep into the muscle fibre (allow calcium ions to enter cardiomyocytes promoting their release from the sarcoplasmic reticulum).
Explanation: T-tubules are invaginations of the sarcolemma (muscle cell membrane) that penetrate deep into the muscle fibre. Their primary function is to conduct action potentials (electrical impulses) rapidly from the cell surface to the interior of the muscle fibre. This action potential propagation allows for the synchronous depolarisation of the T-tubule membrane and the adjacent sarcoplasmic reticulum (SR), which is the intracellular calcium store. The depolarisation of the T-tubule membrane triggers the opening of calcium release channels (ryanodine receptors) on the SR, leading to the release of calcium ions into the cytoplasm. These calcium ions then bind to troponin on the actin filaments, allowing for the initiation of muscle contraction.
Option B is incorrect because T-tubules do not block myosin-binding sites on actin molecules; rather, they facilitate muscle contraction by promoting calcium release.
Option C is incorrect because the sarcoplasmic reticulum stores calcium ions.
Option D is incorrect because anchoring myosin filaments to the Z-disc is a function of titin and other structural proteins within the sarcomere.
Option e) is incorrect because T-tubules do not have enzymatic activity for ATP breakdown; this function is primarily carried out by ATPase enzymes associated with myosin heads during muscle contraction.
Question 48:
Answer: B) Thrombin converts fibrinogen into fibrin and is inhibited by plasmin.
Explanation: Thrombin is an enzyme that converts soluble fibrinogen into insoluble strands of fibrin, leading to the formation of a blood clot. Plasmin, on the other hand, is an enzyme that breaks down fibrin clots and, in turn, regulates the activity of thrombin.
Option A is incorrect because thrombin activates Factor XIII to cross-link fibrin, not Factor X, and its activity is primarily inhibited by antithrombin III.
Option C is incorrect because thrombin activates platelets by cleaving protease-activated receptors (PARs) on their surface, and its activity is not enhanced by heparin but rather inhibited by it through binding to antithrombin III.
Option D is incorrect because thrombin promotes clot formation by converting fibrinogen to fibrin. Protein C inhibits thrombin’s activity by inactivating factors Va and VIIIa, thus downregulating the coagulation cascade.
Option E is incorrect because thrombin converts fibrinogen into fibrin, not the reverse, and it is not promoted by plasmin, instead it is inhibited because plasmin degrades fibrin, leading to fibrinolysis.
Question 49:
Answer: A) To activate Factor VII.
Explanation: Tissue factor (Factor III) initiates the extrinsic pathway of the coagulation cascade by forming a complex with Factor VII, which activates Factor X. This is a critical step in the coagulation process.
Option B is incorrect because tissue factor does not directly activate Factor X. Factor X is activated downstream in the cascade after the formation of the tissue factor-Factor VIIa complex.
Option C is incorrect because tissue factor does not activate thrombin directly. Thrombin is generated later in the cascade through the action of Factor Xa and prothrombinase.
Option D is incorrect because Factor IX is primarily activated in the intrinsic pathway of the coagulation cascade.
Option E is incorrect because Factor XII is involved in the initiation of the intrinsic pathway of coagulation and is activated by contact exposed collagen.
Question 50:
Answer: A) vWF enhances platelet adhesion to exposed collagen.
Explanation: Von Willebrand factor (vWF) is crucial for haemostasis and circulates the blood complexed to Factor VIII. It acts by promoting the adhesion of platelets to exposed collagen via GP 1a/2a at sites of vascular injury, initiating a complex that binds to fibrinogen.
Option B is incorrect because vWF promotes platelet adhesion and aggregation.
Option C is incorrect because vWF does not activate thrombin. Thrombin activation occurs in the coagulation cascade.
Option D is incorrect because vWF indirectly stimulates platelet aggregation. Once platelets bind to exposed collagen with the help of vWF, platelets become activated & release compounds such as serotonin, calcium, thromboxane A2, ADP & platelet derived growth factor. This factors then stimulate platelet aggregation.
Option E is incorrect because vWF does not activate antithrombin. Antithrombin is a protease inhibitor that regulates thrombin and other coagulation factors.
Question 51:
Answer: B) Factors II, VII, IX, and X
Explanation: Vitamin K is essential for the synthesis of specific clotting factors in the liver, including Factors II (prothrombin), VII, IX, and X. These factors are vital for the coagulation process and help ensure that blood clots can form effectively when needed.
Question 52:
Answer: A) Thrombin
Explanation: Thrombin is the central enzyme in the common pathway of the coagulation cascade. It plays a pivotal role by converting soluble fibrinogen into insoluble strands of fibrin. This fibrin meshwork forms the structural basis of a stable blood clot.
Option B is incorrect because Factor X is involved earlier in the cascade to activate thrombin.
Option C is incorrect because Factor IX is part of the intrinsic pathway not common and is involved in activating Factor X.
Option D is incorrect because tissue plasminogen activator (tPA) is involved in fibrinolysis.
Option E is incorrect because prothrombinase is involved in converting prothrombin (Factor II) to thrombin, not in the conversion of fibrinogen to fibrin.
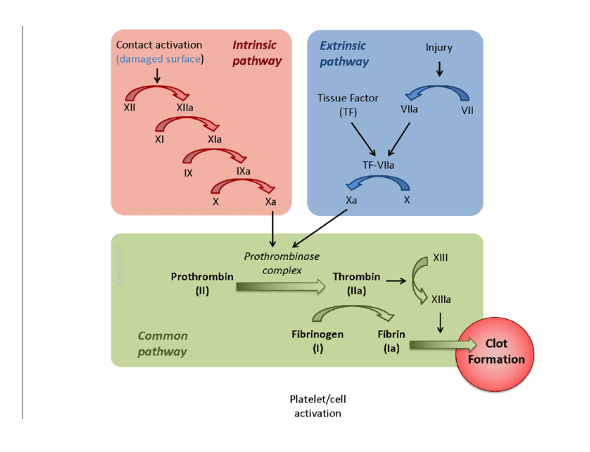
Question 53:
Answer: B) Endothelial cells
Explanation: The extrinsic pathway of the coagulation cascade is initiated by the release of tissue factor (Factor III) from damaged endothelial cells lining blood vessels. Tissue factor is essential for the activation of this pathway and the subsequent formation of a blood clot.
Option A is incorrect because platelets primarily release factors involved in platelet aggregation, not tissue factor.
Option C is incorrect because blood plasma contains various coagulation factors but not tissue factor.
Option D is incorrect because the liver synthesises clotting factors but does not release tissue factor.
Option E is incorrect because exposed collagen activates platelets and triggers the intrinsic pathway, not the extrinsic pathway initiated by tissue factor from endothelial cells.
Question 54:
Answer: A) ADP enhances platelet aggregation by activating P2/Y12 receptors.
Explanation: When platelets are activated, they release ADP (adenosine diphosphate), which acts as a signalling molecule triggered by the P2/Y12 receptor. ADP encourages nearby platelets to become activated, leading to platelet aggregation. This process is crucial for the formation of a stable blood clot at the site of vascular injury.
Option A is incorrect because ADP enhances aggregation by activating specific receptors.
Option B is incorrect because ADP does not directly activate GPIIb/IIIa receptors. These receptors are activated by other pathways involving fibrinogen binding.
Option C is incorrect because Von Willebrand factor primarily promotes platelet adhesion to exposed collagen which then triggers platelet aggregation as a result.
Option D is incorrect because ADP does not directly enhance the activity of tissue factor. Tissue factor plays a role in the initiation of the coagulation cascade, not in platelet aggregation.
Question 55:
Answer: D) Thromboxane A2 activates P2Y12 receptors on platelets, amplifying platelet aggregation.
Explanation: Thromboxane A2 plays a crucial role in haemostasis by promoting platelet aggregation and vasoconstriction. When platelets are activated, they release thromboxane A2, which amplifies platelet aggregation through the activation of P2Y12 receptors on platelets. This process enhances the recruitment and activation of additional platelets, forming a stable blood clot at the site of vascular injury.
Option A is incorrect because thromboxane A2 does not promote endothelial cell repair and angiogenesis. These processes are primarily regulated by other factors such as vascular endothelial growth factor (VEGF).
Option B is incorrect because thromboxane A2 does promote vasoconstriction by inhibiting prostacyclin synthesis, not the other way around. Prostacyclin (PGI2) is an inhibitor of platelet aggregation and a vasodilator.
Option C is incorrect because thromboxane A2 does not enhance the release of tissue plasminogen activator (tPA), which facilitates clot dissolution. Thromboxane A2 promotes clot formation rather than dissolution.
Option E is incorrect because thromboxane A2 does not bind to Factor VIII to enhance the intrinsic pathway of coagulation. Factor VIII is involved in the intrinsic pathway primarily regulated by other factors like Factor IX and Factor X.
Question 56:
Answer: E) Heparin enhances production of antithrombin-III decreasing coagulation whereas aspirin reduces production of thromboxane A2 decreasing platelet aggregation.
Explanation: Heparin and aspirin are both used to prevent abnormal blood clot formation, but they work through different mechanisms. Heparin enhances the activity of antithrombin III, which inhibits several key enzymes in the coagulation cascade mainly thrombin, thus decreasing coagulation. On the other hand, aspirin inhibits the enzyme cyclooxygenase (COX), which in turn reduces the production of thromboxane A2. Thromboxane A2 is a promoter of platelet aggregation; therefore, by reducing its production, aspirin decreases platelet aggregation.
Option B is incorrect because, while aspirin does inhibit platelet aggregation (stage 2 of haemostasis), heparin primarily works by inhibiting coagulation (stage 3 of haemostasis) through the enhancement of antithrombin III activity, not by inhibiting platelet aggregation directly.
Question 57:
Answer: C) Protein C promotes fibrinolysis by stimulating the production of plasmin.
Explanation: Protein C is a critical component in the regulation of blood clotting and anticoagulation. When activated (by thrombomodulin), it inactivates Factors Va and VIIIa, reducing thrombin generation and thereby decreasing clot formation. Furthermore, Protein C indirectly promotes fibrinolysis by enhancing the conversion of plasminogen to plasmin, which breaks down fibrin clots.
Option A is incorrect because aspirin inhibits the production of thromboxane A2. Thromboxane A2 is involved in promoting platelet aggregation and vasoconstriction.
Option B is incorrect because Protein C does not enhance the activation of Factor VIII. Instead, it inactivates Factor VIIIa, thus reducing clot formation.
Option D is incorrect because Protein C does not inhibit platelet aggregation by producing prostacyclin. Prostacyclin is produced by endothelial cells and functions as a vasodilator and inhibitor of platelet aggregation.
Option E is incorrect because Protein C does not promote the formation of alpha-2-macroglobulin. Alpha-2-macroglobulin is a protease inhibitor that inhibits a variety of proteases but is not directly influenced by Protein C in the context of coagulation.
Question 58:
Answer: D) Celiac trunk.
Explanation: The celiac trunk, arising directly from the abdominal aorta, stands as a pivotal arterial conduit in abdominal vascular anatomy. Its primary mission is to channel oxygenated blood to a cluster of vital abdominal organs, comprising the liver, stomach, spleen, and even portions of the pancreas.
Option A is incorrect because the right subclavian artery supplies blood to the right arm and portions of the brain and spinal cord.
Option B is incorrect because the common carotid artery supplies blood to the head and neck regions.
Option C is incorrect because the inferior mesenteric artery supplies blood to the large intestine (last ¼ of transverse colon, descending colon, sigmoid colon, and rectum).
Option E is incorrect because the superior mesenteric artery supplies blood to the majority of the small intestine and part of the large intestine.

Question 59:
Answer: B) Converting fibrinogen into fibrin
Explanation: Thrombin (produced in the common pathway of the coagulation cascade), is a critical enzyme that primarily functions by converting fibrinogen into fibrin. This conversion is essential for the formation of a stable blood clot, as fibrin strands create a mesh that traps blood cells and solidifies the clot at the site of injury.
Option A is incorrect because thrombin does not activate Factor X; rather, Factor X is upstream of thrombin in the coagulation cascade and helps to generate thrombin.
Option C is incorrect because, while thrombin does promote platelet aggregation, this is not its primary role in the coagulation cascade.
Option D is incorrect because thrombin does not directly synthesize fibrin clots; it converts fibrinogen to fibrin, which then forms the basis of the clot.
Option E is incorrect because thrombin does not activate plasminogen. Plasminogen is activated by tissue plasminogen activator (tPA) to form plasmin, which breaks down clots.
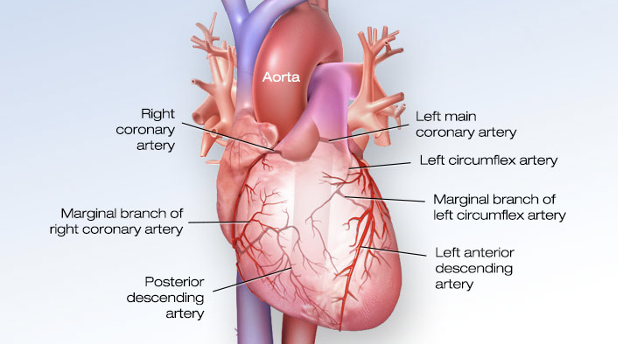
Question 60:
Answer: E) Right coronary artery (RCA)
Explanation: The posterior descending artery (PDA) is a branch of the right coronary artery (RCA). It supplies the posterior part of the heart with oxygenated blood.
Option A is incorrect because the left anterior descending artery (LAD) supplies the anterior wall of the left ventricle and the interventricular septum & is a branch of the left coronary artery.
Option B is incorrect because the left coronary artery (LCA) typically bifurcates into the LAD and the left circumflex artery (LCx), neither of which directly give rise to the PDA.
Option C is incorrect because the left circumflex artery (LCx) supplies the lateral and posterior walls of the left ventricle.
Option D is incorrect because the right marginal artery is a branch of the RCA, but it supplies the lateral part of the right ventricle, not the PDA.
Question 61:
Answer: A) Pericardium
Explanation: The pericardium is the membrane that surrounds the heart and anchors it within the mediastinum, the central compartment of the chest.
Option B is incorrect because the pleura is the membrane that surrounds the lungs.
Option C is incorrect because the myocardium is the muscular middle layer of the heart wall responsible for contraction.
Option D is incorrect because the endocardium is the inner lining of the heart chambers and valves.
Option E is incorrect because the epicardium is the outer layer of the heart wall, which is also the visceral layer of the serous pericardium but does not encompass the entire protective sac around the heart like the pericardium does.
Question 62:
Answer: B) Right atrium
Explanation: The coronary sinus is a venous structure that drains deoxygenated blood from the heart’s coronary veins. It empties into the right atrium of the heart, allowing for the return of this blood to the heart’s circulation.

Question 63:
Answer: B) Papillary muscles
Explanation: Papillary muscles are small, finger-like projections on the inner lining of the heart’s ventricles. Their primary function is to prevent backflow of blood into the atria by anchoring the chordae tendineae, which are thin, fibrous cords that attach to the atrioventricular (AV) valves.
Option A is incorrect because pectinate muscles are located in the atria and do not play a role in preventing backflow in the ventricles.
Option C is incorrect because chordae tendineae are tendinous cords that connect the papillary muscles to the atrioventricular valves, assisting in valve function but not being the primary structure that prevents backflow.
Option D is incorrect because the moderator band is a muscular band of heart tissue found in the right ventricle only that helps with the conduction of electrical signals. It supplies the anterior papillary muscle so that they contract & close the AV valves before the ventricles contract (preventing blood flow back into the atria).
Option E is incorrect because trabeculae carneae are irregular muscular columns on the inner surface of the ventricles, which assist in contraction.
Question 64:
Answer: E) Left anterior descending artery (LAD)
Explanation: The anterior interventricular sulcus is a groove on the heart’s surface that marks the course of the left anterior descending artery (LAD), also known as the anterior interventricular artery. This coronary artery supplies oxygenated blood to the anterior part of the interventricular septum and a portion of the left ventricle.
Interventricular = between the right & left ventricles.

Question 65:
Answer: B) Right coronary artery (RCA)
Explanation: The sinoatrial (SA) node of the heart, is most supplied by the right coronary artery (RCA) in 60% of people whilst it is supplied by LCx in the other 40%. The AV node of the heart is supplied by the right coronary artery (RCA) in 90% of people & by the left circumflex artery in 10% of people.
Question 66:
Answer: B) To facilitate electrical communication between cardiac muscle cells
Explanation: Intercalated discs are specialized structures found in cardiac muscle tissue. They play a key role in facilitating electrical communication between adjacent cardiac muscle cells, allowing for synchronised contraction of the heart. These discs contain gap junctions and desmosomes, which allow for the synchronised contraction of the heart muscle by permitting the direct transmission of action potentials from one cell to another. The passage of ions such as sodium (Na+), potassium (K+), calcium (Ca2+), and chloride (Cl-) through these gap junctions allows for rapid and coordinated depolarisation and repolarisation of adjacent cardiac muscle cells.
Option A is incorrect because glucose is primarily stored in the liver, muscle & adipose tissue as glycogen.
Option C is incorrect because while calcium ions do play a crucial role in cardiac muscle contraction, the intercalated discs are specifically involved in electrical communication, not the passage of calcium ions.
Option D is incorrect because generating ATP through oxidative phosphorylation occurs in the mitochondria.
Option E is incorrect because the passage of sodium ions occurs through ion channels in the cell membrane, not specifically through intercalated discs, which are more involved in electrical connectivity.
Question 67:
Answer: B) Sinus venosus
Explanation: The smooth-walled part of the right atrium, including the openings of the superior and inferior vena cava, develops from the embryonic structure known as the sinus venosus. This transformation occurs during heart development.
Option A is incorrect because the bulbus cordis develops into the right ventricle outflow tract and contributes to the formation of the smooth-walled part of the right ventricle.
Option C is incorrect because the truncus arteriosus gives rise to the aorta and pulmonary trunk.
Option D is incorrect because the infundibulum refers to the smooth pouch forming the outflow tract of the right ventricle.
Option E is incorrect because the septomarginal trabecula (moderator band) is a muscular band in the right ventricle, not part of the right atrium developmentally.
Question 68:
Answer: D) To shunt blood from the umbilical vein to the inferior vena cava bypassing the liver
Explanation: The ductus venosus is a fetal shunt that directs oxygenated blood from the umbilical vein directly into the inferior vena cava, bypassing the fetal liver. This allows oxygenated blood to reach the fetal heart and brain efficiently.
Option A is incorrect because the shunting of blood from the right atrium to the left atrium bypassing the lungs occurs through the foramen ovale.
Option B is incorrect because the shunting of blood from the pulmonary artery to the aorta bypassing the lungs occurs through the ductus arteriosus.
Option E is incorrect because blood is shunted from the umbilical vein to the inferior vena cava not superior vena cava.
Question 69:
Answer: A) The aorta and pulmonary trunk
Explanation: During heart development, a critical transformation takes place during weeks 4 to 8 of gestation. The truncus arteriosus, an early embryonic structure, undergoes a remarkable change, ultimately giving rise to two major adult structures: the aorta, which directs oxygen-rich blood to the body, and the pulmonary trunk, responsible for channelling oxygen-poor blood to the lungs.
Question 70:
Answer: D) Vasa vasorum.
Explanation: Vasa vasorum are tiny blood vessels that supply oxygen and nutrients to the walls of larger arteries and veins as they are too large for diffusion to give them enough nutrients. They ensure that the walls of these larger vessels receive the necessary nourishment for their function and maintenance.
Option A is incorrect because coronary arteries specifically supply oxygenated blood to the heart muscle itself.
Option B is incorrect because capillaries are the smallest blood vessels where gas exchange occurs between blood and tissues.
Option C is incorrect because pulmonary arteries carry deoxygenated blood from the heart to the lungs.
Option E is incorrect because arterioles are small arteries that regulate blood flow into capillary beds.

Question 71:
Answer: D) Phospholamban inhibits SERCA pump resulting in a decreased reuptake of calcium ions, thereby reducing the frequency of muscle contraction.
Explanation: Phospholamban is a regulatory protein found in muscle cells, especially cardiac muscle cells. Its primary function is to inhibit the SERCA (Sarco/Endoplasmic Reticulum Calcium ATPase) pump, which normally transports calcium ions from the cytoplasm back into the sarcoplasmic reticulum (SR) during muscle relaxation. By inhibiting the SERCA pump, phospholamban decreases the reuptake of calcium ions into the SR, thereby affecting the frequency of muscle contractions. When the heart is stimulated by the sympathetic nervous system (noradrenaline), the formation of Protein Kinase A phosphorylates phospholamban, thus inhibiting it. This allows the SERCA pump to function much quicker allowing for faster reuptake of calcium ions, more rapid relaxation of the heart & therefore increased contractions.
Option A is incorrect because phospholamban does not directly facilitate muscle contraction by enabling calcium to bind to troponin C. Calcium binding to troponin C is a separate process involved in initiating muscle contraction.
Option B is incorrect because sarcoplasmic reticulum stores calcium ions.
Option C is incorrect because phospholamban inhibits, rather than regulates, the calcium ion transport within muscle cells.
Option E is incorrect because phospholamban inhibits, rather than stimulates, the SERCA pump.
Question 72:
Answer: A) Phase 0
Explanation: In the cardiac action potential, phase 0 corresponds to the rapid depolarisation of the cell membrane. During this phase, there is a rapid influx of sodium ions into the cell, leading to a reversal of the membrane potential and the initiation of an action potential. This phase is critical for the initiation of muscle cell contraction in the heart.
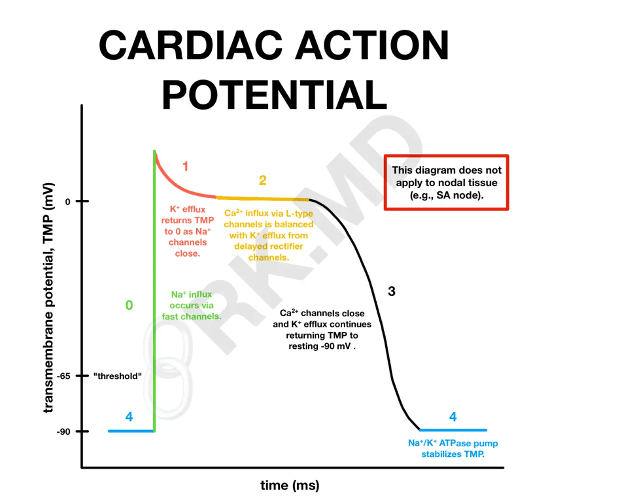
Question 73:
Answer: D) Phase 3
Explanation: Phase 3 of the cardiac action potential is the repolarisation phase where the membrane potential returns to its resting state. During this phase, potassium ions (K⁺) play a crucial role in the repolarisation process, moving out of the cell. This phase allows the cardiac muscle cell to reset and prepare for the next action potential.
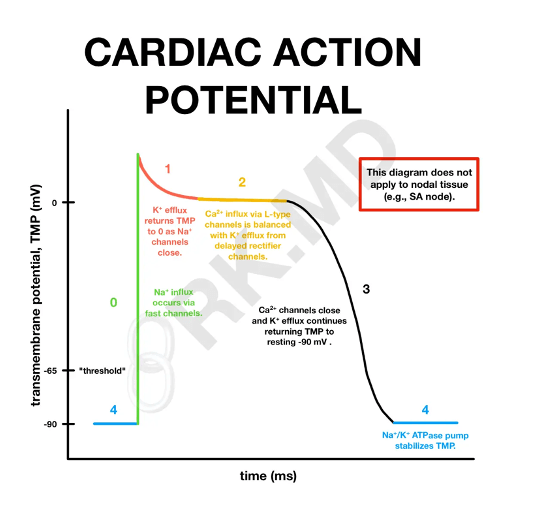
Question 74:
Answer: C) Calcium (Ca²⁺) via L-type channels
Explanation: During the plateau phase (Phase 2) of the cardiac action potential, calcium ions (Ca²⁺) play a crucial role in maintaining the membrane potential. The influx of calcium ions into the cell balances the efflux of potassium ions, leading to a prolonged depolarisation. This phase is significant because it allows for sustained muscle contraction.
Option D is incorrect because T-type calcium channels are involved in generating pacemaker potentials in cardiac nodal cells, not in the plateau phase of the action potential.
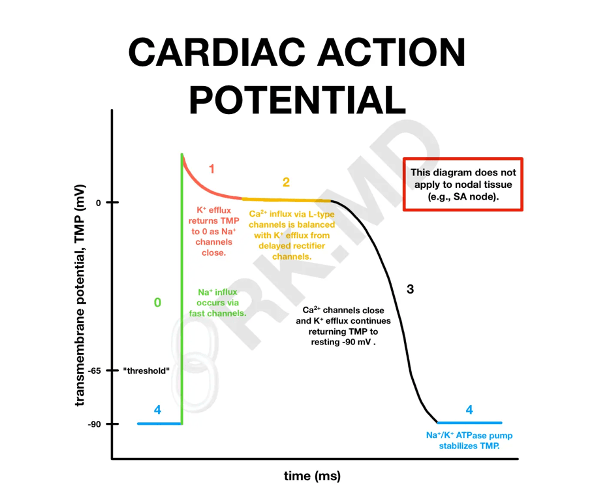
Question 75:
Answer: E) It represents the delay at the AV node allowing atria to empty into ventricles.
Explanation: The plateau phase (Phase 2) of the cardiac action potential is crucial in regulating the timing of cardiac muscle contraction. It allows for a prolonged depolarisation of the cell membrane due to the influx of calcium ions through L-type calcium channels. This extended depolarisation ensures that the atria contract fully and empty their contents (blood) into the ventricles before the ventricles contract. This delay is essential for efficient pumping of blood through the heart and proper coordination between atrial and ventricular contractions.
Option A is also true to some extent because the plateau phase helps in maintaining prolonged depolarisation of cardiac muscle cells, contributing to sustained contraction. However, in the context of the question asking for the primary significance of the plateau phase, option E is more directly related to the specific role of the AV node delay in allowing the atria to contract and empty blood into the ventricles before ventricular contraction begins.
Option B is incorrect because rapid depolarisation occurs during Phase 0 of the cardiac action potential.
Option C is incorrect because the plateau phase does not represent a period of absolute refractoriness. Absolute refractoriness is typically associated with Phase 0 to the end of phase 2.
Option D is incorrect because the plateau phase does not prevent calcium entry into the cell. In fact, the plateau phase is characterised by sustained calcium entry through L-type calcium channels.
Question 76:
Answer: C) Calcium (Ca²⁺) via L-type channels
Explanation: During the pacemaker cell action potential, the depolarisation phase (Phase 0) primarily involves the movement of calcium ions (Ca²⁺) into the cell. This influx of calcium ions is responsible for initiating the action potential in pacemaker cells.
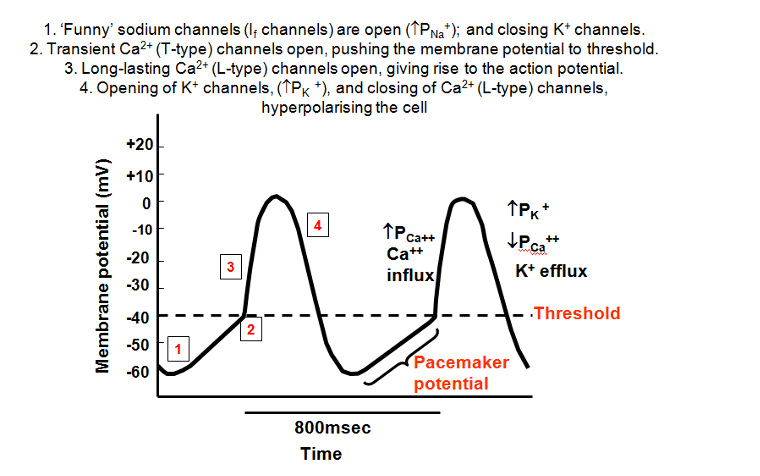
Question 77:
Answer: D) Phase 3
Explanation: Phase 3 of the pacemaker cell action potential involves the opening of voltage-gated potassium channels, leading to repolarisation. During this phase, potassium ions (K⁺) move out of the cell, allowing it to return to its resting state.

Question 78:
Answer: B) Potassium (K⁺) and Sodium (Na⁺)
Explanation: The “funny current” (If) in pacemaker cells is mainly carried by sodium (Na⁺) and potassium (K⁺) ions through HCN (hyperpolarisation-activated cyclic nucleotide-gated) channels. These channels are permeable to both sodium and potassium ions, but predominantly sodium at typical resting potentials. The gradual influx of positive charge through the “funny current” during diastole leads to the slow diastolic depolarisation, which eventually triggers the action potential in pacemaker cells.
Option A is incorrect because although sodium (Na⁺) and calcium (Ca²⁺) do contribute to the depolarisation of pacemaker cells, the funny current (If) does not involve calcium ions via T-type channels. T-type calcium channels become active later in the depolarisation process, after the funny current has already initiated the slow depolarisation.
Option C is incorrect because the funny current does not involve calcium (Ca²⁺) ions via T-type or L-type channels. Calcium channels, especially L-type, play a role later in the action potential, specifically during the rapid depolarisation phase after the threshold is reached, not during the initial diastolic depolarisation driven by the funny current.
Option D is incorrect because the funny current involves both sodium (Na⁺) and potassium (K⁺), not sodium alone. While the influx of sodium is more significant, the movement of potassium is also essential for the mixed conductance that characterises the funny current.
Option E is incorrect because the funny current does not involve calcium (Ca²⁺) via L-type channels. L-type calcium channels are active later, contributing to the plateau phase of the cardiac action potential. The funny current is specifically mediated by hyperpolarisation-activated cyclic nucleotide-gated (HCN) channels that allow sodium and potassium ions to move across the membrane, facilitating the slow diastolic depolarisation.
Question 79:
Answer: A) Atherosclerosis begins with lipid build up in arteries, leading to macrophage engulfment of LDL particles and the formation of foam cells. T cells subsequently join the process, promoting plaque formation and smooth muscle migration.
Explanation: Atherosclerosis is a complex process that involves the build-up of lipids, primarily low-density lipoprotein (LDL) particles, in the arterial walls. The correct sequence of events in atherosclerosis formation involves the following steps:
- Lipid Accumulation: Atherosclerosis begins with the accumulation of lipids, especially LDL cholesterol, within the arterial walls. These lipids infiltrate the intima, the innermost layer of the artery.
- Formation of Foam Cells: Macrophages in the arterial wall engulf the LDL particles, leading to the formation of foam cells. These foam cells are laden with lipid droplets.
- Inflammatory Response: The presence of foam cells triggers an inflammatory response within the artery walls. Inflammatory cells, including T cells, are recruited to the site of injury.
- Plaque Formation: The ongoing inflammation and accumulation of foam cells contribute to the formation of fatty streaks and eventually atherosclerotic plaques. These plaques consist of lipid-rich cores covered by fibrous caps.
- Smooth Muscle Migration: Smooth muscle cells from the arterial media migrate into the intima and proliferate, contributing to plaque growth.
T cells play a role in the later stages of atherosclerosis, primarily by promoting inflammation and contributing to the progression of plaques. The process can lead to arterial narrowing, reduced blood flow, and potentially serious complications such as heart attacks and strokes.
Question 80:
Answer: D) Beta-2 receptor; bronchodilation
Explanation: Beta-2 adrenergic receptors are predominantly found in bronchial smooth muscle. Activation of these receptors by agonists like epinephrine leads to bronchodilation, relaxing the airway smooth muscle and improving airflow. This effect is essential for managing conditions like asthma, where bronchoconstriction is a concern.
Beta-1 adrenergic receptors are primarily found in the heart, not in the lungs. They are activated by noradrenaline (released from the sympathetic nervous system) which increases heart rate (chronotropy), strength of heart contraction (ionotropy) & speed of electrical transmission through the heart (dromotropy).
Question 81:
Answer: E) Vasoconstriction
Explanation: Alpha-1 adrenergic receptor activation in blood vessels leads to vasoconstriction. This increases peripheral resistance and raises blood pressure. Alpha-1 agonists are sometimes used to treat conditions like hypotension.
Question 82:
Answer: D) Activation of Protein Kinase A
Explanation: Activation of beta-adrenergic receptors in cardiac myocytes leads to the activation of Protein Kinase A (PKA) via Gs signalling pathway. Noradrenaline binds to beta-1 adrenergic receptor (G-Protein coupled receptor). This causes GDP to dissociate & GTP to bind to alpha subunit. As a result of this, alpha subunit dissociates from beta & gamma subunits & activates adenylate cyclase. Adenylate cyclase converts ATP into cAMP. cAMP activates Protein Kinase A which can then phosphorylate proteins such as phospholamban, L-type calcium channels & ryanodine receptors to enhance cardiac function.
Option A is incorrect because while activation of beta-adrenergic receptors does lead to increased intracellular calcium levels, this occurs indirectly through the activation of PKA and subsequent phosphorylation of calcium handling proteins, rather than being a direct downstream signalling event.
Option B is incorrect because activation of phospholipase C is typically associated with G-protein coupled receptors that signal through the Gq pathway, not the beta-adrenergic receptors which primarily signal through the Gs pathway.
Option C is incorrect because beta-adrenergic receptors stimulate adenylate cyclase, leading to an increase in cAMP levels, rather than inhibiting adenylate cyclase.
Option E is incorrect because beta-adrenergic receptors increase cAMP levels through stimulation of adenylate cyclase, leading to activation of PKA, rather than inactivating cAMP.
Question 83:
Answer: B) Inhibiting norepinephrine release
Explanation: Alpha-2 adrenergic receptors on presynaptic terminals act as autoreceptors, inhibiting the further release of norepinephrine when stimulated. This provides negative feedback to regulate sympathetic activity.
Question 84:
Answer: C) The medullary cardiovascular control centres
Explanation: Both the aortic arch baroreceptors and carotid sinus baroreceptors send sensory information to the brainstem cardiovascular control centres, particularly the medulla oblongata. This information helps regulate autonomic responses to maintain blood pressure within a normal range.
Option A is incorrect because while sensory information can be transmitted through the spinal cord, the primary integration and processing centre for baroreceptor input is the medullary oblongata.
Option B is incorrect because the sinoatrial node (SAN) is a pacemaker of the heart that controls heart rate, but it is not the primary recipient of baroreceptor sensory information.
Option D is incorrect because the adrenal medulla is involved in the release of catecholamines (adrenaline and noradrenaline) during the fight-or-flight.
Option E is incorrect because the thalamus is involved in sensory perception and regulation of motor functions.
Question 85:
Answer: C) Arterioles
Explanation: Arterioles are known as resistance vessels because they regulate blood flow into organs and tissues by adjusting their diameter. Their small size and extensive smooth muscle make them the primary site for controlling peripheral resistance.
Question 86:
Answer: E) It causes systemic vasoconstriction.
Explanation: Angiotensin II is a potent vasoconstrictor that causes systemic vasoconstriction, leading to an increase in blood pressure. This is a primary mechanism through which it regulates cardiovascular function and helps maintain blood pressure. Angiotensin II also triggers the release of ADH/vasopressin which increases water reabsorption, aldosterone release to increase sodium reabsorption & noradrenaline release activating the sympathetic nervous system.
Option B is incorrect because although angiotensin II indirectly promotes fluid retention by stimulating aldosterone secretion from the adrenal cortex, its primary action within the cardiovascular system is vasoconstriction.
Option C is incorrect because angiotensin II does not directly increase heart rate; it triggers the release of noradrenaline which increases heart rate.
Option D is incorrect because angiotensin II does not induce bronchoconstriction; it mainly affects blood vessels to regulate blood pressure.
Question 87:
Answer: C) Endocardial cushions
Explanation: Endocardial cushions are specialised areas of thickened endocardium that play a crucial role in septation during heart development. They contribute to the formation of the AV septum, which separates the atria, and the membranous interventricular septum, which divides the ventricles.
Option A is incorrect because the bulbus cordis contributes to the formation of the right ventricle and the outflow tracts of both ventricles.
Option B is incorrect because the truncus arteriosus gives rise to the aorta and the pulmonary trunk.
Option D is incorrect because the aorticopulmonary septum forms the division between the aorta and the pulmonary artery but does not contribute to the AV septum.
Option E is incorrect because the sinus venosus is involved in forming parts of the atria and the vena cava, not the AV septum or the membranous interventricular septum.
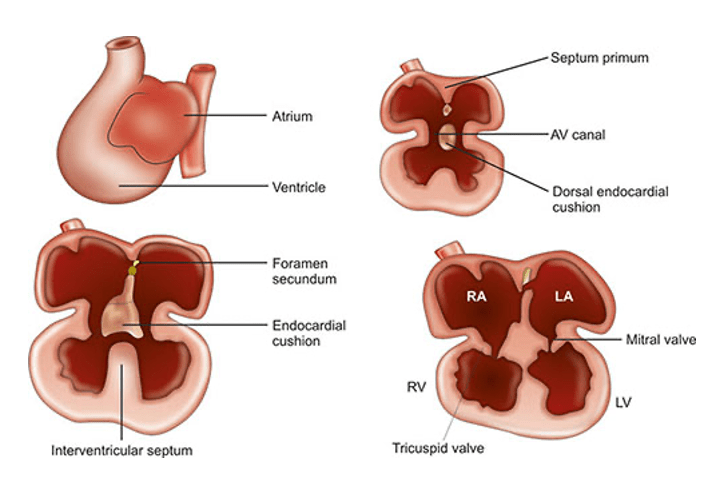
Question 88:
Answer: B) Septum primum
Explanation: The septum primum is the structure that divides the primitive atrium into the right and left atria during embryonic development. It grows downwards from the roof of the primitive atrium towards the endocardial cushions, eventually forming a complete separation between the two atria, with the development of the septum secundum and the formation of the foramen ovale completing this process.
Option A is incorrect because the term “atrial septum” is a general term that encompasses the entire structure formed by the septum primum and septum secundum, not a specific embryonic structure.
Option C is incorrect because the endocardial cushions contribute to the formation of the AV septum and the membranous part of the interventricular.
Option D is incorrect because the aorticopulmonary septum is involved in separating the aorta and pulmonary artery, not the atria.
Option E is incorrect because the bulbus cordis contributes to the formation of the right ventricle and the outflow tracts of both ventricles.
Question 89:
Answer: E) HbF is composed of alpha & gamma subunits whereas HbA is composed of alpha & beta subunits.
Explanation: Fetal hemoglobin (HbF) differs from adult hemoglobin (HbA) in its subunit composition. HbF is composed of two alpha and two gamma subunits, whereas HbA is composed of two alpha and two beta subunits. This difference in subunit composition gives HbF a higher affinity for oxygen than HbA, which is crucial for the efficient transfer of oxygen from the mother to the fetus.
Option A is incorrect because while it is true that HbF has a higher affinity for oxygen than HbA, this option does not address the structural differences between HbF & HbA.
Option B is incorrect because HbF does not contain beta chains; instead, it contains gamma chains.
Option C is incorrect because both HbF and HbA are produced in the bone marrow.
Option D is incorrect because the efficiency of binding carbon dioxide is not the primary distinguishing factor between HbF and HbA.
Question 90:
Answer: A) Left horn of Sinus Venosus
Explanation: The left horn of the sinus venosus contributes to the formation of the coronary sinus, which acts as a vessel for draining deoxygenated blood from the myocardium (heart muscle) back into the right atrium. This is an essential component of the venous return system within the heart.
Option B is incorrect because the sphenoidal sinus is a paranasal sinus located within the sphenoid bone.
Option C is incorrect because the right horn of the sinus venosus contributes to the formation of parts of the right atrium.
Option D is incorrect because the ductus venosus is a fetal shunt that allows blood to bypass the liver; it does not form the coronary sinus.
Option E is incorrect because the inferior vena cava is a large vein that carries deoxygenated blood from the lower half of the body to the right atrium, but it is not formed from the left horn of the sinus venosus.
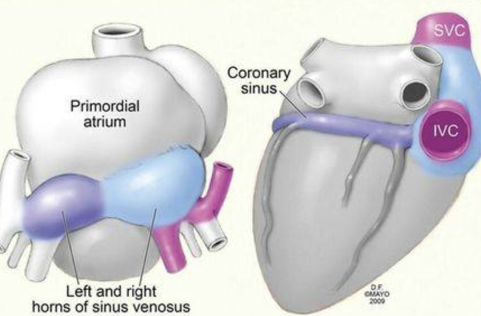
Question 91:
Answer: B) It can cause a right-to-left shunt
Explanation: A patent fossa ovalis refers to the persistence of a flap-like opening in the interatrial septum, which should typically close after birth. If it remains open (patent) in adulthood, it can allow blood to shunt from the right atrium to the left atrium, bypassing the lungs, and potentially leading to cyanosis (bluish discoloration due to reduced oxygenation). This is related to fetal circulation, where the foramen ovale allows blood to bypass the non-functional fetal lungs.
Option A is incorrect because a patent fossa ovalis is not a normal variant in adults; it can have clinical consequences.
Option C is incorrect because a patent fossa ovalis typically causes a right-to-left shunt, not a left-to-right shunt. A left-to-right shunt would not typically lead to cyanosis but rather could cause increased pulmonary blood flow and potential heart failure.
Option D is incorrect because a patent fossa ovalis does not facilitate left ventricular filling. The normal path of blood flow to the left ventricle is through the left atrium and the mitral valve.
Option E is incorrect because a patent fossa ovalis can have significant clinical implications and is not merely a visual defect.
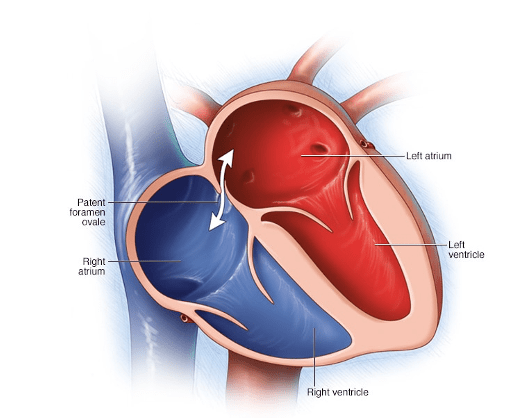
Question 92:
Answer: B) Tendon of Todaro
Explanation: The “Triangle of Koch” is an anatomical region in the heart where the atrioventricular (AV) node is located. The Tendon of Todaro, a fibrous structure within this triangle, serves as the point of origin for the AV node, which plays a crucial role in the electrical conduction system of the heart.
Option A is incorrect because the atrioventricular orifice is not within the Triangle of Koch and does not specifically indicate the location of the AV node.
Option C is incorrect because the ostium secundum is an opening in the atrial septum during fetal development which is unrelated to the Triangle of Koch.
Option D is incorrect because, although the coronary sinus is one of the borders of the Triangle of Koch, it is not the specific structure within the triangle where the AV node is located.
Option E is incorrect because the mitral valve is located between the left atrium and left ventricle and is not related to the Triangle of Koch in the right atrium.
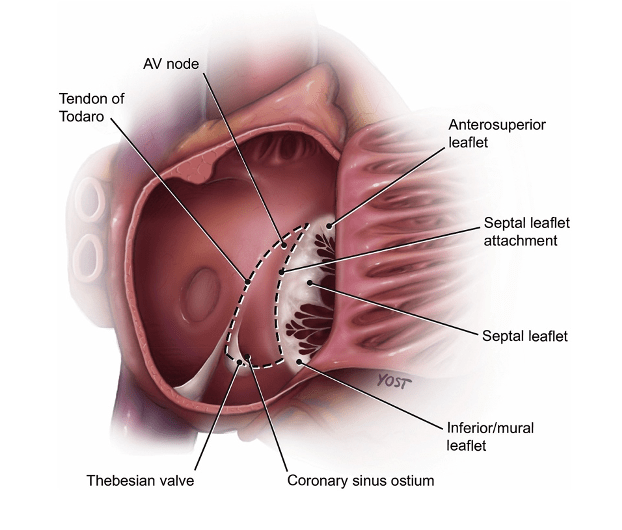
Question 93:
Answer: D) Autonomic nervous system
Explanation: The cardiac plexus is an intricate network of nerves located near the heart that receives contributions from both the sympathetic and parasympathetic divisions of the autonomic nervous system. The autonomic nervous system regulates involuntary physiological functions, including heart rate and cardiac output. The sympathetic nervous system contributes to the cardiac plexus by increasing heart rate and force of contraction, while the parasympathetic nervous system contributes by decreasing heart rate. This dual innervation allows for fine-tuned regulation of cardiac function in response to varying physiological demands.
Option A is incorrect because, while the sympathetic nervous system contributes to the cardiac plexus, it is only one part of the autonomic nervous system.
Option B is incorrect because the dorsal root ganglion contains sensory neurons that convey information to the central nervous system but does not directly contribute to the cardiac plexus.
Option C is incorrect because, while the parasympathetic nervous system contributes to the cardiac plexus, it is only one part of the autonomic nervous system.
Option E is incorrect because the somatosensory nervous system is responsible for transmitting sensory information from the body to the brain.
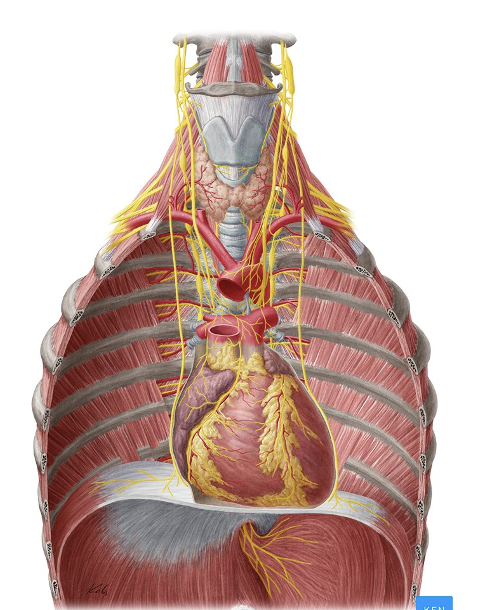
Question 94:
Answer: B) Pain
Explanation: Visceral afferent fibres primarily transmit information related to pain (nociception) from the internal organs. These fibres play a crucial role in signalling discomfort or pathology within the body’s internal structures.
Option C is incorrect because blood pressure information from the heart is primarily transmitted via baroreceptors.
Option D is incorrect because pH sensing is detected by chemoreceptors.
Option E is incorrect because heart rate information is primarily transmitted by autonomic nerves.
Question 95:
Answer: A) They are both valveless.
Explanation: Both the inferior vena cava (IVC) and superior vena cava (SVC) are valveless veins. Unlike many other veins in the body, they lack valves to prevent backflow of blood. This anatomical feature facilitates the efficient return of blood to the right atrium of the heart.
Question 96:
Answer: B) It contracts to push blood through veins; it is most active in the lower limbs.
Explanation: The skeletal muscle pump is a mechanism that aids venous return by contracting skeletal muscles, which compress nearby veins. This compression helps push blood in the veins towards the heart, particularly in the lower limbs where this mechanism is most actively utilised.
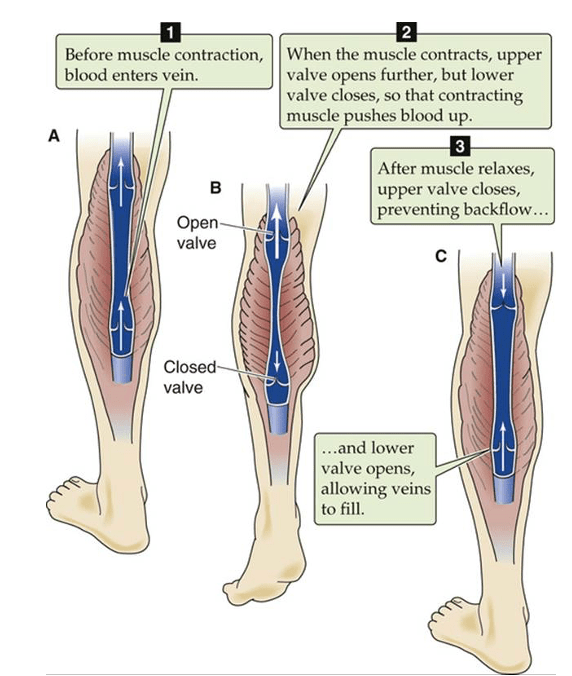
Question 97:
Answer: C) The T-wave vector points away from the epicardium and towards the endocardium.
Explanation: During ventricular repolarisation, the T-wave vector typically points away from the epicardium (outer layer of the heart) and towards the endocardium (inner layer of the heart). This vector direction reflects the sequence of repolarisation as it starts epicardium to endocardium. Duration of action potential in epicardial cells is shorter which is why it starts here. Furthermore, the T-wave appears as a positive deflection on an ECG because the wave of repolarisation is moving away from the positive electrode (typically placed on the skin near the heart), which corresponds to the epicardium. The movement of electrical activity from epicardium (at the apex of the heart) to endocardium (moving back up towards the atria) results in the positive deflection seen in the T-wave.

Question 98:
Answer: A) Endocardium to epicardium
Explanation: In an electrocardiogram (ECG), the electrical vector of depolarisation typically follows from the endocardium (inner layer of the heart) to the epicardium (outer layer of the heart). This directional flow of depolarisation is represented by the QRS complex on the ECG, where the initial small deflection (Q-wave) indicates depolarisation starting from the endocardium (depolarisation of the interventricular septum) and progressing towards the epicardium with the larger R-wave (apex of the heart). The T-wave, representing repolarisation, generally moves in the opposite direction, from the epicardium back towards the endocardium.
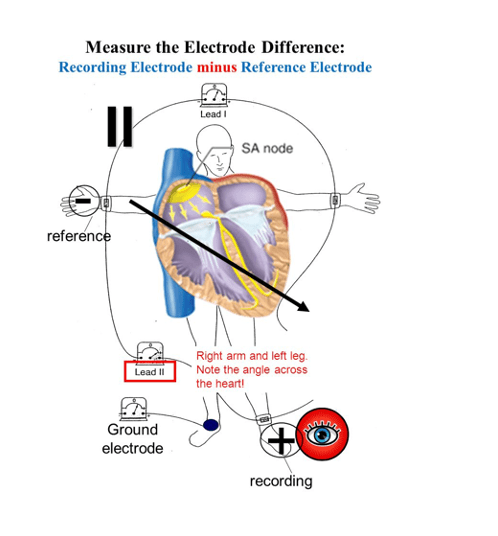
Question 99:
Answer: B) ARP is the time when cells cannot respond to any stimulus, while RRP allows for a response to strong stimuli.
Explanation: The ARP is the period during which cardiac muscle cells cannot respond to any stimulus, ensuring that there is no premature contraction. In contrast, the RRP follows the ARP and allows cells to respond to strong stimuli, which can be crucial for preventing arrhythmias by ensuring that the heart’s contractions are coordinated and controlled.

Question 100:
Answer: C) Endocardium; they facilitate rapid and coordinated ventricular depolarisation.
Explanation: Purkinje fibres are specialised cardiac conduction fibres found in the endocardium (specifically the subendocardium) of the heart. Their location within the endocardium allows them to conduct electrical impulses rapidly and efficiently throughout the ventricles, ensuring synchronised and coordinated ventricular contractions, which is essential for effective pumping of blood.

Question 101:
Answer: D) Stable angina
Explanation: Stable angina is characterised by chest pain or discomfort that occurs predictably with exertion or stress and is relieved by rest. It is typically associated with a fixed atherosclerotic plaque in a coronary artery, causing reduced blood flow to the heart muscle during periods of increased demand.
Option A is incorrect because Prinzmetal’s angina (variant angina) is caused by coronary artery spasm rather than exertion and is not typically relieved by rest.
Option B is incorrect because unstable angina is characterised by chest pain that occurs unpredictably and often at rest.
Option C is incorrect because variant angina (Prinzmetal’s angina) refers specifically to angina caused by coronary artery spasm rather than exertion.
Option E is incorrect because there is no specific category known as “common angina” in clinical terminology.
Question 102:
Answer: D) Reduced plasma oncotic pressure
Explanation: Hypoalbuminemia, a common consequence of chronic liver disease, leads to a reduction in the concentration of albumin in the blood. Albumin plays a crucial role in maintaining plasma oncotic pressure, which opposes the outward movement of water from the capillaries into the interstitial spaces. When albumin levels are low, there is a decreased ability to “hold” water within the vascular compartment, resulting in reduced plasma oncotic pressure. This, in turn, promotes the movement of fluid from the blood vessels into the surrounding tissues, leading to oedema. It also means that less fluid is reabsorbed at the venule end of the capillary resulting in reduced lymphatic drainage (due to excess fluid accumulation). However, this is an indirect effect of low protein levels in the blood.
Question 103:
Answer: E) Moderator bands
Explanation: Moderator bands, also known as septomarginal trabeculae, are unique structures found in the right ventricle of the heart. These muscular bands stretch from the interventricular septum to the anterior papillary muscle. Their primary function is to facilitate the coordinated contraction of the papillary muscles before the rest of the right ventricular walls contract. By transmitting electrical signals rapidly across the right ventricle, moderator bands ensure that the papillary muscles contract just before the ventricular walls, which is crucial for preventing regurgitation of blood through the tricuspid valve back into the atria during ventricular systole.
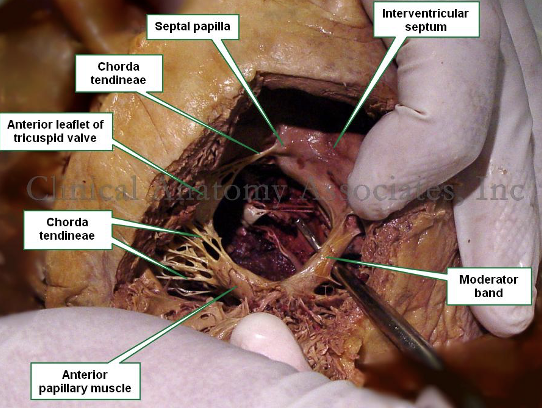
Question 104:
Answer: C) Brachiocephalic artery
Explanation: The brachiocephalic artery arises from the aortic arch and carries oxygenated blood to the head and arms. It branches into the right subclavian artery, supplying the right arm, and the right common carotid artery, which supplies blood to the right side of the head and neck.
Option A is incorrect because the pulmonary artery carries deoxygenated blood from the heart to the lungs, not oxygenated blood to the upper body.
Option B is incorrect because although the subclavian artery arises separately from the aortic arch it mainly carries oxygenated blood to the arms not head.
Option D is incorrect because the superior vena cava returns deoxygenated blood from the upper body to the heart.
Option E is incorrect because although the common carotid artery originates directly from the aortic arch, it supplies blood primarily to the head and neck, not the entire upper body & arms.
Question 105:
Answer: B) Right atrial wall
Explanation: Pectinate muscles are comb-like muscular ridges that are primarily found in the walls of the right atrium. These muscles are responsible for increasing the surface area of the atrium, allowing it to accommodate the incoming blood from the body’s venous circulation. They are especially prominent in the right atrium compared to the left atrium.
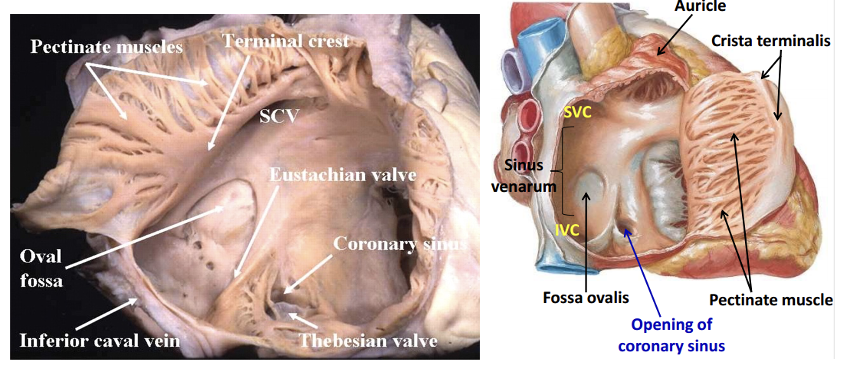
Question 106:
Answer: D) To increase contractile efficiency
Explanation: Trabeculae carneae are muscular projections found in the ventricles of the heart. Their primary function is to increase the contractile efficiency of the heart by providing additional contractile force. They help the ventricles pump blood effectively, especially during systole when the ventricles contract.
Option A is incorrect because trabeculae carneae do not primarily serve to reinforce the myocardium structurally.
Option B is incorrect because conducting electrical impulses is the role of the specialised conduction system of the heart (e.g., Purkinje fibres, bundle branches).
Option C is incorrect because preventing backflow of blood is achieved by the atrioventricular valves (tricuspid and mitral valves) and semilunar valves (aortic and pulmonary valves).
Option E is incorrect because the speed of heart contraction is regulated by the electrical conduction system.
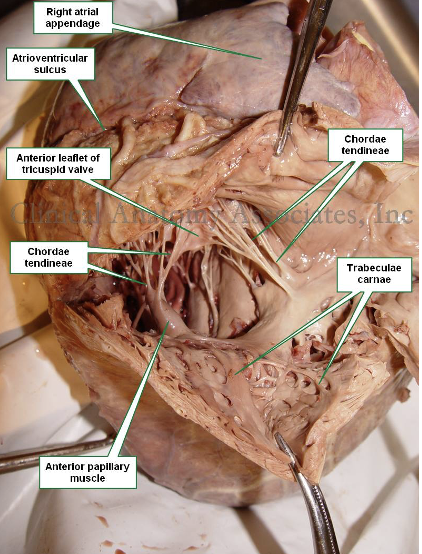
Question 107:
Answer: B) Chordae tendinae
Explanation: Chordae tendinae are cord-like structures that connect the cusps of the atrioventricular (AV) valves (tricuspid and mitral valves) to the papillary muscles in the ventricles. They play a critical role in preventing the prolapse of these valves into the atria when the ventricles contract. This helps maintain unidirectional blood flow through the heart. Papillary muscles pull to make chordae tendinae taut.

Question 108:
Answer: C) Moderator bands
Explanation: Moderator bands, also known as septomarginal trabeculae, are specialised muscular structures found in the right ventricle of the heart. They are responsible for transmitting electrical signals and contraction forces to the papillary muscles. This coordinated contraction of the papillary muscles via the moderator bands prevents the prolapse of the tricuspid valve during ventricular contraction, ensuring proper valve function and blood flow.

Question 109:
Answer: C) Tropomyosin
Explanation: In resting cardiac muscle cells, tropomyosin prevents myosin from binding to actin by covering the myosin-binding sites on the actin filaments. This regulatory protein plays a crucial role in maintaining muscle relaxation when calcium levels are low.
Option A is incorrect because troponin C binds calcium ions to initiate muscle contraction but does not directly prevent myosin from binding to actin. When calcium binds to troponin C, this causes tropomyosin to move & uncover actin-myosin binding site.
Option B is incorrect because myosin light chain kinase is involved in the phosphorylation of myosin light chains, which regulates the interaction between actin and myosin during muscle contraction, rather than preventing binding in resting muscle.
Option D is incorrect because troponin T is part of the troponin complex that interacts with tropomyosin and calcium ions to regulate muscle contraction.
Option E is incorrect because calcium ions are required for muscle contraction and are involved in the activation of the contractile apparatus.
Question 110:
Answer: A) To store calcium ions for muscle contraction
Explanation: The sarcoplasmic reticulum (SR) in cardiac muscle cells serves as a specialised organelle for the storage and release of calcium ions (Ca²⁺) during the process of muscle contraction. When an action potential triggers the release of calcium ions from the SR, it initiates the contractile process by allowing the interaction between actin and myosin filaments. The stored calcium ions are crucial for the regulation of cardiac muscle contraction.
Option B is incorrect because ATP is primarily synthesised in mitochondria. ATP can NOT be stored.
Option C is incorrect because muscle contraction is initiated by the release of calcium ions from the SR via ryanodine channels.
Option D is incorrect because the SR releases calcium ions during muscle contraction rather than initiating it.
Option E is incorrect because the action potential is initiated by the depolarization of the cell membrane.
Question 111:
Answer: B) Sarcomere
Explanation: Sarcomeres are the fundamental contractile units within cardiac muscle cells. Sarcomeres are composed of overlapping actin and myosin filaments that slide past each other during contraction, generating the force necessary for muscle contraction. Each sarcomere spans from Z-line to Z-line and is the structural and functional unit responsible for the striated appearance of cardiac muscle under a microscope.
Option A, myofibrils, is also correct because myofibrils are large structures composed of repeating sarcomeres. However Option B is a better answer because sarcomeres are the individual contractile units involved in muscle contraction.
Option C, T-tubules, is incorrect because T-tubules (transverse tubules) are invaginations of the cell membrane (sarcolemma) that penetrate into the interior of the muscle cell. They play a role in transmitting action potentials from the cell surface to the interior, facilitating synchronous muscle contraction, but they are not the contractile units themselves.
Options D (A-band) and E (M-band) are incorrect because they refer to specific regions within the sarcomere. The A-band is the region where thick filaments (myosin) are located, while the M-band is the middle of the sarcomere where the thick filaments are linked together. These are structural components within the sarcomere but are not synonymous with the contractile units responsible for muscle contraction, which are the sarcomeres themselves.
Question 112:
Answer: C) The endocardium lines the inner surface of the heart chambers and contributes to smooth blood flow.
Explanation: The endocardium is the innermost layer of the heart wall and lines the inner surfaces of the heart chambers. Its primary function is to provide a smooth lining that allows for efficient blood flow within the heart. The endocardium is composed of endothelial cells and connective tissue and is distinct from the epicardium and myocardium, which are the outer layers of the heart wall responsible for contraction and protection. The valves of the heart are formed by specialised structures within the endocardium, but the main function of the endocardium is to ensure smooth cardiac function.
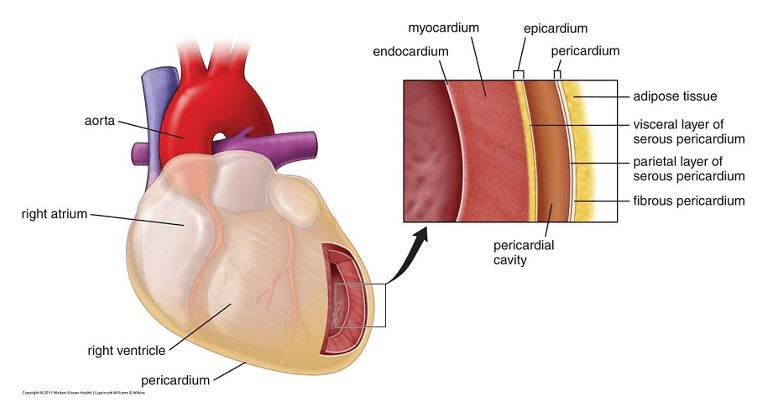
Question 113:
Answer: A) Fibrous pericardium
Explanation: The fibrous pericardium is the outermost layer of the pericardium and is tough and fibrous in nature. It provides structural support to the heart and anchors it within the mediastinum of the thoracic cavity.
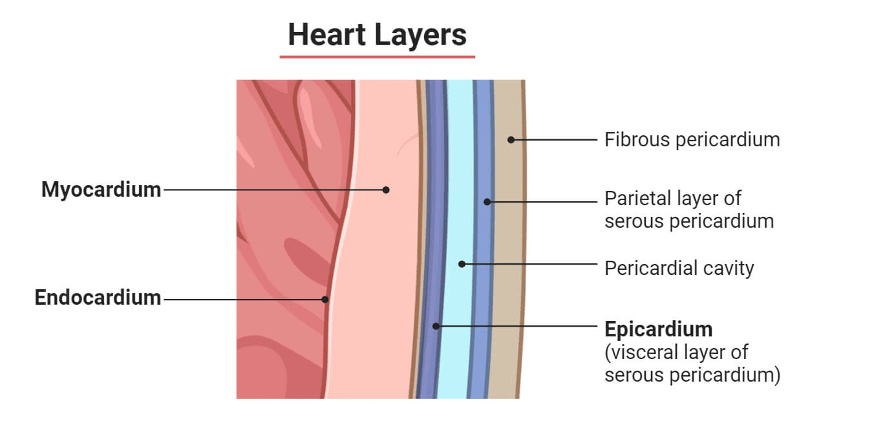
Question 114:
Answer: C) Visceral pericardium
Explanation: The visceral pericardium, also known as the epicardium, is the innermost layer of the pericardium and is closely adhered to the heart muscle. It secretes a small amount of serous fluid into the pericardial cavity, which lubricates the surfaces of the heart and pericardium, reducing friction during cardiac contractions. A third name for the visceral pericardium is the serous layer of the pericardium.
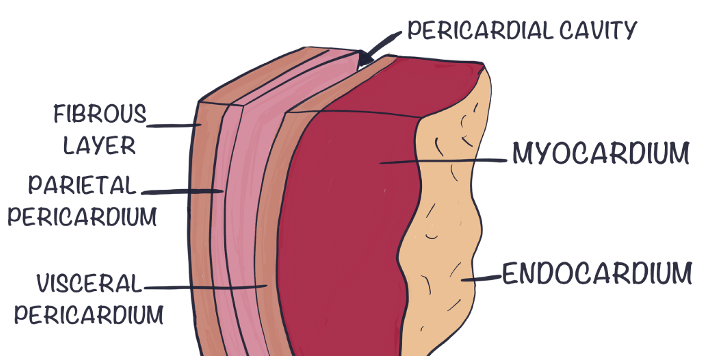
Question 115:
Answer: D) Cardiac muscle alone
Explanation: Cardiac muscle is the correct answer because it exhibits both involuntary contractions and striations. Involuntary contractions mean that cardiac muscle contracts without conscious control, which is characteristic of the autonomic nervous system’s influence over heart function. Striations refer to the striped appearance under a microscope due to the organised arrangement of contractile proteins (actin and myosin). These striations are similar to skeletal muscle but different in structure and function.
Smooth muscle exhibit involuntary control but lack striations. On the other hand, skeletal muscles are under voluntary control but contain striations.
Question 116:
Answer: C) The great cardiac vein drains into the coronary sinus.
Explanation: The great cardiac vein is a major coronary vein that travels alongside the left anterior descending artery (LAD) and drains into the coronary sinus. It plays a crucial role in returning deoxygenated blood from the myocardium to the right atrium for subsequent oxygenation. The proximity to the LAD ensures efficient drainage from the left ventricle and interventricular septum.
Option A is incorrect because the great cardiac vein primarily drains deoxygenated blood into the left atrium.
Option B is incorrect because the great cardiac vein runs alongside the left coronary artery.
Option D is incorrect because the great cardiac vein carries deoxygenated blood to the lungs in order for blood to be oxygenated.
Option E is incorrect because the great cardiac vein does not drain directly into the right atrium; it drains into the coronary sinus.

Question 117:
Answer: B) Middle cardiac vein
Explanation: The middle cardiac vein primarily drains the posterior aspect of the left ventricle and frequently connects directly to the coronary sinus. This venous drainage pattern ensures efficient return of deoxygenated blood from the posterior left ventricle to the right atrium.
Option A is incorrect because the great cardiac vein drains the anterior aspect of the heart and does not primarily drain the posterior left ventricle.
Option C is incorrect because the small cardiac vein drains the right ventricle and does not primarily drain the posterior left ventricle.
Option D is incorrect because anterior cardiac veins drain the anterior surface of the right ventricle and right atrium.
Question 118:
Answer: E) Right marginal vein
Explanation: The right marginal vein courses along the right atrium and usually drains directly into the right atrium rather than the coronary sinus. It collects deoxygenated blood from the right margin of the heart and contributes to the venous drainage of the heart.
Option A is incorrect because the great cardiac vein drains the anterior aspect of the heart and typically empties into the coronary sinus.
Option B is incorrect because the middle cardiac vein primarily drains the posterior aspect of the left ventricle and empties into the coronary sinus.
Option C is incorrect because the small cardiac vein drains the right ventricle and also empties into the coronary sinus.
Option D is incorrect because although the anterior cardiac veins empty into the right atrium, they drain the anterior surface of the right ventricle and right atrium, not along the right atrium only. Therefore option E is the best answer.
Question 119:
Answer: A) Right atrium
Explanation: The coronary sinus is a dilated venous structure located in the right atrium of the heart. It serves as a common collecting point for most of the cardiac veins, including the great cardiac vein, middle cardiac vein, small cardiac vein, and others. The coronary sinus then delivers deoxygenated blood into the right atrium for subsequent oxygenation.
Question 120:
Answer: A) T12
Explanation: The aortic hiatus is located at the level of the 12th thoracic vertebra (T12). It is an opening in the diaphragm through which the aorta passes as it descends from the thoracic cavity into the abdominal cavity. This anatomical structure is crucial for the passage of the descending aorta and plays a key role in maintaining the separation between the thoracic and abdominal cavities.
Aortic hiatus has 12 letters = passes through T12 vertebral level
Option B is incorrect because the vena cava passes through the diaphragm at T8 vertebral level. Vena cava has 8 letters so passes through T8.
Option C is incorrect because T4 is the site of the Angle of Louis. This is where the ascending aorta becomes the arch of the aorta. It is also where the arch of aorta becomes the descending aorta too! T4 sternal angle also separates the superior & inferior mediastinal compartments.
Option D is incorrect because the inferior mesenteric artery branches out of the aorta at L1 vertebral level.
Option E is incorrect because the oesophagus passes through the diaphragm at T10. Oesophagus has 10 letter = passes through at T10 vertebral level.
Question 121:
Answer: C) Sinusoidal capillaries
Explanation: Sinusoidal capillaries, also known as discontinuous capillaries, have the largest gaps between their endothelial cells. These gaps allow for the free exchange of large molecules, cells, and even blood components between the blood and surrounding tissues. They are commonly found in organs like the liver, spleen, and bone marrow, where extensive exchange and filtration are necessary.
Option A is incorrect because continuous capillaries have tight junctions between endothelial cells and a complete basement membrane, limiting the passage of larger molecules.
Option B is incorrect because fenestrated capillaries have small pores (fenestrations) in the endothelial cells, allowing for rapid exchange of smaller molecules but not as extensive as sinusoidal capillaries.
Option D is incorrect because capillary pericytes are cells that wrap around capillaries and are involved in their maintenance and regulation but do not directly contribute to substance exchange.

Question 122:
Answer: B) T8
Explanation: The inferior vena cava (IVC) pierces the diaphragm at the level of the 8th thoracic vertebra (T8) as it ascends from the abdominal cavity into the thoracic cavity. This anatomical landmark is important for understanding the relationship between the IVC and the diaphragm.
Vena cava has 8 letters so passes through T8 vertebral level.
Oesophagus has 10 letter = passes through at T10 vertebral level.
Aortic hiatus has 12 letters = passes through T12 vertebral level
Question 123:
Answer: A) Vagus nerve (cranial nerve X)
Explanation: The vagus nerve (cranial nerve X) is primarily responsible for the parasympathetic functions in the body, often referred to as the “rest and digest” functions. It innervates various organs, including the heart, and plays a key role in slowing down heart rate, promoting digestion, and conserving energy during periods of relaxation.
Option B is incorrect because the facial nerve (cranial nerve VII) is responsible movements involved in fascial expression, taste in anterior 2/3rd of tongue & innervating the submandibular & sublingual glands.
Option C is incorrect because the glossopharyngeal nerve (cranial nerve IX) is involved in taste sensation from the posterior third of the tongue , innervating parotid gland & relaying information from the carotid sinus back to medullary cardiovascular centre in the brainstem.
Option D is incorrect because the accessory nerve (cranial nerve XI) primarily controls muscles involved in head and shoulder movement (trapezius & sternocleidomastoid).
Option E is incorrect because the hypoglossal nerve (cranial nerve XII) controls muscles of the tongue.
Question 124:
Answer: B) Calcium-sodium exchanger (NCX antiporter)
Explanation: The sodium-calcium exchanger (NCX antiporter) is responsible for removing calcium ions (Ca²⁺) from the cytoplasm of cardiac muscle cells during the relaxation phase. It exchanges three sodium ions (Na⁺) into the cell for every one calcium ion moved out. This process helps restore low intracellular calcium levels, promoting muscle relaxation and preparing the cell for the next contraction cycle.
Option A is incorrect because the sodium-potassium pump (Na⁺/K⁺ pump) primarily transports sodium ions out of the cell and potassium ions into the cell to maintain cellular ion balance.
Option C is incorrect because the sodium-calcium pump (Na⁺/Ca²⁺ pump) is not an actual physiological transporter. The main transporter of calcium & sodium is the sodium-calcium exchanger (NCX antiporter).
Option D is incorrect because the potassium-calcium cotransporter (K⁺/Ca²⁺ cotransporter) exchanges potassium ions for calcium ions across the cell membrane.
Option E is incorrect because SERCA pump (Sarcoplasmic/Endoplasmic Reticulum Calcium ATPase) is responsible for pumping calcium ions from the cytoplasm into the sarcoplasmic reticulum during muscle relaxation, not out of the cell.
Question 125:
Answer: C) L-type calcium (Ca²⁺) channel
Explanation: The L-type calcium channel plays a crucial role in cardiac muscle contraction. It allows the influx of calcium ions from the extracellular fluid into the cell, which triggers the release of additional calcium ions from the sarcoplasmic reticulum. This increase in intracellular calcium concentration leads to muscle contraction by initiating the sliding of myofilaments (actin and myosin).
Option A is incorrect because T-type channels are involved in pacemaker activity of cardiac nodes and are more characteristic of neurons and some smooth muscle cells, not cardiac muscle cells.
Option B is incorrect because NCX is responsible for the exchange of calcium ions out of the cell in exchange for sodium ions, not for the initial entry of calcium ions during muscle contraction.
Option C, SERCA (Sarcoplasmic/Endoplasmic Reticulum Calcium ATPase), is incorrect because SERCA pumps calcium ions from the cytoplasm into the sarcoplasmic reticulum during muscle relaxation, not into the cell during muscle contraction.
Option E, RyR (ryanodine) receptors, is incorrect because RyR receptors are calcium release channels located on the sarcoplasmic reticulum, responsible for releasing calcium from the SR into the cytoplasm in response to calcium-induced calcium release (CICR), not for calcium entry from the extracellular space.
Question 126:
Answer: A) T-tubules (transverse tubules)
Explanation: T-tubules are invaginations of the sarcolemma (cell membrane) that penetrate deep into the interior of cardiac muscle cells. They play a critical role in transmitting action potentials from the cell surface to the sarcoplasmic reticulum, which is responsible for releasing calcium ions (Ca²⁺) to trigger muscle contraction. This arrangement ensures coordinated and synchronous contraction of cardiac muscle fibres.
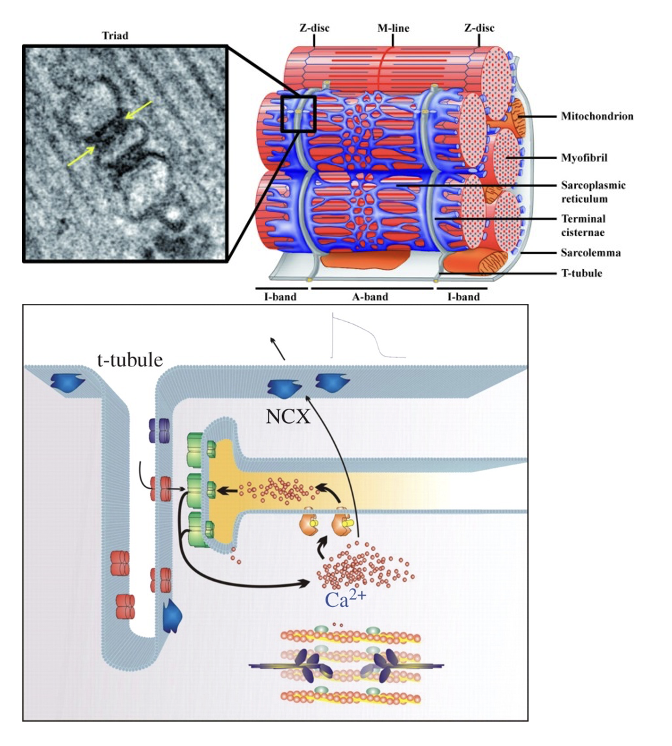
Question 127:
Answer: A) Pulse pressure is the difference between systolic and diastolic blood pressure and reflects the elasticity of arteries.
Explanation: Pulse pressure represents the change in pressure within the arteries during the cardiac cycle. It is calculated as the difference between systolic and diastolic blood pressure. Pulse pressure provides insights into the elasticity and compliance of arterial walls. Increased pulse pressure can be a sign of arterial stiffness or conditions such as aortic regurgitation, where blood leaks back into the left ventricle during diastole, causing an increase in systolic pressure. Monitoring pulse pressure is crucial for assessing cardiovascular health and diagnosing various conditions.
Question 128:
Answer: A) Stroke Volume (SV) = End-Diastolic Volume (EDV) – End-Systolic Volume (ESV). Stroke volume is the amount of blood ejected by the ventricle during systole.
Explanation: Stroke volume (SV) is the volume of blood ejected by the ventricle with each heartbeat. It can be calculated by subtracting the end-systolic volume (ESV), which is the volume of blood remaining in the ventricle at the end of systole, from the end-diastolic volume (EDV), which is the volume of blood in the ventricle at the end of diastole. This formula (SV = EDV – ESV) represents the fundamental relationship between these volumes and defines the stroke volume’s contribution to cardiac output. EDV represents the ventricle’s preload, while ESV indicates the afterload. Understanding stroke volume is crucial for assessing the heart’s efficiency and function.
Question 129:
Answer: A) P-wave
Explanation: In the Wiggers diagram, the P-wave corresponds to atrial depolarisation. This wave represents the electrical activity that triggers atrial contraction (atrial systole). Atrial depolarisation initiates the contraction of the atria, which helps push blood into the ventricles. Understanding the P-wave’s significance is essential for diagnosing arrhythmias and assessing atrial function.
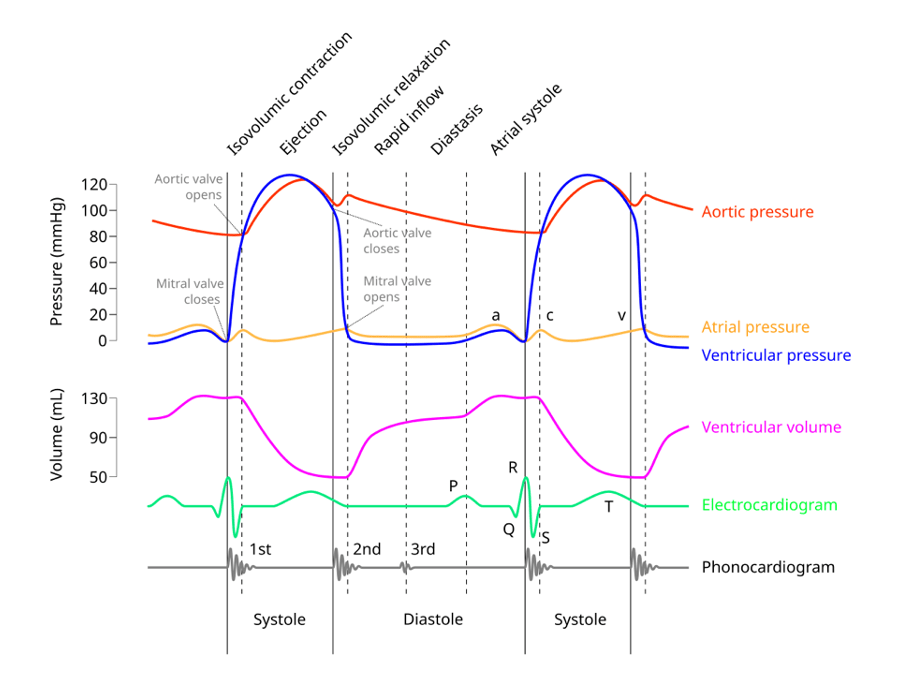
Question 130:
Answer: D) Atrial contraction phase
Explanation: The mitral and tricuspid valves open during the atrial contraction phase of the Wiggers diagram. This phase occurs after the P-wave and represents atrial systole, during which the atria contract, pushing blood through these valves into the ventricles. Understanding when these valves open is essential for assessing atrial function and diagnosing conditions like mitral valve stenosis or regurgitation.
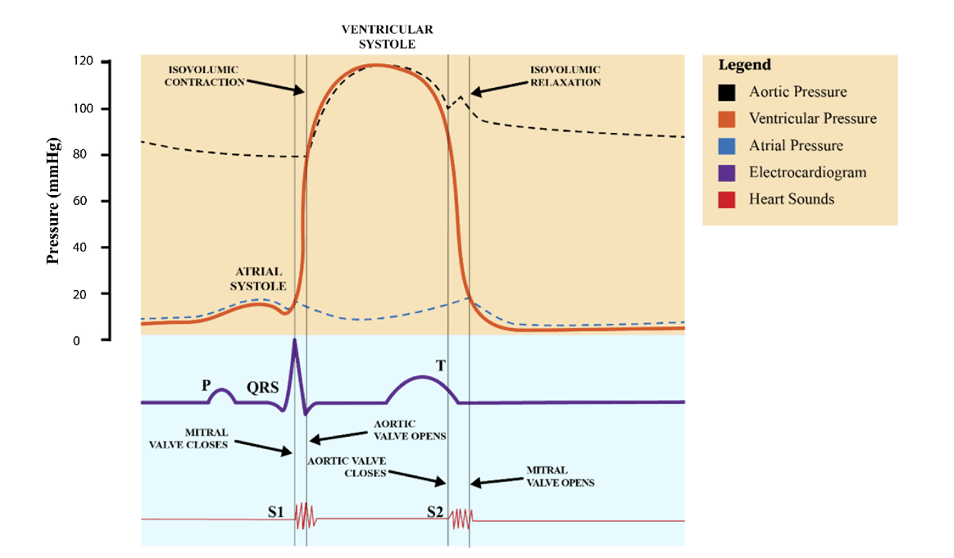
Question 131:
Answer: A) Ventricular ejection phase
Explanation: The aortic and pulmonary valves open during the ventricular ejection phase in the Wiggers diagram. This phase occurs after the QRS complex, representing the period when the ventricles contract and generate enough pressure to open these semilunar valves, enabling the ejection of blood into the systemic and pulmonary circulations. Understanding this phase is crucial for assessing ventricular contractility and diagnosing conditions related to these valves, such as aortic stenosis or pulmonary hypertension.
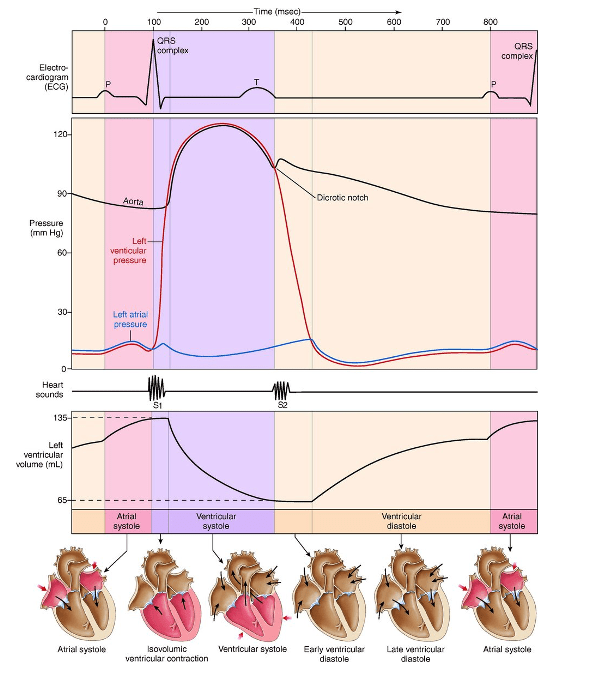
Question 132:
Answer: C) Isovolumetric contraction phase
Explanation: The isovolumetric contraction phase in the Wiggers diagram represents the moment when all four heart valves (mitral, tricuspid, aortic, and pulmonary) are closed, and the ventricles are contracting with increasing pressure. During this phase, no blood is being ejected yet because the ventricular pressure has not surpassed the pressure in the aorta and pulmonary artery. Understanding this phase is essential for assessing ventricular function and diagnosing conditions like hypertrophic cardiomyopathy, which can affect this phase.
Option A is incorrect because the ventricular ejection phase is when the pressure in the ventricles exceeds the pressure in the aorta and pulmonary artery, causing the aortic and pulmonary valves to open and blood to be ejected from the heart.
Option B is incorrect because the ventricular relaxation phase, or diastole, is when the ventricles are relaxing and filling with blood from the atria. During this phase, the pressure in the ventricles decreases.
Option D is incorrect because the atrial contraction phase refers to the atria contracting to push blood into the ventricles, occurring at the end of diastole, not during ventricular contraction.
Option E is incorrect because the isovolumetric relaxation phase occurs after the ventricular ejection phase, when the ventricles relax and all valves are closed, leading to a decrease in ventricular pressure without any change in ventricular volume.
Isovolumetric = all 4 valves are closed.
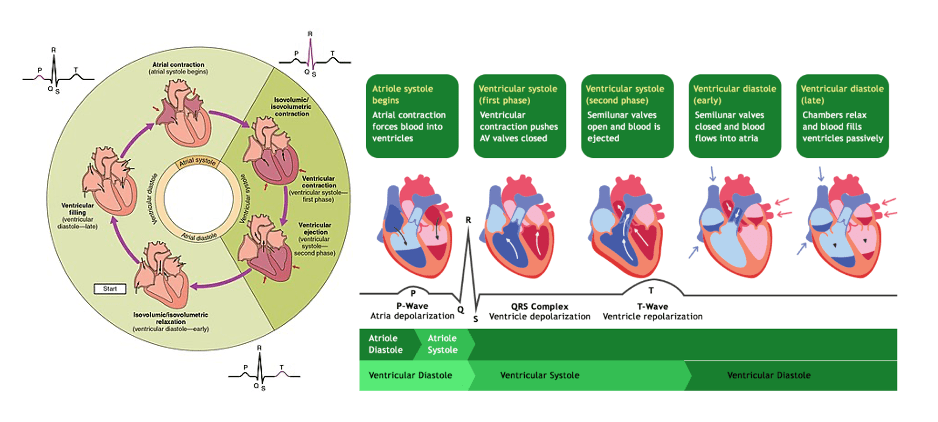
Question 133:
Answer: A) The mitral valve prevents backflow into the left atrium during systole; mitral regurgitation leads to increased left atrial pressure and pulmonary oedema.
Explanation: The primary role of the mitral valve is to prevent the backflow of blood from the left ventricle into the left atrium during ventricular systole, ensuring that blood flows unidirectionally from the left atrium to the left ventricle during diastole. Mitral regurgitation occurs when the mitral valve does not close properly, allowing blood to leak back into the left atrium during systole. This leads to increased pressure in the left atrium, which can cause pulmonary congestion and oedema.
Option B is incorrect because the mitral valve does not allow unidirectional flow into the left atrium during systole; instead, it prevents backflow. Mitral regurgitation would not lead to decreased left ventricular preload but rather to volume overload in the left atrium.
Option C is incorrect because the mitral valve is not involved with preventing backflow into the right atrium; this is the function of the tricuspid valve.
Option D is incorrect because the mitral valve allows unidirectional flow from the left atrium to the left ventricle during diastole, not into the left atrium. Mitral regurgitation does not lead to increased left ventricular afterload but causes increased left atrial pressure.
Option E is incorrect because the mitral valve prevents backflow into the left atrium during systole, not into the left ventricle during diastole. Mitral regurgitation would increase left atrial pressure, not decrease it, and lead to pulmonary oedema rather than systemic oedema.
Question 134:
Answer: C) During ventricular ejection
Explanation: The aortic and pulmonary valves open during the ventricular ejection phase of the cardiac cycle. This occurs after the ventricles have contracted, generating enough pressure to overcome the resistance in the aorta and pulmonary artery, allowing blood to be ejected into the systemic and pulmonary circulations.
Note: in isovolumetric phases, all valves are closed.
Option A is incorrect because atrial systole refers to the contraction of the atria, not the ventricles. This causes the AV valves to open, not aortic & pulmonary valves.
Option B is incorrect because isovolumetric relaxation is the phase when the ventricles relax and the semilunar valves close, not open. During this phase, no blood is being ejected.
Option D is incorrect because atrial diastole refers to the relaxation of the atria, not the phase when the semilunar valves open.
Option E is incorrect because isovolumetric contraction is the phase when the ventricles begin to contract, but the pressure is not yet high enough to open the semilunar valves. The semilunar valves remain closed during this phase.
Question 135:
Answer: B) Carotid sinus
Explanation: Baroreceptors are specialised sensory receptors located in the walls of certain blood vessels, including the aorta and carotid sinus. They play a crucial role in monitoring changes in blood pressure. When blood pressure increases or decreases beyond normal limits, carotid sinus receptors (found in the cardiovascular system, specifically in the neck close to the carotid artery) detect these change & sends impulses to the cardiovascular centre in the medulla oblongata. This feedback mechanism helps regulate blood pressure by adjusting heart rate, stroke volume, and vascular resistance to maintain homeostasis.
Option A is incorrect because aortic bodies are chemoreceptors that detect changes in blood chemistry, such as oxygen and carbon dioxide levels, rather than blood pressure.
Option C, while correct in identifying baroreceptors as the primary sensors for blood pressure changes, is less specific than option B. Carotid sinus receptors specifically refer to baroreceptors located in the cardiovascular system.
Option D is incorrect because Pacinian corpuscles are mechanoreceptors found in the skin and other tissues that detect changes in pressure and vibration.
Option E is incorrect because mechanoreceptors detect mechanical changes such as stretch and pressure in various tissues, including the lungs (preventing over-inflation of the lungs).
Question 136:
Answer: E) Aortic bodies
Explanation: Aortic bodies are sensory receptors located near the aortic arch. They primarily sense changes in blood oxygen (O2) levels, carbon dioxide (CO2) levels, and blood pH. These receptors are important for regulating ventilation (breathing rate) by sending signals to the respiratory centres in the brainstem. When blood O2 levels drop or CO2 levels rise, aortic bodies initiate adjustments in ventilation to ensure adequate oxygen supply and carbon dioxide removal.
Option A is incorrect because free nerve endings are general sensory receptors that detect pain, temperature, and other stimuli.
Option B is incorrect because the carotid sinus contains baroreceptors that detect changes in blood pressure, not blood oxygen or carbon dioxide levels.
Option C is incorrect because baroreceptors are responsible for detecting changes in blood pressure.
Option D is incorrect because Ruffini endings are mechanoreceptors that detect sustained pressure and skin stretch.
Question 137:
Answer: D) Endothelins induce vasoconstriction and are synthesised in endothelial cells.
Explanation: Endothelins are vasoactive peptides primarily synthesised and released by endothelial cells lining blood vessels. Their main role during the vascular phase of haemostasis is to induce vasoconstriction. This vasoconstriction helps in reducing blood flow to the injured area, contributing to haemostasis and minimising blood loss.

Question 138:
Answer: C) Heparin is derived from mast cells and activates antithrombin III, preventing blood clot formation.
Explanation: Heparin is primarily derived from mast cells and serves as a potent anticoagulant. Its main function in the context of hemostasis is to activate antithrombin III, an endogenous anticoagulant. By binding to antithrombin III, heparin enhances its inhibitory activity against several clotting factors and thrombin, effectively preventing blood clot formation.
Option A is incorrect because heparin is not synthesised in the liver; it is derived from mast cells.
Option B is incorrect because heparin does not promote platelet aggregation; it inhibits clot formation.
Option D is incorrect because heparin is not found in red blood cells; it is primarily derived from mast cells.
Option E is incorrect because heparin is not a medication that activates thrombin; instead, it inhibits thrombin and other coagulation factors.
Question 139:
Answer: B) Warfarin inhibits the synthesis of vitamin K-dependent clotting factors and its antagonist is vitamin K.
Explanation: Warfarin acts as an anticoagulant by inhibiting the synthesis of vitamin K-dependent clotting factors, including factors II, VII, IX, and X. Its antagonist is vitamin K, which is essential to produce these clotting factors. Administering vitamin K can counteract the effects of warfarin and restore normal clotting factor function.
Option A is incorrect because warfarin does not inhibit platelet aggregation; that role is associated with aspirin, which inhibits cyclooxygenase.
Option C is incorrect because warfarin does not prevent fibrin formation; that role is more related to antithrombin and heparin.
Option D is incorrect because warfarin does not enhance clot stabilisation; that function is associated with fibrinogen and platelet aggregation.
Option E is incorrect because warfarin does not enhance clot production; instead, it inhibits the production of clotting factors.
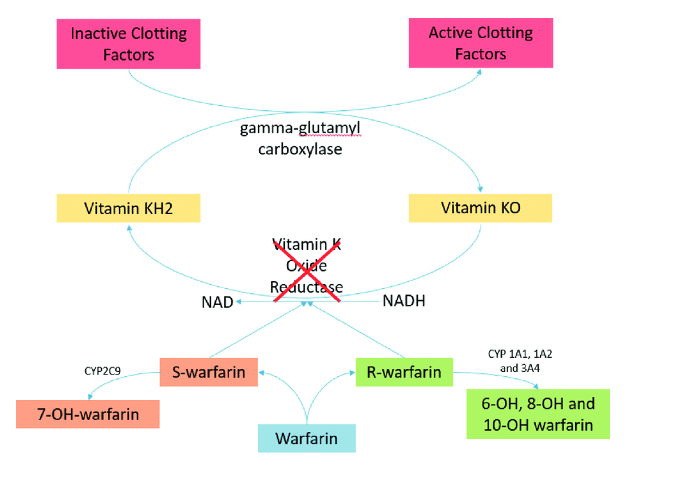
Question 140:
Answer: B) The AV node delays the electrical impulse briefly to allow for atrial contraction before ventricular contraction.
Explanation: The AV node is a critical component of the cardiac conduction system. It delays the electrical impulse briefly after receiving it from the SA node, allowing the atria to contract and push blood into the ventricles before ventricular contraction. This delay ensures efficient filling of the ventricles and proper coordination between atrial and ventricular contractions.
Option A is incorrect because the sinoatrial (SA) node, not the AV node, is responsible for initiating the electrical impulse that triggers each heartbeat.
Option C is incorrect because while the AV node can serve as a backup pacemaker, its primary role is not as a backup to the SA node.
Option D is incorrect because the AV node does not speed up the electrical impulse; instead, it delays it.
Option E is incorrect because the AV node does not relay the electrical impulse to the sinoatrial node (SAN); instead, it relays it to the bundle of His, which then distributes the impulse to the ventricles.
Question 141:
Answer: D) HCN channels allow for sodium and potassium ion movement, contributing to the gradual depolarisation in pacemaker cells.
Explanation: HCN channels play a crucial role in pacemaker cells by allowing both sodium (Na⁺) and potassium (K⁺) ions to pass through their pores. This unique property contributes to the gradual depolarisation of the pacemaker potential via the If current, which eventually reaches the threshold for action potential initiation. As these channels open, sodium ions enter the cell, depolarising it, and then potassium ions exit, repolarising it, resulting in the rhythmic firing of action potentials in pacemaker cells.
Option A is incorrect because HCN channels do not generate action potentials themselves; rather, they contribute to the pacemaker potential – the funny current – that leads to action potential generation.
Option B is incorrect because while HCN channels do help maintain the membrane potential near threshold, their primary role is not to stabilise the resting membrane potential.
Option C is incorrect because HCN channels primarily conduct sodium and potassium ions (the “funny current”) rather than calcium ions during the depolarization phase of the pacemaker potential.
Option E is incorrect because HCN channels do not bind to HCN; rather, they are gated by cyclic nucleotides and contribute to the funny current that leads to gradual depolarisation.
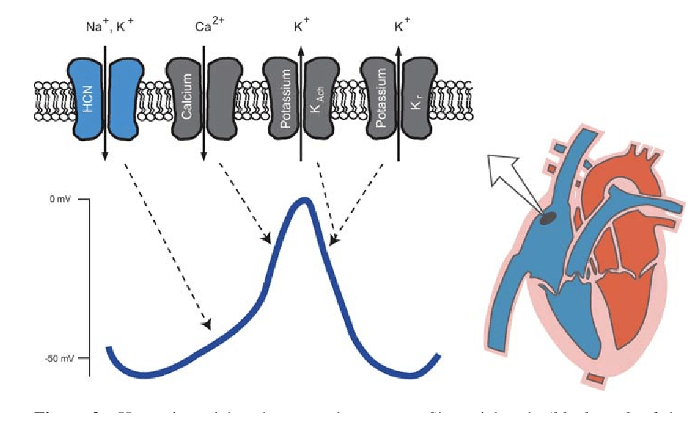
Question 142:
Answer: B) Sympathetic stimulation steepens phase 4 depolarisation, leading to a faster heart rate.
Explanation: Sympathetic stimulation, typically mediated by the release of norepinephrine, increases the rate of phase 4 depolarisation in pacemaker cells. This effect results in a faster spontaneous firing rate of action potentials in the SA node, leading to an increased heart rate. The sympathetic nervous system’s influence on phase 4 depolarisation is an essential mechanism for regulating heart rate in response to physiological demands, such as exercise or stress.
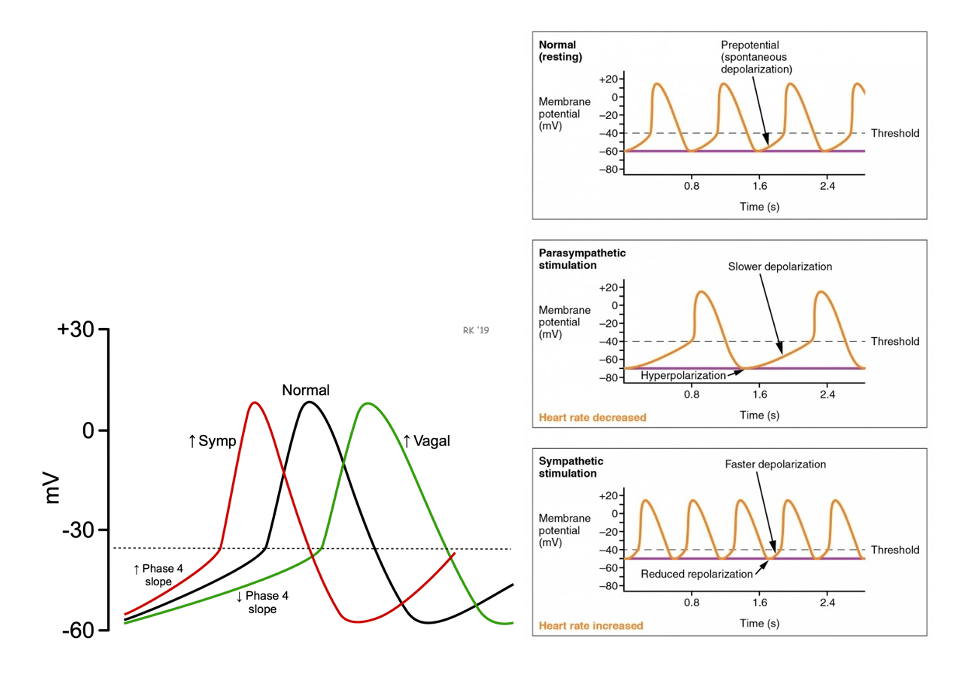
Question 143:
Answer: D) Parasympathetic stimulation makes phase 4 less steep, which slows down the heart rate.
Explanation: Parasympathetic stimulation primarily acts on pacemaker cells in the heart via the vagus nerve, releasing acetylcholine, which interacts with muscarinic receptors. This interaction increases potassium (K⁺) efflux during phase 3 repolarisation and decreases the influx of sodium (Na⁺) and calcium (Ca²⁺) ions. The increased potassium efflux leads to a less steep phase 3 repolarisation, meaning the cells take longer to reach the threshold for the next action potential. This effect decreases the rate of depolarisation, leading to a slower heart rate (bradycardia).
Option A is incorrect because parasympathetic stimulation does not accelerate phase 3 repolarisation. Instead, it slows down the rate of repolarisation, making phase 3 less steep, which contributes to a slower heart rate rather than a faster one.
Option B is incorrect because parasympathetic stimulation does not steepen phase 3 repolarisation. Steepening would imply a faster transition to the resting potential, which would increase the heart rate. However, parasympathetic effects actually make phase 3 less steep, slowing down the repolarisation process.
Option C is incorrect because parasympathetic stimulation does affect phase 3 of pacemaker cells. It plays a crucial role in modulating the heart rate by altering the dynamics of phase 3 repolarisation, making it less steep and thus slowing the heart rate.
Option E is incorrect because parasympathetic stimulation does not make phase 3 even or uniform in such a way that allows for simultaneous contraction. The concept of making phase 3 “even” does not align with the physiological mechanisms influenced by parasympathetic activity. Parasympathetic effects are aimed at slowing the rate of pacemaker cell depolarisation, leading to a decrease in heart rate.
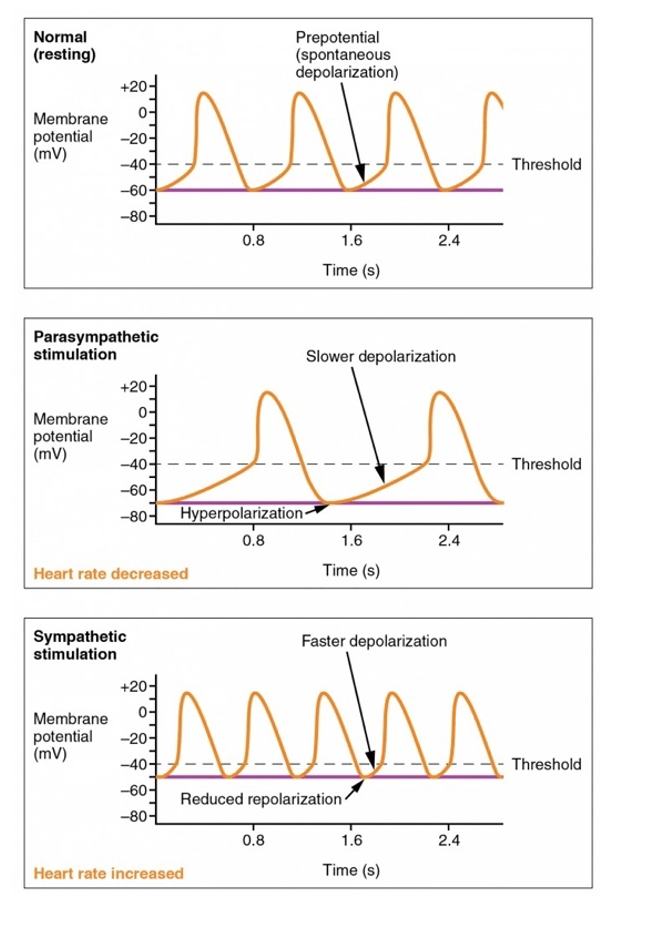
Question 144:
Answer: D) Sternopericardial ligament
Explanation: The Sternopericardial ligament connects the posterior surface of the sternum to the pericardium and is responsible for helping to maintain the position of the heart within the mediastinum. This ligament plays a role in preventing excessive movement or displacement of the heart within the chest cavity.
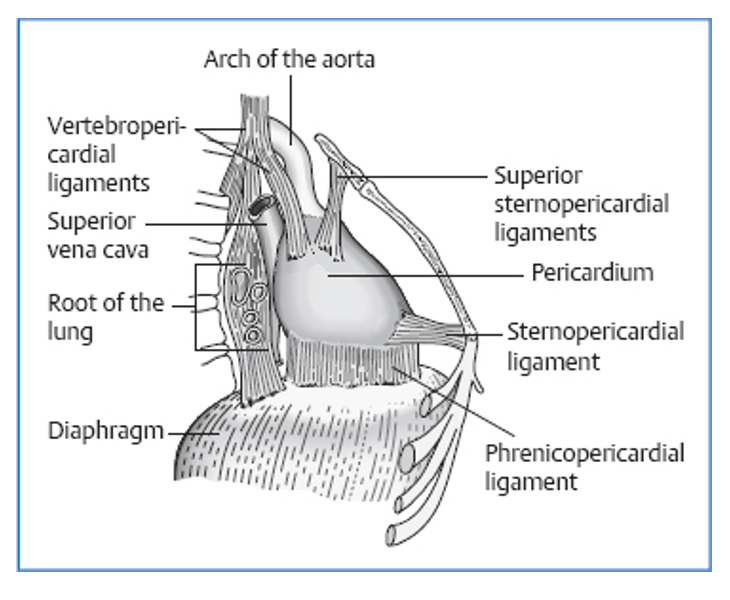
Question 145:
Answer: B) Stimulation of carotid sinus baroreceptors
Explanation: When you stand up suddenly, blood tends to pool in your legs due to gravity, potentially causing a drop in blood pressure. Carotid sinus baroreceptors, located in the carotid arteries, are highly sensitive to changes in blood pressure and play a crucial role in regulating it. When these baroreceptors sense a drop in blood pressure upon standing, they trigger reflex responses, such as increasing heart rate and constricting blood vessels, to counteract the decrease in blood pressure and maintain adequate blood flow to the brain. This mechanism helps prevent dizziness or fainting when transitioning from a seated or lying position to standing.
Option A is incorrect because while aortic arch baroreceptors are important for overall blood pressure regulation, the carotid sinus baroreceptors are more sensitive and crucial in detecting changes in blood pressure.
Option C is incorrect because the parasympathetic nervous system primarily regulates heart rate and gastrointestinal function, not rapid blood pressure adjustments related to posture changes.
Option D is incorrect because the renin-angiotensin-aldosterone system (RAAS) primarily regulates long-term blood pressure by modulating fluid balance and vascular tone, not immediate adjustments to posture.
Option E is incorrect because while noradrenaline release is involved in sympathetic nervous system responses to maintain blood pressure, it is not the primary mechanism for preventing rapid blood pressure decreases during postural changes.
Question 146:
Answer: D) Megakaryocytes
Explanation: Platelets, also known as thrombocytes, are derived from megakaryocytes, which are large, multinucleated cells found in the bone marrow. Megakaryocytes undergo a unique process of cytoplasmic fragmentation, producing numerous platelets from their cytoplasm. These platelets are essential for blood clotting and wound healing, as they aggregate at the site of injury to form a plug and initiate the clotting cascade. Other options like monocytes, erythrocytes, lymphocytes, and neutrophils are not the source of platelet production.
Question 147:
Answer: B) The Bohr effect shifts the oxygen dissociation curve to the right, decreasing oxygen affinity, while the chloride exchanges for bicarbonate out of red blood cells, facilitating oxygen release to muscle tissue.
Explanation: During exercise, muscle cells produce more carbon dioxide (CO2), leading to increased acidity. The Bohr effect causes a rightward shift in the oxygen dissociation curve, decreasing haemoglobin’s oxygen affinity, making it easier to release oxygen to metabolically active muscle tissue. Simultaneously, the chloride shift involves the exchange of chloride ions for bicarbonate ions in red blood cells, helping to transport CO2 away from muscle tissue, which is essential for pH regulation. This collective mechanism ensures efficient oxygen delivery and pH balance during exercise.
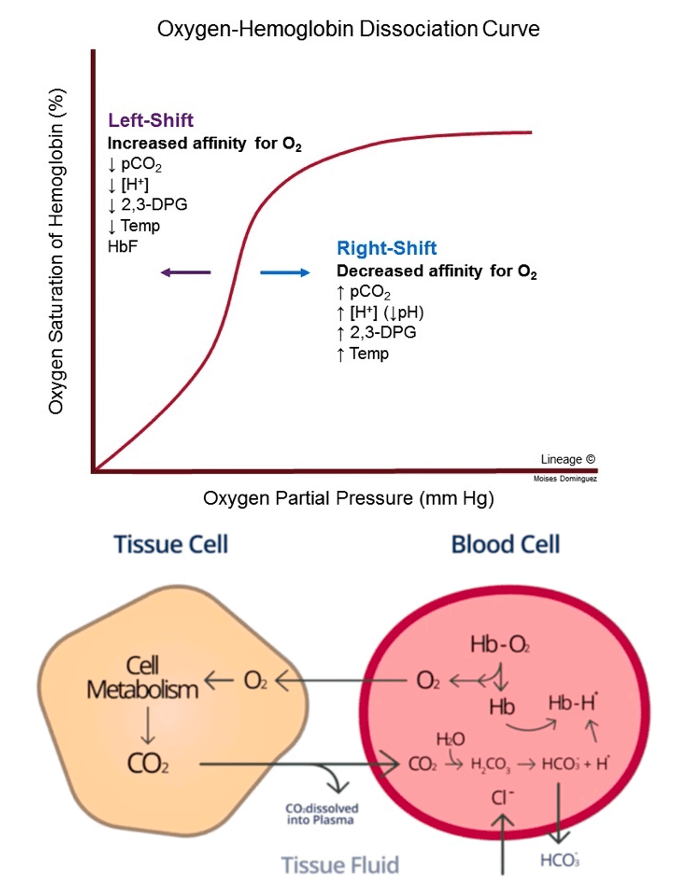
Question 148:
Answer: E) High levels of 2,3-diphosphoglycerate (2,3-DPG)
Explanation: Oxygen affinity of haemoglobin is influenced by various factors. One significant regulator is 2,3-diphosphoglycerate (2,3-DPG), a compound produced in red blood cells during glycolysis. High levels of 2,3-DPG, often seen in conditions like anaemia or at high altitudes, cause a rightward shift in the oxygen dissociation curve. This shift results in decreased oxygen affinity, making it easier for HbA to release oxygen to the tissues.
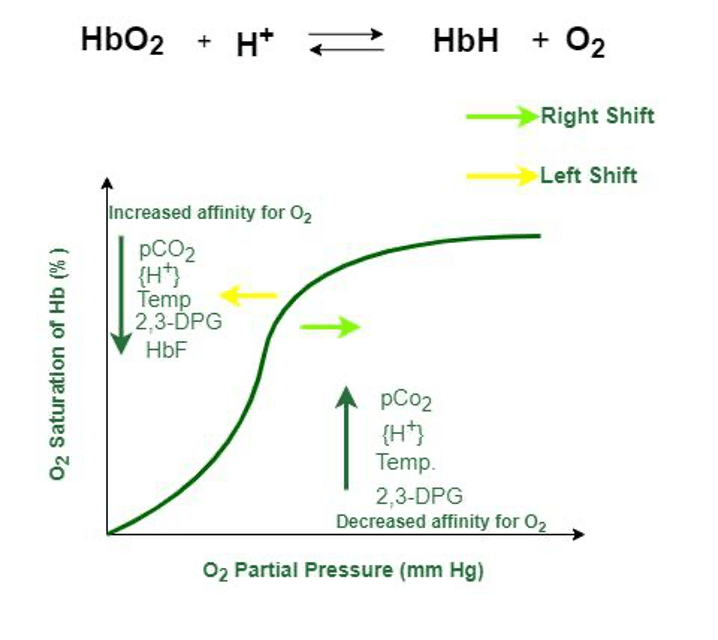
Question 149:
Answer: C) Heparin
Explanation: Heparin is released from mast cells and acts as a potent anticoagulant. It enhances the activity of antithrombin III, a natural inhibitor of blood clot formation. By binding to antithrombin III, heparin accelerates its ability to inactivate thrombin and other coagulation factors, thus preventing excessive clotting within the bloodstream. This anticoagulant property of heparin is utilized clinically to prevent and treat various thrombotic disorders.
Option A is incorrect because prostacyclin is a prostaglandin released from endothelial cells that inhibits platelet aggregation.
Option B is incorrect because while histamine is released from mast cells and plays a role in allergic reactions and inflammation, it is not involved in inhibiting blood clot formation.
Option D is incorrect because plasmin is a proteolytic enzyme involved in fibrinolysis, breaking down blood clots rather than preventing their formation.
Option E is incorrect because Von Willebrand factor is a glycoprotein involved in platelet adhesion (vWF binds platelets to underlying exposed collagen fibres).
Question 150:
Answer: D) By blocking sodium channels
Explanation: Local anaesthetics, such as lidocaine, primarily act by blocking sodium channels in nerve cells. They bind to these channels and prevent the influx of sodium ions, which are essential for the initiation and propagation of action potentials. By blocking sodium channels, local anaesthetics interrupt the transmission of pain signals and inhibit nerve cell excitation, leading to the temporary loss of sensation in the affected area.
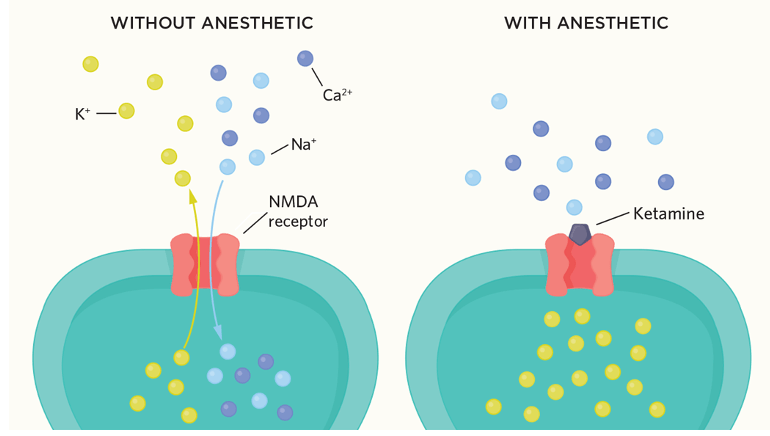
Question 151:
Answer: B) Calcium (Ca2+)
Explanation: Calcium ions (Ca2+) have been studied for their potential antihypertensive effects. Calcium channel blockers, which inhibit the entry of calcium into vascular smooth muscle cells and cardiomyocytes, can lead to vasodilation and decreased cardiac contractility, thereby reducing blood pressure. These medications are commonly used in the management of hypertension. Sodium channel blockers (e.g., class I antiarrhythmics) are primarily employed for the treatment of arrhythmias, whereas calcium channel blockers play a pivotal role in controlling hypertension.
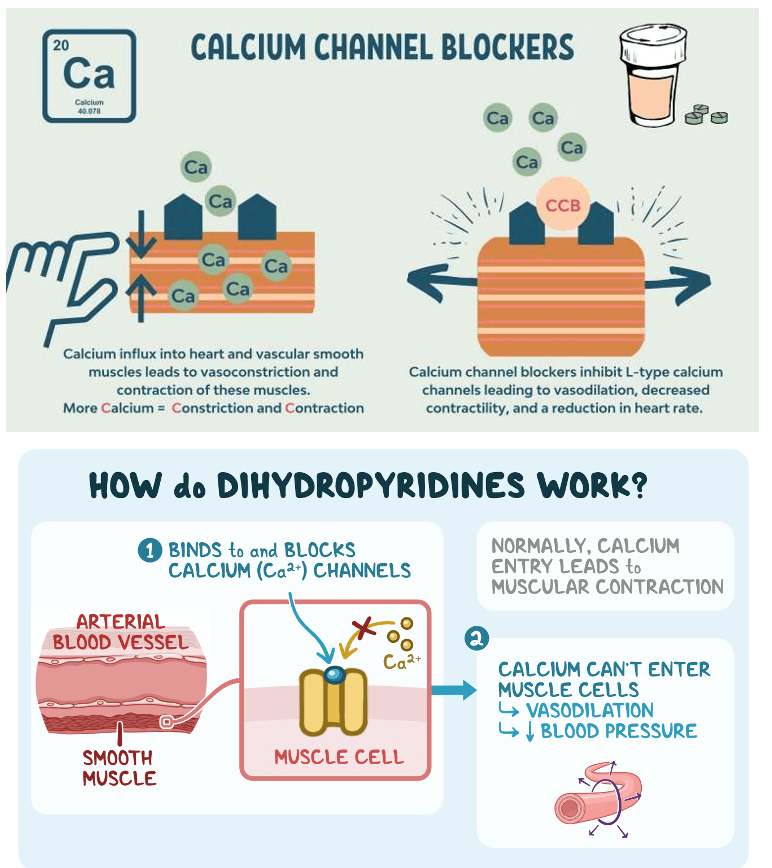
Question 152:
Answer: C) Sodium (Na+) and calcium (Ca2+)
Explanation: Antiarrhythmic therapies often target sodium and calcium ions to regulate cardiac action potentials and impulse conduction. Sodium channel blockers (Class I antiarrhythmics) primarily affect sodium influx during depolarisation, while calcium channel blockers (Class IV antiarrhythmics) impact calcium entry, especially during the plateau phase of cardiac action potentials (phase 2). These interventions help stabilize the heart’s rhythm and prevent various types of arrhythmias.
Remember, the NCX exchanger transports one calcium ion (Ca2+) out of the cardiocytes & 2 sodium ions (Na+) into the cardiocytes in order to remove calcium ions following contraction of the heart. Since there is a net positive charge of +1 into the cardiac myocytes, this may trigger depolarisation of the cells resulting in arrythmias.
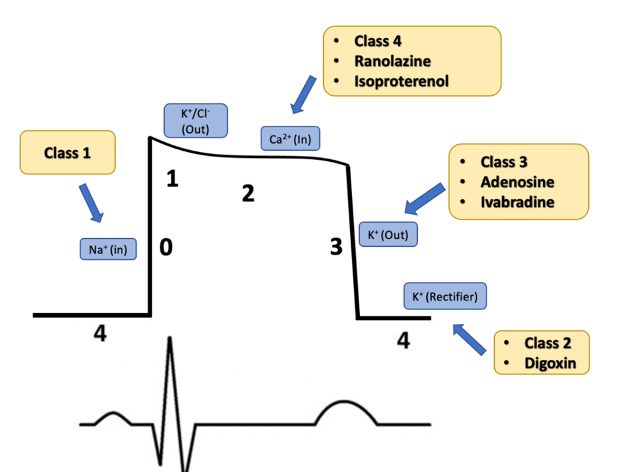
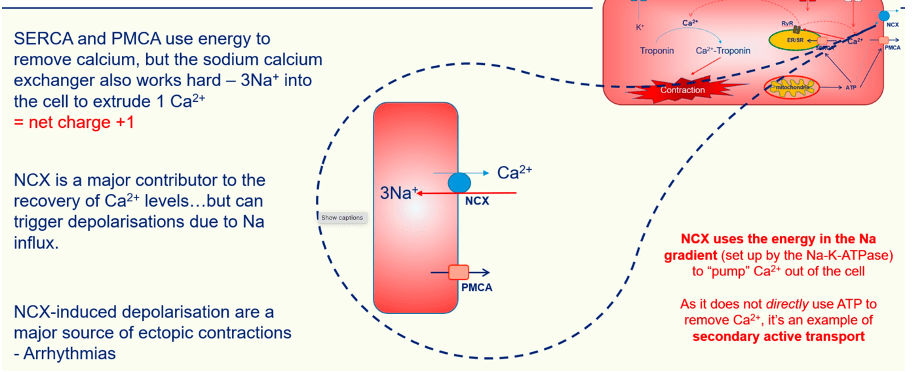

Question 153:
Answer: C) Increased ventilation and decreased perfusion
Explanation: In patients with chronic obstructive pulmonary disease (COPD), ventilation-perfusion coupling is a compensatory mechanism. It increases airflow (ventilation) to lung regions with compromised airways due to conditions like chronic bronchitis or emphysema. However, these regions may experience reduced blood flow (perfusion) due to damaged lung tissue. The body’s goal is to optimise gas exchange by increasing ventilation, but impaired perfusion can limit oxygen exchange efficiency. This phenomenon is essential to understand when managing COPD patients’ respiratory challenges.
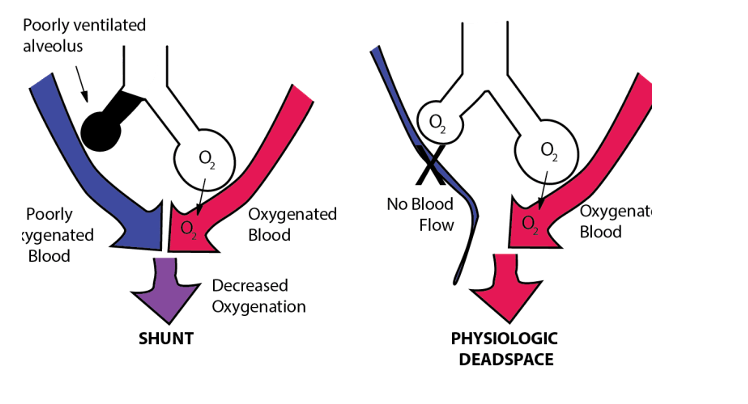
Question 154:
Answer: A) EF = Stroke volume / End-diastolic volume
Explanation: Ejection fraction (EF) is a crucial measure of cardiac function, indicating the heart’s ability to pump blood effectively. It represents the fraction of blood ejected from the left ventricle during each heartbeat.
The correct formula for calculating EF is EF = Stroke volume / End-diastolic volume. This formula compares the volume of blood ejected during systole (stroke volume) to the volume of blood in the ventricle at the end of diastole before contraction (end-diastolic volume). It expresses the result as a percentage.
Remember stroke volume is calculated by this equation: End-Diastolic Volume (EDV) – End-Systolic Volume (ESV)
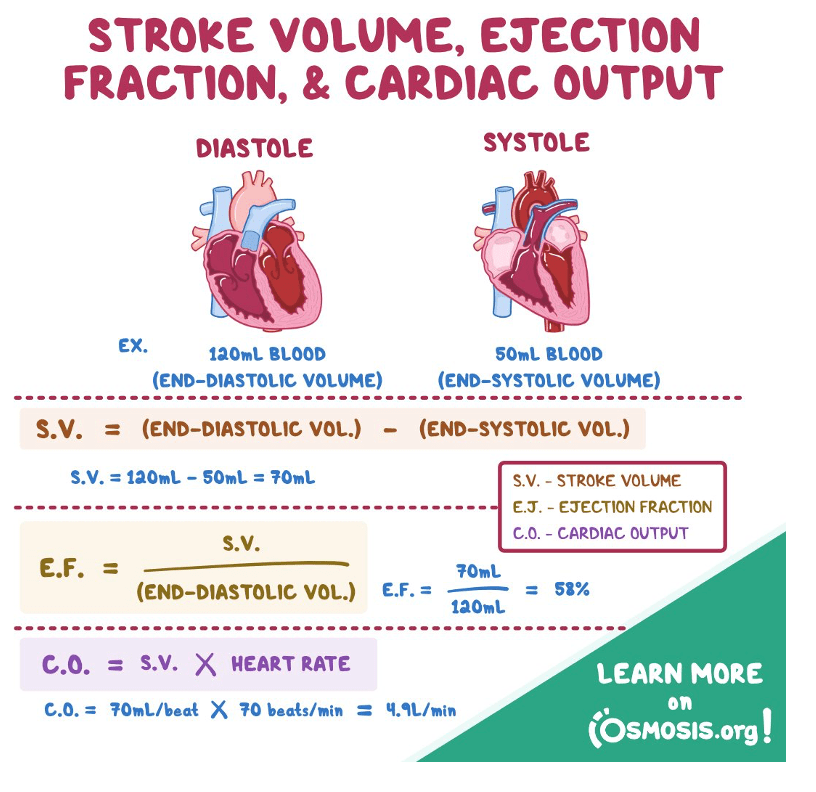
Question 155:
Answer: D) Lactate
Explanation: During strenuous exercise, the heart’s demand for energy increases significantly. While fatty acids are the heart’s primary energy source under normal conditions, when oxygen supply becomes limited, as is often the case during heavy exercise, the heart shifts to utilising lactate as a vital energy source.
This metabolic adaptation allows the heart to continue pumping efficiently in oxygen-deprived conditions. Lactate is produced in skeletal muscles as a by-product of anaerobic glycolysis and is transported to the heart, where it is converted back into pyruvate and enters the citric acid cycle to generate ATP, providing the necessary energy for continued cardiac contractions.
Fatty acids are the primary fuel source for the heart under normal aerobic conditions but are less utilised when oxygen supply is limited.
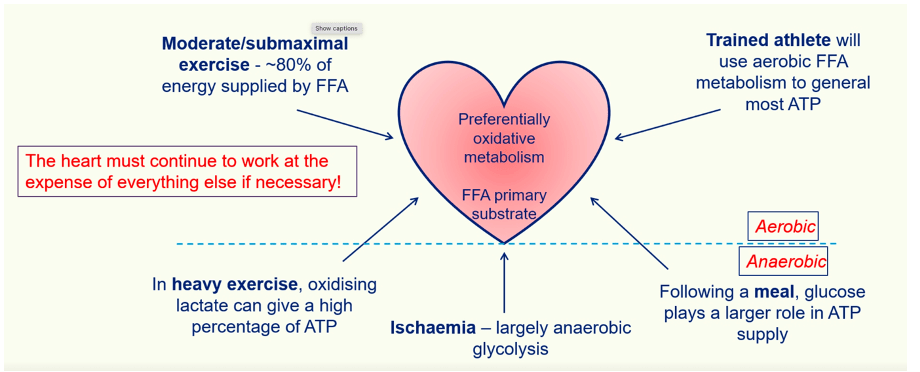
Question 156:
Answer: E) After a meal when glucose levels are elevated
Explanation: Following a meal, the elevated glucose levels in the bloodstream provide an abundant source of energy for various tissues, including the heart. During this period, the heart may use more glucose to meet its energy demands. However, Free fatty Acids still is the most efficient and widely used energy source of the heart and in circumstances of low FFA the heart may use more glucose.

Question 157:
Answer: C) Calcium (Ca2+)
Explanation: In excitation-contraction coupling in cardiac muscle cells, calcium (Ca2+) is a pivotal ion. When an action potential spreads across the cardiac cell membrane, this triggers the release of calcium ions via L-type channels (aka dihydropyridine receptor channels) from the extracellular space. The rise in intracellular calcium ion concentration further triggers the release of calcium ions from the sarcoplasmic reticulum via ryanodine receptor channels. These calcium ions then bind to troponin, leading to a conformational change in the troponin-tropomyosin complex, which allows actin and myosin to interact and initiate muscle contraction. The contraction of cardiac muscle is highly dependent on the regulation of intracellular calcium levels. Therefore, calcium is essential for the contractility of the heart.
Additionally, calcium is involved in various other processes in cardiac function, such as the regulation of ion channels, including L-type calcium channels, which are crucial for the action potential. This intricate control of calcium is vital for the precise timing and coordination of cardiac muscle contraction and relaxation.
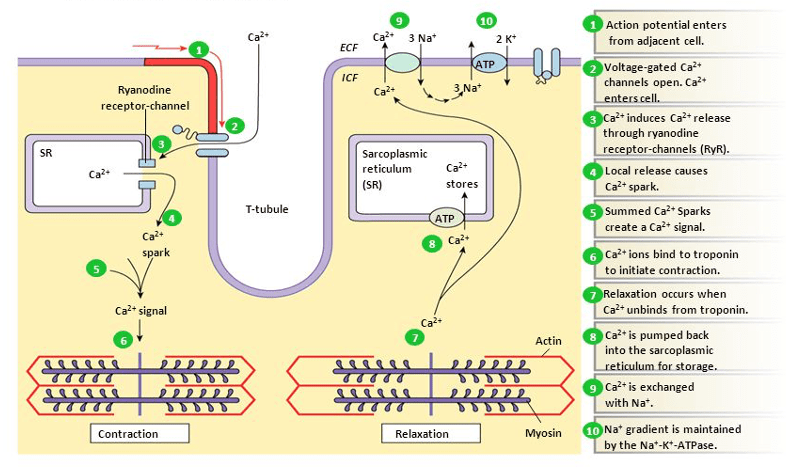
Question 158:
Answer: B) Preload
Explanation: Preload refers to the force exerted on the left ventricle of the heart immediately before it contracts. It is mainly determined by the volume of blood in the ventricle at the end of diastole. An increase in preload, often associated with an increased venous return to the heart, results in a greater stretch of the cardiac muscle fibres. This increased stretch enhances the force of contraction during systole, allowing the heart to pump a larger volume of blood.
Preload is a crucial factor in the Frank-Starling mechanism, which states that the stroke volume of the heart is directly proportional to its initial diastolic volume (preload). Understanding preload is essential for assessing and managing conditions such as heart failure, where optimising preload can improve cardiac output.
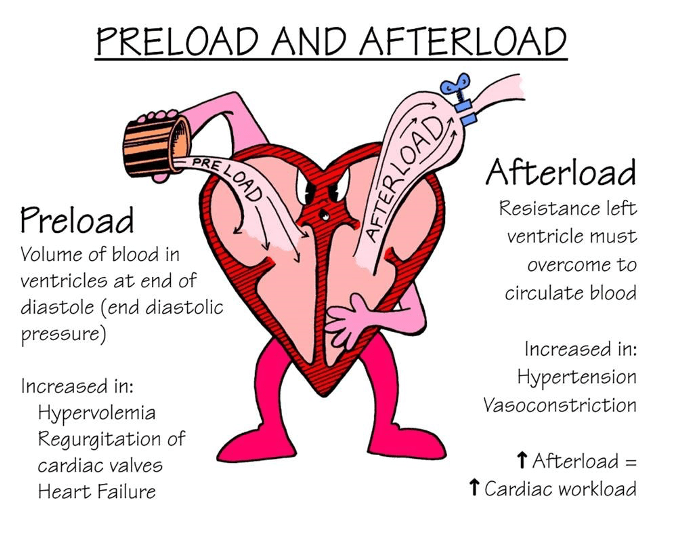
Question 159:
Answer: C) Beta-1 adrenergic receptor
Explanation: The Beta-1 adrenergic receptor is primarily responsible for increasing intracellular calcium levels in cardiac myocytes. When activated by norepinephrine or epinephrine, Beta-1 receptors stimulate the adenylate cyclase-cAMP (Gs) pathway, leading to increased calcium influx during the plateau phase of the cardiac action potential. This results in enhanced contractility of the heart.
Beta-1 adrenergic receptors are predominantly found in cardiac tissue, making them a key target for sympathetic stimulation and the regulation of heart rate and contractility. Activation of these receptors plays a crucial role in the body’s response to stress or increased demand for cardiac output.
Option A is incorrect because Alpha-1 adrenergic receptors cause vasoconstriction in blood vessels.
Option B is incorrect because Alpha-2 adrenergic receptors are primarily inhibitory autoreceptors located on presynaptic nerve terminals and other tissues. Their activation leads to a decrease in neurotransmitter release, including norepinephrine, thereby exerting a negative feedback control on sympathetic activity.
Option D is incorrect because Beta-2 adrenergic receptors are found in bronchial smooth muscle cells and blood vessels. Their activation leads to bronchodilation and vasodilation, which are important responses during sympathetic activation to increase airway diameter and blood flow to muscles.
Option E is incorrect because dopamine receptors, specifically the dopamine-1 (D1) subtype, primarily mediate vasodilation in renal, coronary, and mesenteric blood vessels. Their activation increases renal blood flow and promotes natriuresis.
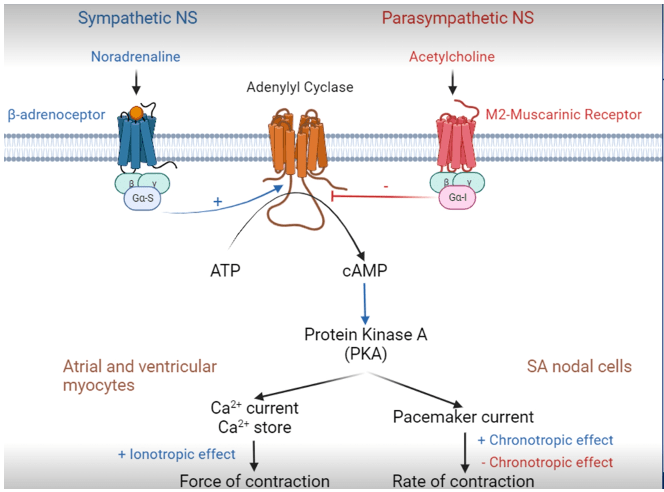
Question 160:
Answer: B) Sympathetic nervous system
Explanation: The sympathetic nervous system is primarily responsible for increasing heart rate and contractility in response to stress or increased demand. This system releases norepinephrine and epinephrine, which bind to Beta-1 adrenergic receptors in the heart, leading to increased intracellular calcium levels and enhanced contractility. It also accelerates the heart rate by affecting the SA (sinoatrial) node, the heart’s natural pacemaker.
Conversely, the parasympathetic nervous system (A) opposes these effects by releasing acetylcholine, which binds to muscarinic receptors and slows down the heart rate. The enteric nervous system (C) primarily regulates the digestive tract, the somatic nervous system (D) controls voluntary muscle movements, and the central nervous system (E) includes the brain and spinal cord, which coordinate overall body functions.
Question 161:
Answer: D) It states that stroke volume increases with increasing preload, up to a certain point.
Explanation: Starling’s law of the heart, also known as the Frank-Starling mechanism, describes the relationship between the preload (end-diastolic volume) of the heart and stroke volume. According to this law, as preload increases, stroke volume also increases, up to a certain point. This phenomenon occurs because an increased preload leads to greater stretch of cardiac muscle fibres, resulting in a more forceful contraction during systole.
However, beyond a certain point, further increases in preload may not lead to a proportional increase in stroke volume, and the heart may reach its maximum capacity. This principle is vital for understanding cardiac physiology and how the heart adapts to changes in venous return and blood volume.
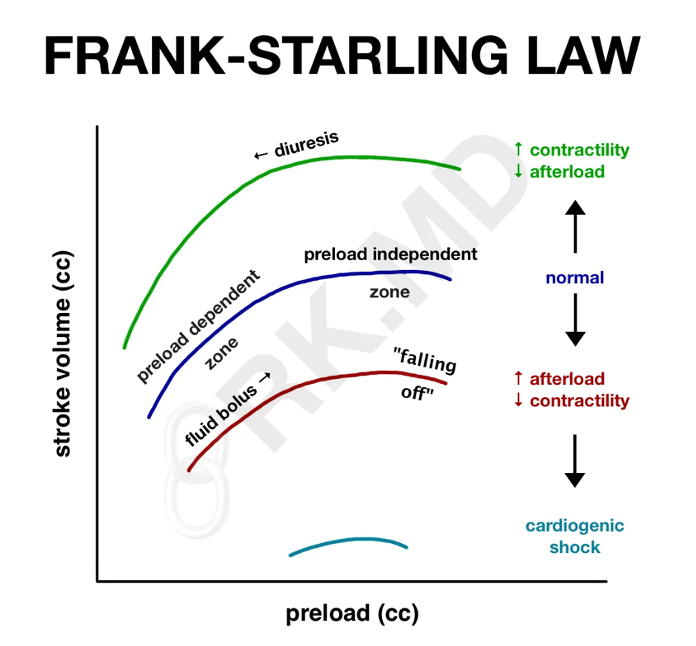
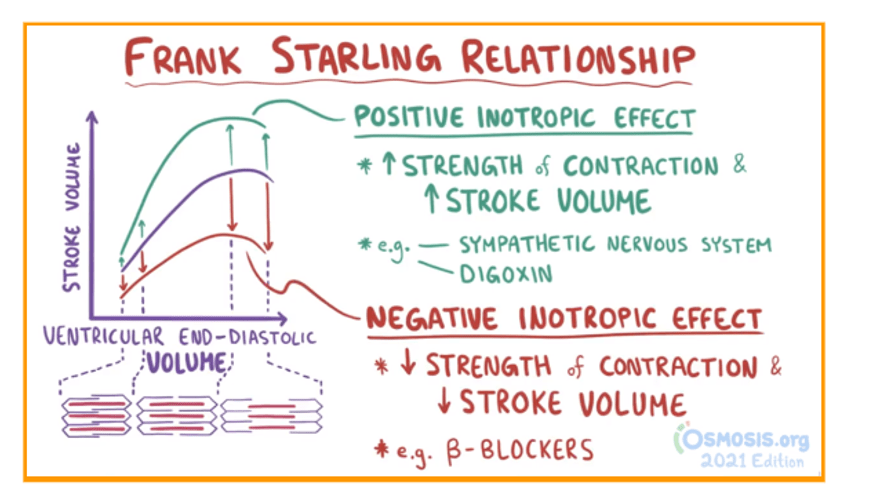
Question 162:
Answer: B) Afterload
Explanation: Afterload refers to the resistance that the left ventricle of the heart must overcome to eject blood into the systemic circulation. It is primarily determined by the systemic vascular resistance, which includes the resistance in the arteries and arterioles throughout the body. Increased afterload can make it more difficult for the heart to pump blood, potentially leading to increased myocardial workload and reduced stroke volume.
Understanding afterload is crucial in conditions like hypertension, where elevated systemic vascular resistance can place greater stress on the heart. Medications targeting afterload reduction may be used to manage such conditions and improve cardiac function.
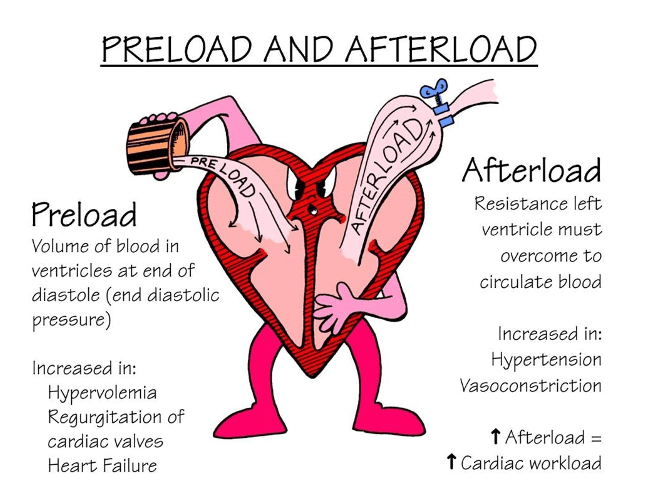
Question 163:
Answer: C) Visceral pericardium
Explanation: The visceral pericardium, also known as the epicardium, is the layer of the pericardium that is directly attached to the heart muscle. It provides a protective covering for the outer surface of the heart and is closely adhered to the myocardium.

Question 164:
Answer: D) Lateral plate mesoderm
Explanation: The heart is derived from the lateral mesoderm during embryological development. It begins as a simple tube and undergoes complex morphological changes to develop into the mature, four-chambered organ we have in adulthood. During embryological development, the heart initially forms from the lateral plate mesoderm. This layer of mesoderm splits into two layers: the somatic mesoderm (which forms the outer body wall) and the splanchnic mesoderm (which forms the wall of the gut). The splanchnic mesoderm gives rise to the cardiac mesoderm, which later develops into the heart tube and subsequently into the mature heart.
Option A is incorrect because the endoderm gives rise to the epithelial lining of the digestive and respiratory tracts, as well as associated organs such as the liver and pancreas, but not the heart.
Option B is incorrect because the ectoderm forms the nervous system (both central and peripheral), as well as epithelial tissues such as the skin & eyes.
Option C is incorrect because the paraxial mesoderm gives rise to structures such as skeletal muscle, cartilage, and connective tissues along the axis of the embryo, including the somites.
Option E is incorrect because the intermediate mesoderm develops into urogenital structures, including the kidneys and reproductive organs, but not the heart.

Question 165:
Answer: D) Ligamentum arteriosum
Explanation: The ligamentum arteriosum is the remnant of the ductus arteriosus in the adult heart. During fetal development, the ductus arteriosus allows blood to bypass the non-functional fetal lungs by connecting the pulmonary artery to the aorta. After birth, the ductus arteriosus normally closes and becomes the ligamentum arteriosum. This closure is essential for redirecting blood flow to the lungs for oxygenation after birth.
Option A is incorrect because although the ductus arteriosus is the structure that connects the pulmonary artery to the aorta in a developing fetus, allowing most of the blood to bypass the non-functional fetal lungs, the remnant is ligamentum arteriosum.
Option B is incorrect because the fossa ovalis is a remnant of the foramen ovale, an opening between the right and left atria in the fetal heart. The foramen ovale allows blood to bypass the lungs during fetal development but closes after birth, forming the fossa ovalis.
Option C is incorrect because the ductus venosus is a fetal blood vessel that connects the umbilical vein to the inferior vena cava, allowing oxygenated blood from the placenta to bypass the liver and enter the fetal circulation.
Option E is incorrect because the ligamentum venosum is a remnant of the ductus venosus in the adult circulation, serving no role in fetal circulation.
Question 166:
Answer: C) Patent foramen ovale
Explanation: A patent foramen ovale (PFO) is a persistent opening between the right and left atria of the heart that typically closes shortly after birth. In some individuals, the foramen ovale may remain partially open or “patent” into adulthood. This opening is a remnant of fetal circulation and allows blood to bypass the lungs, as oxygenation primarily occurs in the placenta during fetal development.
Option A is incorrect because a patent ductus arteriosus is a persistent opening between the pulmonary artery and the aorta, allowing blood to bypass the lungs.
Option B is incorrect because a ventricular septal defect (VSD) is an abnormal opening in the septum between the right and left ventricles, not the atria.
Option D is incorrect because aortic stenosis is a condition where the aortic valve is narrowed, affecting blood flow from the left ventricle to the aorta.
Option E is incorrect because Tetralogy of Fallot is a congenital heart defect involving four specific abnormalities in the heart’s structure, not an atrial opening.
Question 167:
Answer: D) Prostaglandin E2 (PGE2)
Explanation: After birth, the ductus arteriosus closes due to a decrease in the concentration of PGE2. In fetal circulation, PGE2 helps maintain patency of the ductus arteriosus, allowing blood to bypass the non-functional fetal lungs. Upon birth, a decrease in PGE2 levels and an increase in oxygen tension trigger the closure of the ductus arteriosus.
Option A, Prostacyclin, is incorrect because prostacyclin (PGI2) primarily acts as a vasodilator and inhibitor of platelet aggregation.
Option B, Prostaglandin E1 (PGE1), is incorrect because PGE1 is a vasodilator and is used clinically to maintain patency of the ductus arteriosus in certain medical conditions, rather than promoting its closure.
Option C, Arachidonic acid, is incorrect because it is a precursor molecule involved in the synthesis of various eicosanoids, including prostaglandins, but its decrease alone does not directly cause closure of the ductus arteriosus.
Option E, Cyclooxygenase (COX), is incorrect because COX is the enzyme responsible for the synthesis of prostaglandins from arachidonic acid, rather than being directly responsible for the closure of the ductus arteriosus.

Question 168:
Answer: D) Creation of the interventricular septum
Explanation: The fusion of the endocardial tubes during embryological development is a crucial step in the formation of the interventricular septum. This septum divides the primitive heart tube into two distinct ventricles, the left and right, allowing for the separation of oxygenated and deoxygenated blood and ensuring proper circulation in the mature heart.
Option A is incorrect because the atrioventricular valves develop from swellings in the endocardial cushions.
Option B is incorrect because coronary arteries arise from the sinus venosus and aortic sac during heart development.
Option C is incorrect because the cardiac conduction system, including the sinoatrial (SA) and atrioventricular (AV) nodes, forms separately and are not directly related to the fusion of endocardial tubes.
Option E is incorrect because the pericardium forms from mesodermal layers around the heart and is not directly influenced by the fusion of endocardial tubes.
Question 169:
Answer: D) Umbilical vein
Explanation: In the fetal circulation pathway in-utero, oxygenated blood from the placenta enters the fetal circulation through the umbilical vein. This oxygen-rich blood is carried to the fetus and primarily enters the inferior vena cava through the ductus venosus. From there, it partially bypasses the fetal liver and enters the right atrium.
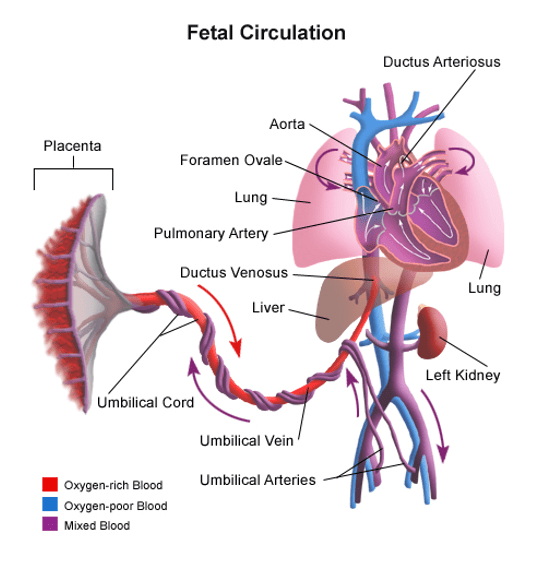
Question 170:
Answer: C) 1 umbilical vein & 2 umbilical arteries
Explanation: The developing fetus has 1 umbilical vein carrying oxygenated blood, nutrients, glucose, maternal antibodies etc. from the mother towards the placenta & 2 umbilical arteries carrying deoxygenated blood, carbon dioxide & waste products from the fetus towards the placenta (back to mother’s circulation in order to be oxygenated again).
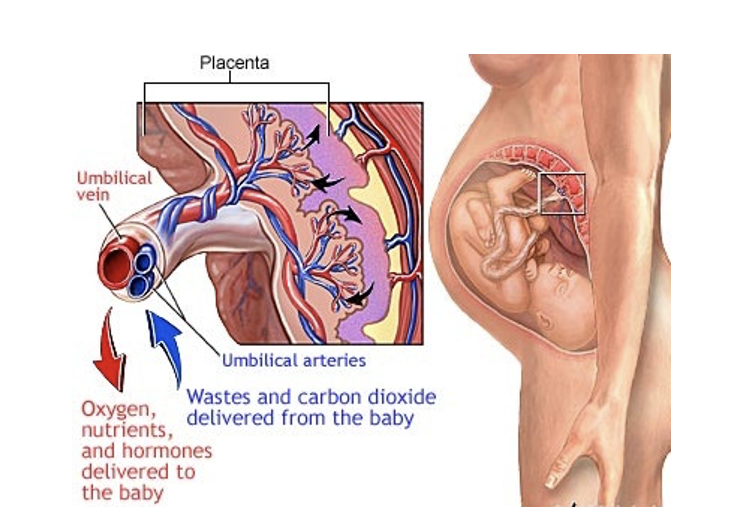
Question 171:
Answer: D) Middle mediastinum
Explanation: The heart is located in the middle mediastinum, which is the central compartment of the thoracic cavity and contains the heart, pericardium, and the roots of the great vessels (aorta, pulmonary arteries, superior and inferior vena cava).
It is primarily responsible for housing the heart and providing a protective environment for it within the thorax. The pericardial cavity within this compartment allows the heart to move and contract without friction against other thoracic organs.
Option A is incorrect because the superior mediastinum is located above the heart and contains structures such as the thymus, parts of the aorta, oesophagus, trachea, thoracic duct, and several important nerves (like the vagus and phrenic nerves). While it houses major blood vessels and structures, it does not contain the heart itself.
Option B is incorrect because the inferior mediastinum is divided into three parts: anterior, middle, and posterior. Only the middle mediastinum within the inferior mediastinum contains the heart.
Option C is incorrect because the anterior mediastinum is the front portion of the inferior mediastinum, located between the sternum and the pericardium. It typically contains loose connective tissue, fat, lymphatic vessels, and sometimes remnants of the thymus.
Option E is incorrect because the posterior mediastinum is located behind the heart and contains structures such as the descending aorta, oesophagus, thoracic duct, azygos vein, and sympathetic nerves.

Question 172:
Answer: A) Simple squamous epithelium
Explanation: The endocardium is lined by simple squamous epithelium, known as the endothelium when it lines the heart and blood vessels. This thin layer of cells provides a smooth, friction-reducing surface for the inner chambers of the heart, facilitating efficient blood flow and minimizing turbulence within the heart. The simple squamous epithelium serves as a selective barrier, allowing nutrients and waste products to pass while maintaining the integrity of the underlying tissue.
Option B is incorrect because simple cuboidal epithelium is typically found lining the ducts of glands, such as the salivary glands and kidney tubules. These cells are cube-shaped and are involved in absorption and secretion processes.
Option C is incorrect because simple columnar epithelium lines parts of the digestive tract, such as the stomach and intestines. These cells are tall and column-like, with functions including absorption and secretion of mucus. They do not provide the thin, frictionless surface needed for the heart’s endocardium.
Option D is incorrect because stratified squamous epithelium is found in areas subjected to mechanical stress, such as the skin, mouth, oesophagus, and vagina. It consists of multiple layers, providing protection against abrasion. While it is protective, its multi-layered structure makes it unsuitable for the smooth lining required in the endocardium.
Option D is incorrect because pseudostratified columnar epithelium is found lining the respiratory tract, including the nasal cavity and trachea. Although it appears to be stratified, it is actually a single layer of cells of varying heights, often with cilia and goblet cells for mucus secretion.

Question 173:
Answer: E) Sternocostal
Explanation: The sternocostal surface of the heart is the anterior surface that faces the rib cage. It is also known as the anterior or costosternal surface and is formed primarily by the right atrium and right ventricle, with a small portion of the left ventricle. This surface lies directly behind the sternum and ribs, making it the part of the heart that faces the rib cage.
Option A is incorrect because the diaphragmatic surface is the inferior surface of the heart that rests on the diaphragm. It is primarily composed of the left ventricle and a portion of the right ventricle.
Option B is incorrect because the base of the heart is the posterior surface and is formed mainly by the left atrium and part of the right atrium. This surface faces backward toward the spine and is not oriented toward the rib cage.
Option C is incorrect because the apex of the heart is the pointed end of the heart that projects downward, forward, and to the left. It is formed by the tip of the left ventricle. The apex points toward the lower left side of the body, not toward the rib cage.
Option D is incorrect because the right pulmonary surface of the heart faces the right lung. It is primarily formed by the right atrium. This surface is oriented laterally and does not face the rib cage directly.
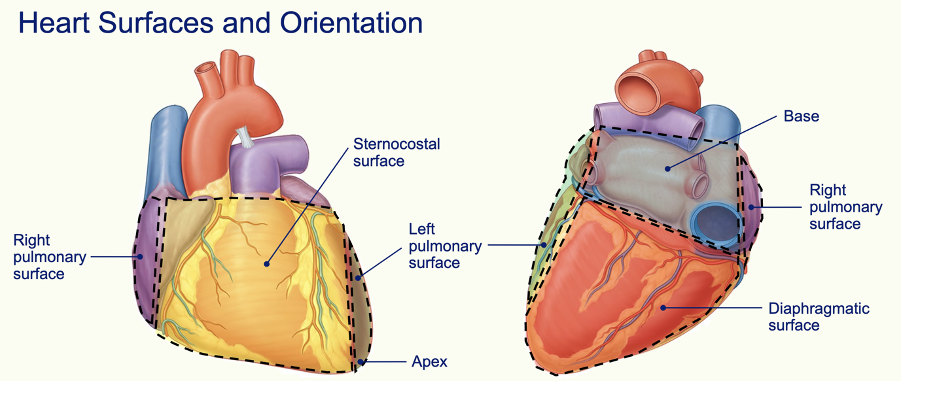
Question 174:
Answer: C) large veins
Explanation: Large veins have the thickest layer of tunica adventitia among blood vessels. This layer is primarily composed of collagen and elastic fibers, providing structural support and protection. In large veins such as the vena cava, the tunica adventitia is particularly well-developed and often contains additional structures like the vasa vasorum, which supplies blood to the outer layers of the vessel wall.
Option A is incorrect because elastic arteries, such as the aorta, have a thick tunica media rich in elastic fibers, allowing them to stretch and recoil with each heartbeat. However, their tunica adventitia is not as thick as that of large veins. The primary role of the elastic arteries is to maintain blood pressure during diastole, not to provide structural support like the tunica adventitia in veins.
Option B is incorrect because muscular arteries, also known as distributing arteries, have a well-defined tunica media composed mainly of smooth muscle fibers. The tunica adventitia in muscular arteries is relatively thinner compared to that in large veins and mainly provides protection and some structural support, rather than being the thickest layer.
Option D is incorrect because medium veins have a more developed tunica adventitia than venules, but it is not as thick as that in large veins. The tunica adventitia in medium veins provides support and prevents overdistension, but the primary focus remains on the large veins for having the thickest tunica adventitia.
Option E is incorrect because venules have a relatively thin wall overall, with a tunica adventitia that is not well-developed compared to larger blood vessels. Their primary function is to collect blood from capillaries and begin the return flow to the heart.
Question 175:
Answer: B) Muscular arteries
Explanation: Muscular arteries have the greatest number of smooth muscle cells in their walls. These arteries are also known as distributing arteries because they distribute blood to various parts of the body. The tunica media of muscular arteries is thick and primarily composed of smooth muscle cells, allowing them to control blood flow by vasoconstriction and vasodilation. This structure is essential for regulating blood pressure and directing blood flow to specific regions according to the body’s needs.
Option A is incorrect because elastic arteries, such as the aorta and its major branches, have a tunica media that is rich in elastic fibers, allowing them to stretch and recoil with the cardiac cycle. Although they do contain smooth muscle cells, their primary function is to maintain blood pressure by absorbing the pulse wave generated by the heart thus these vessels contain the highest number of elastic fibres.
Option C is incorrect because large veins, such as the vena cava, have some smooth muscle cells in their tunica media, but this layer is generally less developed compared to arteries. The tunica adventitia in veins is thicker and more significant than the smooth muscle layer, providing structural support and elasticity rather than actively regulating blood flow through smooth muscle contraction.
Option D is incorrect because medium veins have a relatively thin layer of smooth muscle in the tunica media compared to arteries. Their primary role is to return blood to the heart under low pressure, so they rely more on valves and the skeletal muscle pump than on muscular control. Consequently, the number of smooth muscle cells is considerably less than in muscular arteries.
Option E is incorrect because venules have very few smooth muscle cells, especially in their smaller forms. They primarily serve as conduits for blood returning from the capillary beds to the veins. As they increase in size, some smooth muscle appears in their walls, but it is nowhere near the quantity found in muscular arteries. The focus is on permeability and the exchange of substances rather than regulation of blood flow through muscle contraction.

Question 176:
Answer: D) Gq (G-protein coupled receptor)
Explanation: Angiotensin II binds to the angiotensin II type 1 receptor (AT1R), which is a Gq-coupled receptor. This interaction activates phospholipase C (PLC), leading to the production of inositol triphosphate (IP3) and diacylglycerol (DAG). IP3 then stimulates the release of calcium ions from the endoplasmic reticulum, while DAG activates protein kinase C (PKC). The increase in intracellular calcium and PKC activity leads to several physiological responses, including vasoconstriction, increased blood pressure, and stimulation of aldosterone secretion.
Option A is incorrect because tyrosine kinase receptors are involved in signalling pathways for growth factors such as insulin and epidermal growth factor (EGF). These receptors do not mediate the effects of angiotensin II. Instead, they activate intracellular tyrosine kinases that lead to phosphorylation of specific tyrosine residues, initiating downstream signalling cascades. Instead insulin is what binds to receptor tyrosine kinase not angiotensin II.
Option B is incorrect because nuclear signalling pathways involve steroid hormones, thyroid hormones, and vitamin D, which directly bind to intracellular receptors that function as transcription factors to regulate gene expression. Angiotensin II does not enter the cell to bind to nuclear receptors.
Option C is incorrect because Gs-coupled receptors stimulate adenylyl cyclase, increasing cyclic AMP (cAMP) levels and activating protein kinase A (PKA). This pathway is typical for hormones such as glucagon and adrenaline.
Option E is incorrect because Gi-coupled receptors inhibit adenylyl cyclase, decreasing cAMP levels. This signalling pathway is involved in processes such as the inhibition of neurotransmitter release. While there is some evidence that angiotensin II might have effects mediated by Gi receptors, the primary and most significant pathway for its physiological actions is through Gq-coupled receptors, not Gi.
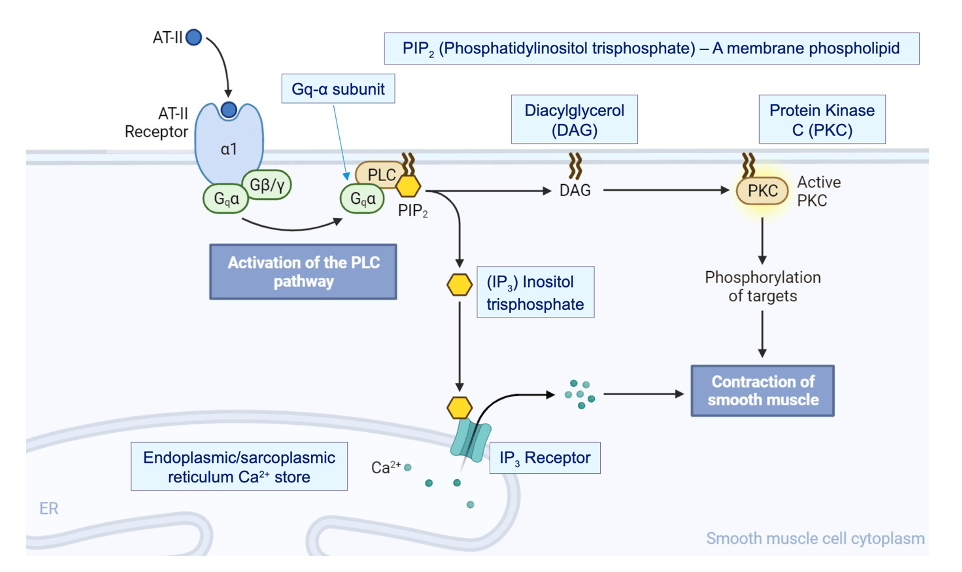
Question 177:
Answer: B) Stage 0 action potential in nodal cells corresponds to rapid depolarisation by L-type calcium channels whereas it corresponds to T-type calcium channels in contractile cells.
Explanation: In nodal cells, Stage 0 of the action potential is characterised by rapid depolarization primarily through L-type calcium channels. In contrast, in contractile cells, Stage 0 corresponds to rapid depolarisation primarily mediated by the influx of sodium ions through voltage-gated sodium channels, not T-type calcium channels.
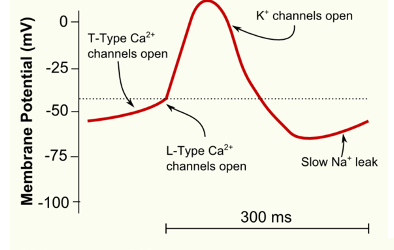
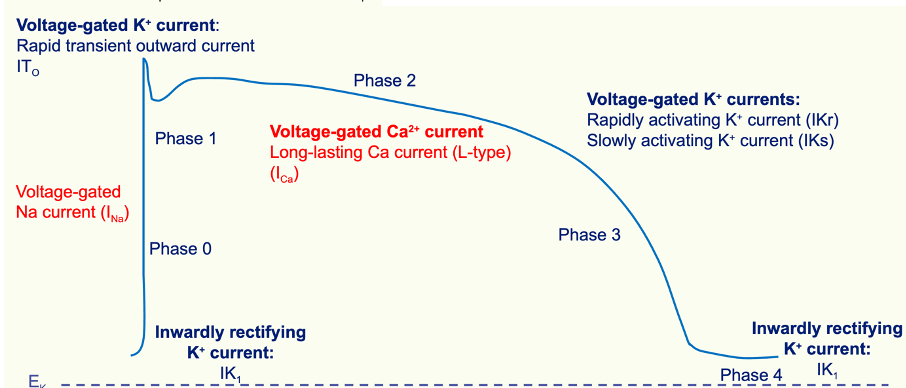
Question 178:
Answer: C) Dromotropy
Explanation: Dromotropy refers to the speed of electrical conduction through the heart, including the Purkinje fibers. It specifically measures how quickly electrical impulses are transmitted through the conduction system of the heart.
Option A is incorrect because ionotropy relates to the force of contraction of the heart muscle.
Option B is incorrect because chronotropy refers to the rate of heart rate or how quickly the heart beats.
Option D is incorrect because louistropy refers to the speed of calcium ion reuptake & relaxation of heart muscles.
Option E is incorrect because hypertrophy refers to the enlargement of an organ, tissue or cell, typically the heart muscle, due to increased workload.
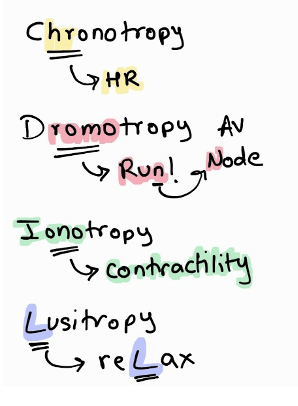
Question 179:
Answer: A) Elastin
Explanation: As we age, elastin, a key component of the tunica media layer of blood vessel walls that provides elasticity and the ability to recoil, is predominantly lost. This loss contributes to the decreased flexibility and increased stiffness of blood vessels in older adults.
Option B is incorrect because collagen levels generally increase with age, contributing to increased stiffness and rigidity of blood vessels.
Option C is incorrect because smooth muscle cells can also change with age, but they are not the predominant component lost.
Option D is incorrect because reticular fibers are less affected by aging compared to elastin.
Option E is incorrect because fibroblasts, which produce extracellular matrix components, are not the primary component lost with aging.
Question 180:
Answer: E) Internal jugular venous pressure
Explanation: The internal jugular venous pressure can be used to indirectly estimate central venous pressure (CVP). The internal jugular vein provides a good reflection of the pressure in the central venous system because it is closely connected to the superior vena cava. Jugular venous pressure (JVP) provides an indirect measure of central venous pressure because the internal jugular vein (IJV) connects to the right atrium without any intervening valves, resulting in a continuous column of blood.
Option A is incorrect because the external jugular venous pressure can provide some insight into CVP but is generally less accurate compared to the internal jugular.
Option B is incorrect because the common carotid venous pressure is not typically used to estimate CVP.
Option C is incorrect because the superior vena cava venous pressure is closely related to CVP but is not measured directly for this purpose.
Option E is incorrect because the subclavian venous pressure is not commonly used for indirect estimation of CVP.
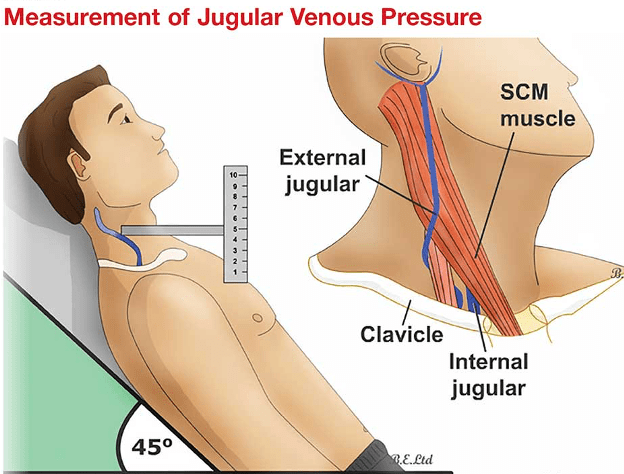
Question 181:
Answer: C) X descent 2
Explanation: X descent 2 on the jugular venous pressure (JVP) waveform corresponds to the phase when the ventricles contract and become physically smaller. This contraction causes a decrease in atrial pressure, allowing blood to be drawn into the atria. This reduction in atrial pressure is reflected as the X descent 2 on the JVP waveform.
Option A is incorrect because X descent 1 reflects the initial drop in atrial pressure due to atrial relaxation. X = relaxation
Option B is incorrect because the C wave corresponds to the bulging of the tricuspid valve into the atrium during ventricular contraction. C = contraction
Option D is incorrect because the V wave is associated with increased atrial pressure against a closed tricuspid valve as the atrium fills with blood during ventricular systole. V = closed valve
Option E is incorrect because the Y descent reflects the phase when the atrium empties into the ventricle after the V wave (due to opening of the tricuspid valve).

Question 182:
Answer: B) Red bone marrow
Explanation: Red blood cells are synthesised primarily in the red bone marrow. This is the primary site of haematopoiesis, where stem cells differentiate into reticulocytes (red blood cells), leukocytes (white blood cells), and megakaryocytes (platelets). The red bone marrow is found in the cavities of certain bones, such as the vertebrae, ribs, and pelvis.
Option A is incorrect because yellow bone marrow is involved in storing fat.
Option C is incorrect because the kidneys produce erythropoietin, a hormone that stimulates red blood cell production in the red bone marrow, but they do not synthesise red blood cells themselves.
Option D & E are incorrect because the liver and spleen are involved in the breakdown and recycling of old red blood cells, but they are not major sites of red blood cell synthesis.
Question 183:
Answer: D) Henry’s law
Explanation: Henry’s law states that when a mixture of gases is in contact with a liquid, each gas will dissolve in the liquid in proportion to its partial pressure. The amount of gas that dissolves in the liquid is also dependent on the solubility of the gas and the temperature of the liquid. This law quantifies how the concentration of a gas in a liquid relates to its partial pressure above the liquid.
Option A is incorrect because Graham’s law relates to the rate of diffusion of gases. The rate of diffusion of gases is inversely proportional to the square root of the molar mass & directly proportional to the concentration of gas. Remember size & concentration of gas.
Option B is incorrect because Fick’s law describes the factors that affect the rate of diffusion such as concentration gradient, surface area, thickness etc. Fick’s = factors
Option C is incorrect because Dalton’s law states that in a mixture of non-reacting gases, the total pressure is the sum of the partial pressures of each individual gas. Dalton = total pressure
Option E is incorrect because Boyle’s law describes the relationship between the pressure and volume of a gas at constant temperature. Boyle = volume
Question 184:
Answer: C) Septum primum
Explanation: The septum primum is the first structure to form. It is a thin, crescent-shaped membrane that grows downward from the roof of the atrium towards the endocardial cushions. As it grows, it divides the common atrial cavity into left and right sections. As the septum primum grows downward, it leaves an initial opening called the foramen primum. This foramen allows blood to flow between the left and right atria while the septum is developing. The foramen primum gradually decreases in size as the septum primum continues to grow. The foramen primum eventually closes as the septum primum fuses with the endocardial cushions, completing the separation of the atria.
Before the foramen primum completely closes, another opening, the foramen secundum, forms in the upper part of the septum primum. This new opening allows continued blood flow between the atria.
The septum secundum grows from the right atrial wall towards the septum primum. It overlaps the foramen secundum, and together with the septum primum, helps form the foramen ovale, which is a crucial fetal shunt allowing blood to bypass the lungs.
The foramen ovale is the opening between the atria that allows blood to flow from the right atrium to the left atrium in the fetus. This shunt is critical for fetal circulation as it allows oxygenated blood from the placenta to bypass the non-functioning fetal lungs. After birth, the foramen ovale typically closes and becomes the fossa ovalis.
The foramen primum is the first structure to form during the separation of the atrium in fetal heart development. It is an opening in the septum primum, which allows blood to flow between the left and right atria while the atrial septum is developing.
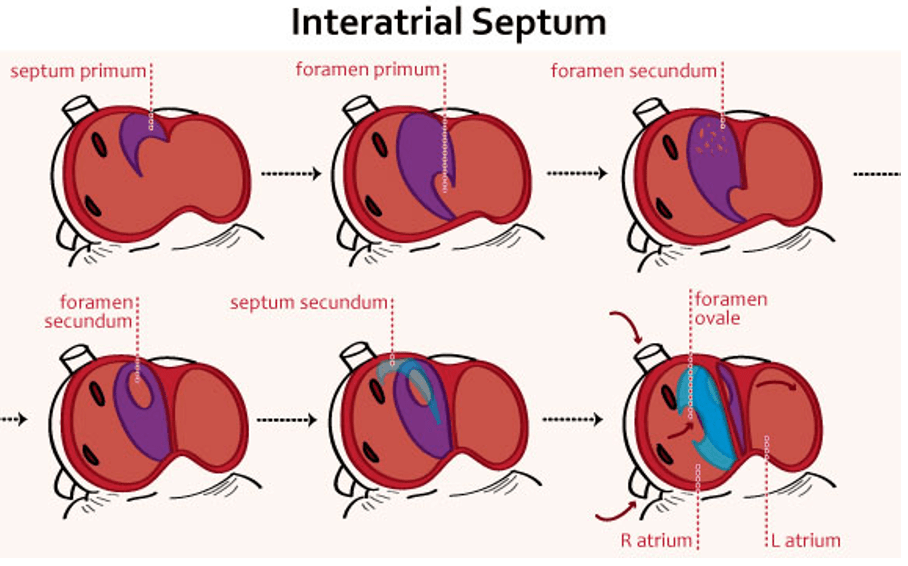
Question 185:
Answer: A) T1-T4
Explanation: If a person experiences a heart attack, the pain is often referred to the dermatomes T1-T4. This is because the heart’s sensory nerves are innervated by sympathetic fibers originating from the spinal segments T1 to T4. When these fibers are activated or irritated due to a heart attack (that detect pain), the pain is commonly perceived in the chest and upper back areas corresponding to these dermatomes.
Option B is incorrect because T1-T5 covers a slightly broader range, but T1-T4 is more specifically associated with the referred pain from a heart attack.
Option C is incorrect because C5-T1 includes cervical dermatomes that are not typically involved in heart attack pain.
Option D is incorrect because C1-C4 covers cervical regions that are not usually associated with cardiac pain.
Option E is incorrect because L1-L5 covers lower back and abdominal regions.
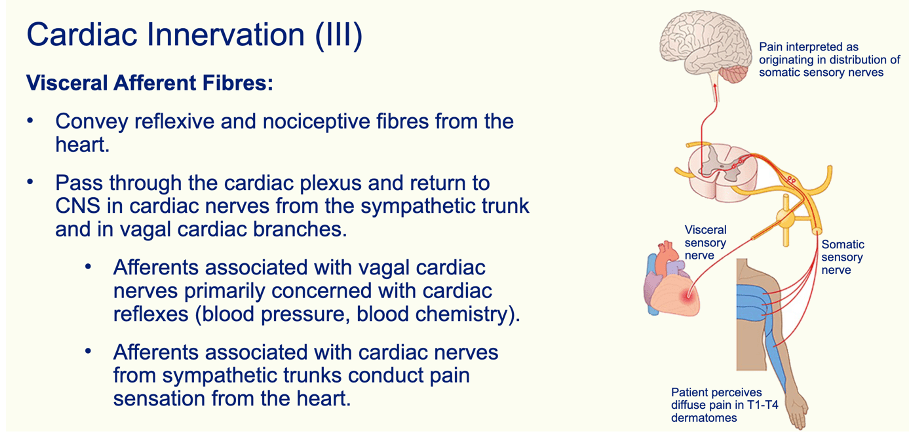
Question 186:
Answer: E) 6
Explanation: The superior vena cava is always found to the right of the aorta.
1 – pulmonary trunk
2 – Left pulmonary artery
3 – Right pulmonary artery
4 – Ascending aorta
5 – Descending aorta
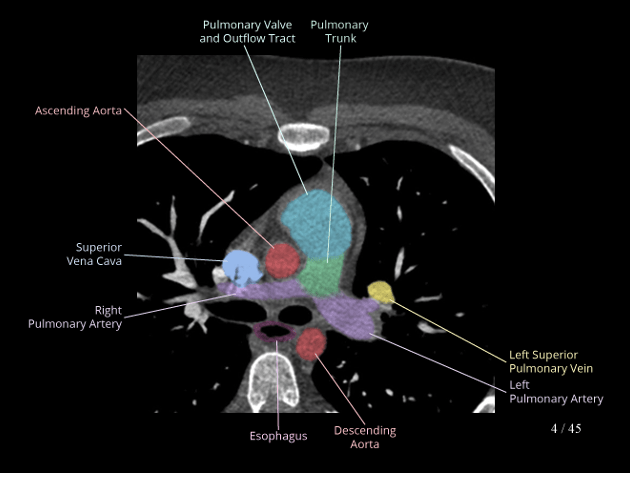
Question 187:
Answer: C) Radial
Explanation: The radial artery can be palpated in the anatomical snuff box. The anatomical snuff box is a triangular depression on the lateral aspect of the wrist, formed by the tendons of the extensor pollicis longus, extensor pollicis brevis & abductor pollicis longus. The radial artery passes through this area, making it possible to feel its pulse here.
Option A is incorrect because the brachial artery is located in the upper arm.
Option B is incorrect because the carotid artery is located in the neck.
Option D is incorrect because the median artery cannot typically be palpated; it is more involved in the blood supply of the hand.
Option E is incorrect because the ulnar artery is located on the medial side of the wrist and is not palpable in the anatomical snuff box but is palpable.
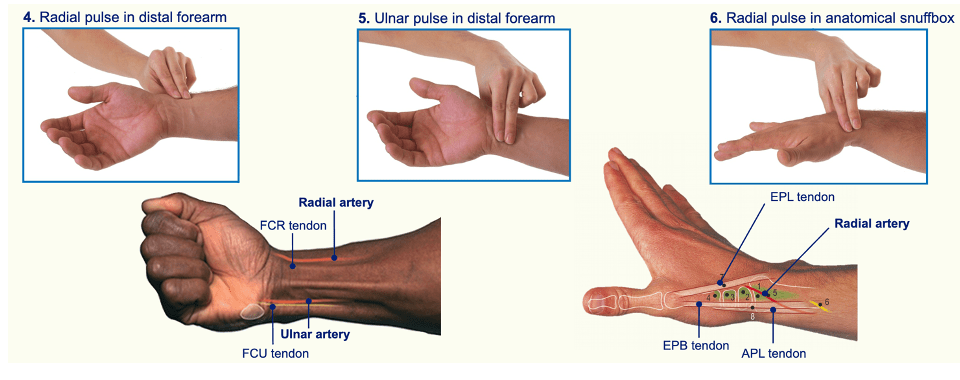
Question 188:
Answer: B) Capillaries
Explanation: Capillaries are the only blood vessels composed of a tunica intima layer only. The tunica intima is the innermost layer of blood vessels and consists of a single layer of simple squamous endothelial cells. In capillaries, this layer is sufficient for their function, which is to facilitate the exchange of gases, nutrients, and waste between the blood and tissues.
Option A is incorrect because arterioles have a tunica intima, tunica media (smooth muscle), and tunica externa.
Option C is incorrect because venules have a tunica intima, tunica media (though it is thin), and tunica externa.
Option D is incorrect because muscular arteries have a well-developed tunica media with smooth muscle cells in addition to the tunica intima and tunica externa.
Option E is incorrect because medium veins also have a tunica intima, tunica media, and tunica externa, with valves often present in their structure.
Question 189:
Answer: A) cAMP (cyclic AMP)
Explanation: Noradrenaline (norepinephrine) utilises cyclic adenosine monophosphate (cAMP) as its second messenger molecule in cardiomyocytes. When noradrenaline binds to beta-1 adrenergic receptors on cardiomyocytes, it activates adenylate cyclase, which then converts ATP to cAMP. The increase in cAMP activates protein kinase A (PKA), which leads to various effects such as increased heart rate and contractility. Noradrenaline can utilise different mechanisms based on the receptor & site of action. E.g., noradrenaline utilises the Gq pathway to trigger contraction of smooth muscle cells in blood vessels using the alpha-1 adrenergic receptor.
Option B is incorrect because adenylate cyclase is the enzyme that converts ATP to cAMP but is not the second messenger itself.
Option C is incorrect because Ca2+ (calcium ions) are involved in the contraction of cardiomyocytes & are second messengers of angiotensin II not noradrenaline.
Option D is incorrect because IP3 (inositol trisphosphate) is involved in signalling pathways that release calcium from the endoplasmic reticulum but is not used by noradrenaline in cardiomyocytes.
Option E is incorrect because Phospholipase C is an enzyme that generates IP3 and diacylglycerol (DAG) involved in the Gq pathway of angiotensin II but is not a second messenger, nor is it used by noradrenaline in cardiomyocytes.

Question 190:
Answer: D) Adipose tissue has a higher fluid content than lean tissue
Explanation: Adipose tissue actually has a lower fluid content compared to lean tissue. Lean tissue, which includes muscle, contains more water, whereas adipose tissue (fat) has a lower water content.
Question 191:
Answer: C) Water
Explanation: Water makes up 96% of the components of lymph. Lymph is a clear or slightly yellowish fluid that is primarily composed of water. It also contains electrolytes, proteins, lipids, and various cellular components, but water makes up the largest proportion of its volume. The other components are present in smaller amounts (4%).
Question 192:
Answer: A) V1-V2
Explanation: In the context of an ECG, the chest leads V1 and V2 are classified as septal leads. These leads are positioned over the anterior part of the chest and are specifically used to view the electrical activity of the heart’s septal wall, which separates the left and right sides of the heart.
Option B is incorrect because V3 and V4 are classified as anterior leads, which view the anterior wall of the left ventricle.
Option C is incorrect because V5 and V6 are classified as lateral leads, which assess the lateral wall of the left ventricle.
Option D is incorrect because lead II, III, and aVF are inferior leads, focusing on the inferior wall of the heart.
Option E is incorrect because lead I, aVR, and aVL are lateral leads, assessing the lateral aspect of the heart.
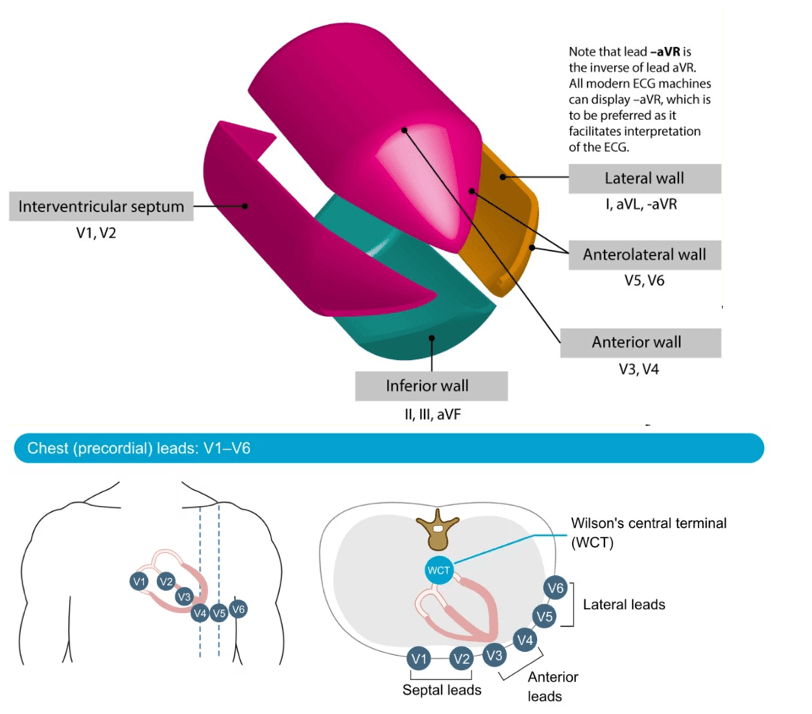
Question 193:
Answer: A) Right coronary artery
Explanation: Leads II, III, and aVF are supplied by the right coronary artery (RCA). In a right-dominant coronary system, the RCA provides blood to the inferior part of the heart, which corresponds to the areas of the heart viewed by these leads.
Option B is incorrect because the left coronary artery (LCA) branches into the left anterior descending artery (LAD) and the left circumflex artery (LCx), supplying the anterior and lateral walls of the heart, respectively.
Option C is incorrect because the posterior descending artery (PDA) supplies the inferior wall of the heart but is a branch of the RCA in a right-dominant system, making it indirectly involved.
Option D is incorrect because the left anterior descending artery (LAD) supplies the anterior wall of the left ventricle.
Option E is incorrect because the left circumflex artery (LCx) supplies the lateral wall of the left ventricle.
RCA: Supplies leads II, III, aVF (inferior leads).
LAD: Supplies leads V1, V2, V3, V4 (anterior leads).
LCx: Supplies leads I, aVL, V5 & V6 (lateral leads).
PDA: Supplies the posterior leads (V7, V8, V9).
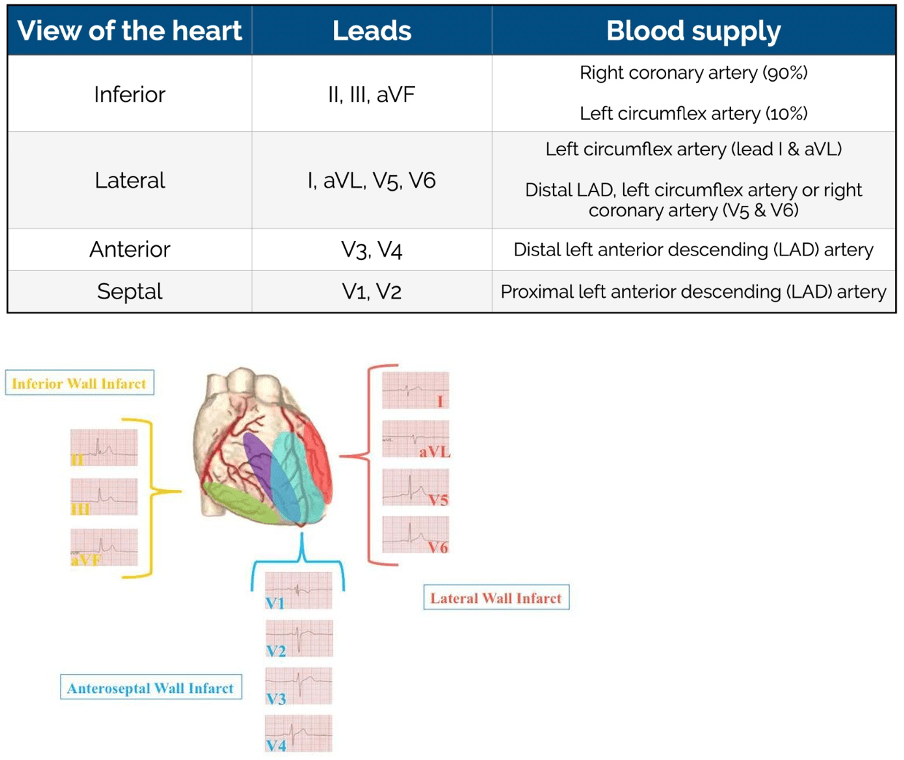
Question 194:
Answer: E) Increased fluid in the venule end of capillaries
Explanation: Reduced oncotic pressure leads to a decrease in the amount of protein, particularly albumin, in the blood plasma. This causes all of the below leading to accumulation of fluid surrounding cells resulting in less reabsorption of fluid at the venule end of capillaries.
Option A is incorrect because reduced albumin synthesis is a cause of decreased oncotic pressure.
Option B is incorrect because decreased oncotic pressure leads to an increase in interstitial fluid, as less fluid is drawn back into the capillaries.
Option C is incorrect because reduced oncotic pressure results in reduced fluid reabsorption from the interstitial space back into the capillaries.
Option D is incorrect because decreased oncotic pressure contributes to oedema due to the accumulation of fluid in the interstitial spaces.
Question 195:
Answer: D) Inflammation leading to the release of cytokines & immune cells
Explanation: Oedema, or swelling due to fluid accumulation in the interstitial space, can be caused by several factors: raised capillary hydrostatic pressure, reduced oncotic pressure, reduced lymphatic drainage & endothelial damage which causes inflammation. Inflammation leads to the release of cytokines and immune cells, which can increase vascular permeability and contribute to fluid leakage into the interstitial space, causing oedema.
Option A is incorrect because reduced capillary hydrostatic pressure and salt/water retention generally do not contribute to oedema. In fact, reduced capillary hydrostatic pressure typically decreases oedema, while salt/water retention usually causes oedema by increasing capillary hydrostatic pressure.
Option B is incorrect because increased oncotic pressure (which means higher protein levels in plasma) typically helps prevent oedema. Low protein levels in plasma (hypoalbuminemia) reduce oncotic pressure and can contribute to oedema.
Option C is incorrect because increased lymphatic drainage helps to reduce oedema by removing excess fluid from the interstitial space. Impaired lymphatic drainage contributes to oedema, not increased drainage.
Option E is incorrect because endothelial repair generally helps restore normal vascular function and reduce oedema.
