
Endocrine (Y2)
Question 1:
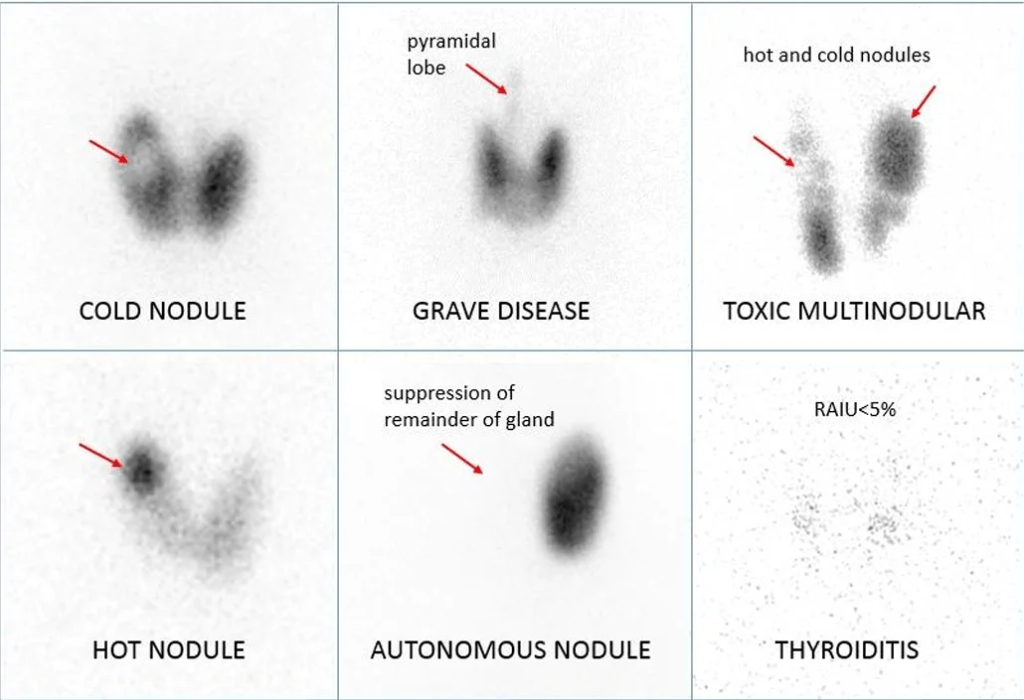
Answer: D) The cold nodule is non-functioning and may warrant FNA to rule out malignancy
Explanation:
Cold nodules appear as areas of decreased or absent uptake on thyroid scintigraphy, indicating non-functioning tissue. These nodules do not take up iodine and may represent malignant lesions, especially when surrounded by functioning (suppressed) thyroid tissue. Therefore, further evaluation with fine needle aspiration (FNA) is recommended to assess for malignancy.
- A) Incorrect: While many cold nodules are benign, they carry a higher risk of malignancy than hot nodules and should not be dismissed without further evaluation.
- B) Incorrect: Functional adenomas appear as “hot” nodules with increased uptake, not cold. A cold nodule, by definition, is non-functioning.
- C) Incorrect: Grave’s disease is characterised by diffusely increased iodine uptake throughout both lobes of the thyroid—not by solitary cold nodules.
- E) Incorrect: Hashimoto’s thyroiditis may show heterogeneous or patchy uptake, but a solitary cold nodule is not diagnostic of Hashimoto’s. Additional serologic and clinical findings are required.

Question 2:
Answer: C) Autoimmune-mediated destruction of pancreatic beta-cells leads to insulin deficiency
Explanation:
This is classic Type 1A Diabetes Mellitus, where an autoimmune process targets the beta-cells of the pancreas, leading to progressive insulin deficiency. The presence of GAD65 antibodies and low C-peptide confirm autoimmune aetiology and loss of endogenous insulin production.
- A) Incorrect: Alpha-cell hyperplasia and glucagon excess may worsen hyperglycaemia, but they are not the primary cause of T1DM.
- B) Incorrect: This describes Type 2 Diabetes, not T1DM. T1DM is not caused by insulin resistance but rather by insulin absence.
- D) Incorrect: Mutations in the insulin receptor are rare and associated with genetic syndromes, not typical T1DM.
- E) Incorrect: Incretin breakdown by DPP-4 affects insulin secretion, but this mechanism is more relevant to Type 2 Diabetes and does not explain the autoimmune destruction central to T1DM.
Question 3:
Answer: C) Exercise-mediated translocation of GLUT4 channels to muscle cell membranes, enhancing glucose uptake
Explanation:
During exercise, skeletal muscle contractions stimulate the insulin-independent translocation of GLUT4glucose transporters to the muscle cell surface, markedly increasing peripheral glucose uptake. In a patient on exogenous insulin, this added uptake can precipitate hypoglycaemia if insulin dosing and carbohydrate intake remain unchanged.
- A) Incorrect: GLUT2 receptors in β-cells detect blood glucose and trigger insulin release under normal physiology, but exercise does not upregulate GLUT2 or increase endogenous insulin secretion in T1DM (where β-cells are destroyed).
- B) Incorrect: Elevated DPP-4 activity would degrade incretins (GLP-1, GIP), reducing insulin secretion and tending to raise blood glucose, not cause hypoglycaemia.
- D) Incorrect: Cortisol is a counter-regulatory hormone that increases hepatic gluconeogenesis and raises blood glucose; it would not provoke hypoglycaemia.
- E) Incorrect: While exercise can improve hepatic insulin sensitivity and reduce hepatic glucose output, this effect is much less pronounced than skeletal muscle glucose uptake via GLUT4 translocation and is not the primary driver of acute exercise-induced hypoglycaemia.
Question 4:
Answer: B) Polymorphisms in HLA genes located on chromosome 6
Explanation:
Type 1A Diabetes Mellitus is strongly associated with HLA gene polymorphisms—especially HLA-DR3 and HLA-DR4—on chromosome 6. These genes encode proteins involved in antigen presentation and contribute to the loss of immune tolerance to pancreatic beta-cell antigens, resulting in autoimmune destruction. The presence of IA-2 and islet cell antibodies supports an autoimmune mechanism.
- A) Incorrect: Mutations in the insulin gene (INS) can cause neonatal diabetes but are not the most common cause of autoimmune T1DM.
- C) Incorrect: GLUT4 is an insulin-responsive glucose transporter found in muscle and adipose tissue, but it is not genetically deleted in T1DM.
- D) Incorrect: Leptin receptor mutations affect weight regulation and are more relevant to obesity-linked Type 2 Diabetes or congenital obesity syndromes.
- E) Incorrect: Glucokinase mutations are associated with MODY2 – maturity onset diabetes of the young, a form of monogenic diabetes (type 2), not autoimmune T1DM.
Question 5:
Answer:
B) Give a sugary drink followed by a carbohydrate snack
Explanation:
This patient is hypoglycaemic (plasma glucose <4.0 mmol/L) and displaying adrenergic symptoms(tachycardia, agitation, sweating), indicating a glucose level between 3.0–3.5 mmol/L, consistent with the measured 2.8 mmol/L. Because he is conscious and able to swallow, immediate treatment is to give rapid-acting glucose (e.g. sugary drink), followed by a slow-release carbohydrate snack to sustain blood glucose levels and prevent recurrence.
- A) Incorrect: IV dextrose is reserved for confused patients who cannot swallow safely or those who are unconscious—not appropriate in this alert patient. It is also administered 10 minutes after a sugary drink is administered if blood glucose remains lower than 4.0 mmol/L.
- C) Incorrect: IM glucagon is used when the patient is confused and unable to swallow—not necessary here.
- D) Incorrect: A high-protein meal is not effective for acute correction of hypoglycaemia and may delay gastric emptying.
- E) Incorrect: Continuous glucose monitoring is useful for long-term prevention, but does not address the urgent need to raise glucose levels in this acute setting.
Question 6:
Answer: D) South Asians are more prone to visceral adiposity and insulin resistance at lower BMI thresholds
Explanation:
South Asians develop insulin resistance and Type 2 Diabetes Mellitus at lower BMI thresholds than Caucasians due to a higher tendency toward central (visceral) adiposity, which contributes more significantly to insulin resistance. This epidemiological observation underpins recommendations for earlier screening and intervention in these populations.
- A) Incorrect: Autoantibody-positive diabetes (e.g. LADA) is not more common in South Asians; LADA is an autoimmune condition and not the primary concern here.
- B) Incorrect: TCF7L2 is a gene associated with beta-cell function and T2DM risk, but it does not specifically increase insulin clearance, nor is its effect exclusive to South Asians.
- C) Incorrect: A reduced incretin response is part of T2DM generally, but it is not exclusive to South Asian individuals.
- E) Incorrect: Pancreatic amyloidosis is more commonly a consequence of long-standing T2DM rather than a racial or ethnic distinction in disease onset, and its absence would not explain early-onset disease.
Question 7:
Answer: B) It influences pancreatic islet cell development and insulin secretion
Explanation:
The TCF7L2 gene, located on chromosome 10, plays a key role in the development and function of pancreatic islet cells, particularly in the regulation of insulin secretion. Variants in this gene are one of the strongest known genetic risk factors for T2DM, independent of obesity, and are believed to impair insulin production.
- A) Incorrect: GLUT4 is an insulin-responsive glucose transporter encoded by a different gene, not TCF7L2, and is primarily involved in peripheral insulin sensitivity, not insulin secretion.
- C) Incorrect: Adipocyte proliferation and visceral fat deposition are influenced by FTO and related genes on chromosome 16, not TCF7L2.
- D) Incorrect: Hepatic gluconeogenesis is regulated by multiple pathways, including insulin receptor substrates, but TCF7L2 does not directly regulate this process.
- E) Incorrect: DPP-4 is responsible for incretin degradation, but TCF7L2 does not enhance this activity—rather, its impact is on pancreatic islet cell biology.
Question 8:
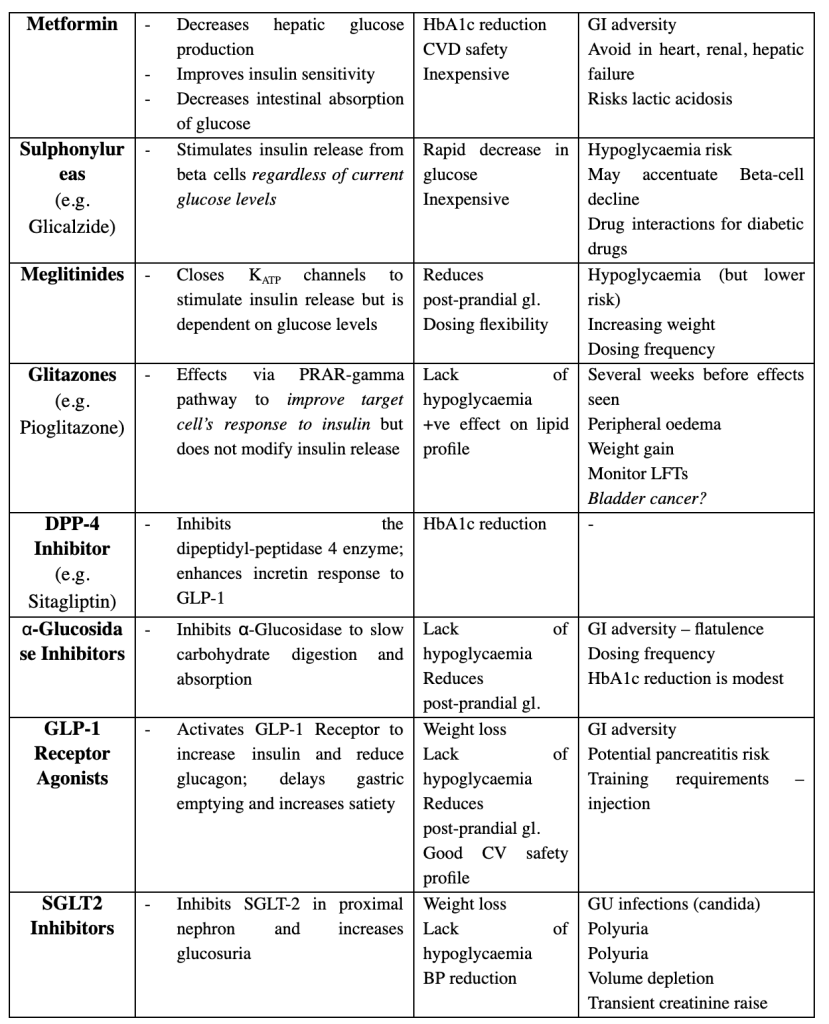
Answer: D) Prescribe a sulfonylurea due to increased sensitivity to these agents
Explanation:
This patient likely has MODY3 – maturity onset diabetes of the young, caused by a mutation in the HNF1-α gene. Unlike Type 1 or Type 2 diabetes, these patients are particularly sensitive to sulfonylureas, which stimulate insulin secretion from functioning beta cells. This is because this mutation affects the functioning of potassium channels in beta cell which sulfonylureas can target. This is the first-line treatment and can often delay or avoid insulin therapy for many years.
- A) Incorrect: MODY patients do not typically require immediate insulin; they usually retain endogenous insulin production, as reflected by a normal C-peptide.
- B) Incorrect: Metformin is useful in insulin resistance seen in T2DM, but not ideal for MODY caused by beta-cell transcription factor defects.
- C) Incorrect: While DPP-4 inhibitors may benefit some with T2DM, they are not first-line in monogenic diabetes such as MODY.
- E) Incorrect: Pancreatic enzyme supplementation is indicated in exocrine pancreatic insufficiency, such as in chronic pancreatitis, not in MODY.
Question 9:
Answer: B) Foetal insulin acts as an anabolic hormone, promoting macrosomia and postnatal rebound hypoglycaemia
Explanation:
In gestational diabetes, maternal hyperglycaemia leads to excessive glucose transfer across the placenta, stimulating foetal pancreatic beta cells to produce high levels of insulin. Foetal insulin is a potent anabolic hormone, causing macrosomia. After birth, the sudden removal of maternal glucose supply, with continued high foetal insulin levels, can lead to neonatal hypoglycaemia.
- A) Incorrect: Foetal insulin is increased, not suppressed, in response to maternal hyperglycaemia.
- C) Incorrect: hCG contributes to maternal insulin resistance, but it does not stimulate foetal beta-cell growth.
- D) Incorrect: Maternal insulin does not cross the placenta; it is the glucose that crosses, stimulating foetal insulin production.
- E) Incorrect: Although metformin can cross the placenta, it does not suppress foetal glucose production in a way that causes these effects.
Question 10:
Answer: D) SGLT2 Inhibitor
Explanation:
SGLT2 inhibitors promote glucosuria, which leads to weight loss, blood pressure reduction, and have demonstrated cardiovascular benefits, making them particularly suitable for patients with established cardiovascular disease. They also do not cause hypoglycaemia and are oral agents, aligning with the patient’s preference to avoid injections.
- A) Incorrect: Sulphonylureas are associated with weight gain and hypoglycaemia, and do not offer cardiovascular benefit.
- B) Incorrect: While glitazones may improve lipid profiles, they are associated with weight gain, fluid retention, and a delayed onset of action—undesirable in heart disease.
- C) Incorrect: DPP-4 inhibitors are weight neutral and safe but do not offer significant cardiovascular benefit compared to SGLT2 inhibitors.
- E) Incorrect: α-Glucosidase inhibitors offer only modest HbA1c reduction, require frequent dosing, and are associated with GI side effects, with no CV benefit.
Question 11:
Answer: B) It bypasses defective signalling upstream by directly activating melanocortin pathways
Explanation:
The patient has a co-dominant heterozygous mutation in a gene involved in the leptin-melanocortin pathway, such as MC4R, which is a common monogenic cause of early-onset obesity. Setmelanotide is a melanocortin-4 receptor agonist, allowing satiety signals to bypass the upstream defect (e.g., leptin or POMC signalling abnormalities) and directly restore hypothalamic appetite suppression.
- A) Incorrect – Leptin sensitivity is not the target; downstream signalling is defective.
- C) Incorrect – Ghrelin suppression is not the main mechanism of Setmelanotide.
- D) Incorrect – Insulin action doesn’t primarily modulate central melanocortin pathways in this context.
- E) Incorrect – GLP-1 signalling is unrelated to the central melanocortin system directly.

Question 12:
Answer: A) Start cabergoline or bromocriptine and monitor visual symptoms
Explanation:
The patient presents with headaches, visual disturbances, and galactorrhoea, which are suggestive of a functioning pituitary adenoma, likely a prolactinoma, despite the absence of an explicitly high prolactin level in the question. The MRI findings of a 3.5 cm pituitary mass (a macroadenoma) compressing theoptic chiasm, along with the galactorrhoea, strongly suggest hyperprolactinemia, which can cause such symptoms. The first-line treatment for prolactinomas is dopamine agonists like cabergoline or bromocriptine, which help lower prolactin levels, shrink the tumour, and alleviate symptoms. Visual symptoms need to be closely monitored as the tumour compresses the optic chiasm, but these medications are effective in most cases.
- B) Incorrect – Surgical resection is typically reserved for cases where medical management (i.e., dopamine agonists) fails, or if there is significant optic nerve compression, but it’s not the first-line therapy unless medication is ineffective or contraindicated.
- C) Incorrect – Octreotide is used to treat GH adenomas (acromegaly), not prolactinomas. This patient’s presentation is more consistent with a prolactinoma.
- D) Incorrect – ACTH therapy would be indicated if the patient had symptoms of Cushing’s disease, which is unlikely given the absence of features such as central obesity, skin changes, or moon facies. The presentation is more suggestive of a prolactinoma.
- E) Incorrect – Radiation therapy is typically used for tumours that are resistant to medical management or for recurrent adenomas, but it is not the first-line treatment for a prolactinoma.
Question 13:
Answer:
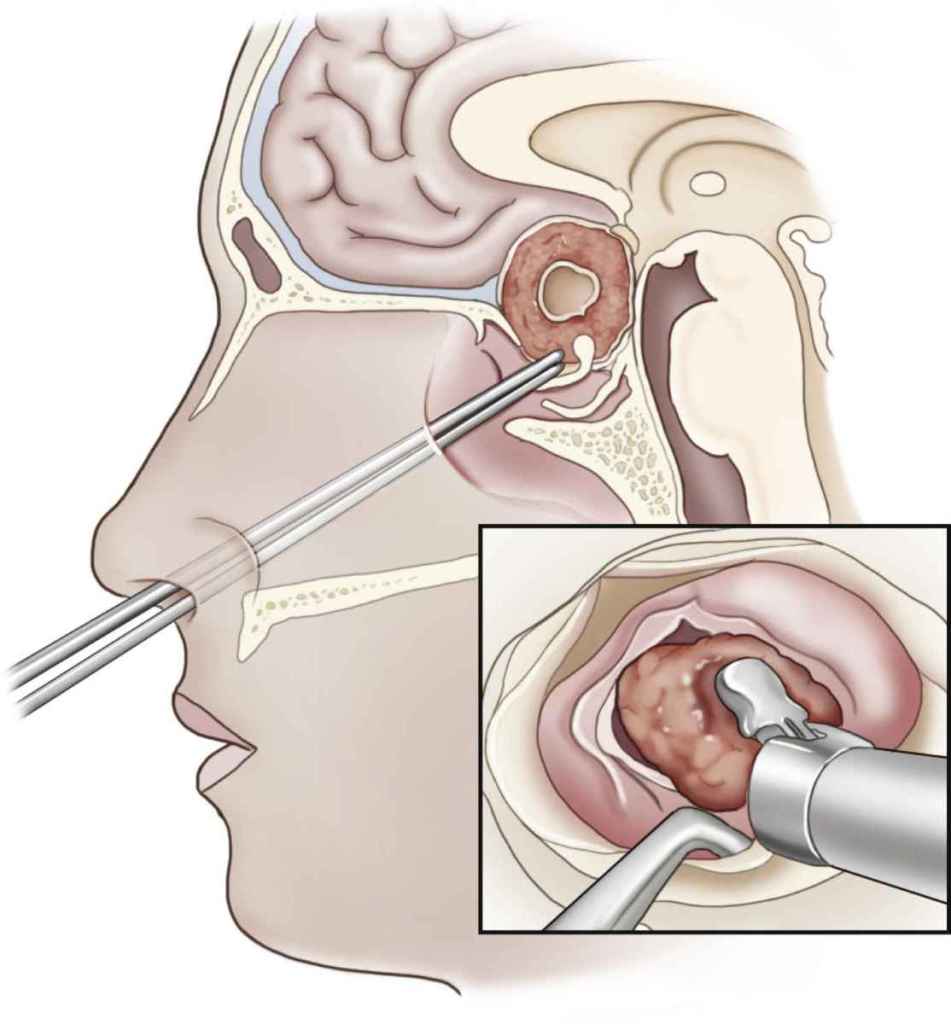
B) Perform a transsphenoidal hypophysectomy
Explanation:
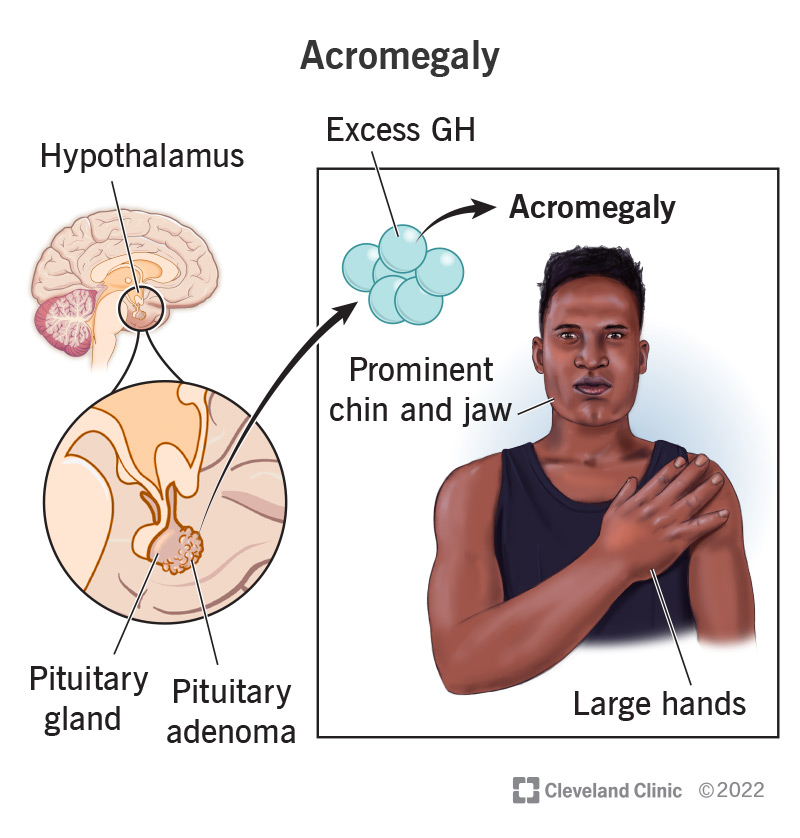
This patient is presenting with classic symptoms of acromegaly, including coarse facial features, macroglossia, spaced-out teeth, and joint pain, along with systemic complications like hypertension and left ventricular hypertrophy, which are common in acromegaly due to excessive growth hormone (GH) secretion. His laboratory findings confirm elevated IGF-1 and GH (1st line), and the oral glucose tolerance test (2nd line) showing unsuppressed GH is diagnostic for GH-secreting adenoma (acromegaly).
The first-line treatment for acromegaly is surgical resection of the pituitary adenoma via transsphenoidal hypophysectomy. This approach is aimed at removing the tumour, which is causing excessive GH production. If surgery is unsuccessful or not possible, radiotherapy or medical therapies such as somatostatin receptor ligands, GH receptor antagonists, and dopamine agonists can be used as adjuncts or alternatives.
- A) Incorrect – Metformin is used for managing diabetes, but this patient’s primary issue is acromegaly, not just diabetes, and should be treated with the primary approach for acromegaly.
- C) Incorrect – Somatostatin receptor ligands (e.g., octreotide) can be used if surgery is not possible or fails, but the next step in this patient should be surgery to address the tumour directly.
- D) Incorrect – Radiotherapy is usually a secondary treatment option when surgery and medical therapies are insufficient, not the first-line approach.
- E) Incorrect – Growth hormone receptor antagonists (e.g., pegvisomant) are used for acromegaly when surgery is not an option or as a second-line treatment, but surgery should be the first step in this patient’s treatment.
Question 14:
Answer: B) Refer for transsphenoidal hypophysectomy
Explanation:
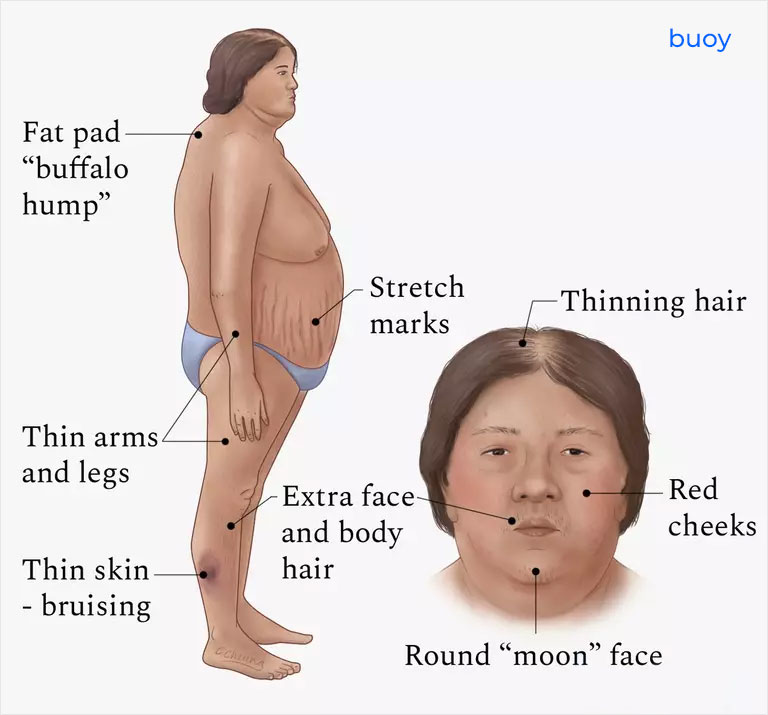
This patient is presenting with clinical features of Cushing’s disease, including central weight gain, moon face, buffalo hump, acne, hirsutism, thin skin, purple striae, hypertension, T2DM, and low bone density. These symptoms, combined with the elevated morning cortisol and failure to suppress cortisol after an overnight dexamethasone test, strongly suggest an ACTH-secreting pituitary adenoma(Cushing’s disease).
Transsphenoidal hypophysectomy is the treatment of choice for Cushing’s disease. It involves the surgical removal of the ACTH-secreting pituitary adenoma, which is typically responsible for the overproduction of cortisol. If surgery is unsuccessful or not feasible, other medical therapies like metyrapone or ketoconazole (which inhibit cortisol production at the adrenal gland level) can be used as adjuncts.
- A) Incorrect – While metyrapone and ketoconazole are used to control cortisol production in cases where surgery is not an option or has failed, the first-line treatment for Cushing’s disease is surgical resection of the pituitary adenoma.
- C) Incorrect – Radiotherapy is generally reserved for patients who have persistent disease following surgery or for those who cannot undergo surgery. It is not the initial treatment for Cushing’s disease.
- D) Incorrect – Glucocorticoid replacement therapy is not appropriate in this patient, as they have excess glucocorticoid production (due to the ACTH-secreting adenoma), not a deficiency. Replacement therapy is used in cases of adrenal insufficiency.
- E) Incorrect – Inferior petrosal sinus sampling (IPSS) is a diagnostic procedure used when there is ambiguity about whether the source of ACTH excess is from the pituitary (Cushing’s disease) or from an ectopic source (e.g., ectopic ACTH production by a tumour). Since the MRI has already identified a pituitary adenoma, IPSS is not necessary at this stage.
Question 15:
Answer: B) Turner’s Syndrome
Explanation:
This child presents with short stature (height < 2nd centile) and a drop in growth centiles, which is suggestive of a growth abnormality. The key finding here is the slightly wider neck, which is a characteristic feature of Turner’s Syndrome.
Turner’s Syndrome is a chromosomal condition (45, X) that results in short stature, and although the girl’s weight is appropriate for her height (which rules out chronic illness), the presence of a wider neck and her normal development point towards this diagnosis.
Common features of Turner’s syndrome include:
- Short stature
- Proportionate weight
- Physical features like a webbed neck, low-set ears, and shield chest (though these may not be immediately apparent in every case)
- Primary ovarian insufficiency leading to infertility or amenorrhea later in life
- A) Incorrect – Growth Hormone Deficiency (GHD) would typically present with abnormal growth velocity and signs such as increased body fat or delayed bone age, none of which are noted here.
- C) Incorrect – Chronic illnesses like Cystic Fibrosis or Asthma would likely be associated with other respiratory symptoms, failure to thrive, or recurrent infections, none of which are described here. She would also likely be underweight but have normal growth velocity & no dysmorphic features.
- D) Incorrect – Idiopathic Short Stature could be a possibility, but the presence of a wider neck raises suspicion for Turner’s Syndrome.
- E) Incorrect – Rickets would typically present with bone deformities and muscle weakness, neither of which are seen in this child.
In this case, Turner’s Syndrome is the most likely diagnosis, and further genetic testing (karyotyping) would confirm this.

Question 16:
Answer: A) Insulin Tolerance Test (ITT)
Explanation:
This child exhibits several clinical features suggestive of Growth Hormone Deficiency (GHD), including short stature, poor growth velocity, prominent forehead, mid-facial hypoplasia, and delayed dentition.
The most appropriate test to confirm GHD is the Insulin Tolerance Test (ITT), which is a stimulation testused to assess GH secretion. In this test, insulin is administered to induce hypoglycaemia, which should stimulate the pituitary gland to release GH. In healthy individuals, GH should rise by about 7 mcg/dL. If the response is insufficient, this indicates GH deficiency.
- B) Incorrect – While an MRI of the pituitary gland is important for detecting structural causes of GHD (such as tumours or anomalies), this test is not used as a diagnostic tool for functional GH deficiency. It is usually performed after confirming the deficiency to assess any anatomical abnormalities.
- C) Incorrect – Karyotyping is not required in this case unless there are suspicions of Turner Syndrome (in girls) or other chromosomal abnormalities. The presence of mid-facial hypoplasia and other features might raise this possibility, but this child is a male, so karyotyping is not the primary diagnostic test here.
- D) Incorrect – Bone age X-ray can be useful to assess delayed skeletal maturation, which can be seen in children with GHD, but it is not sufficient for diagnosis on its own. It is part of the broader evaluation but does not confirm GH deficiency.
- E) Incorrect – While IGF-1 levels are surrogate markers for GH activity and can provide valuable information, stimulation tests such as the Insulin Tolerance Test (ITT) are considered the gold standard for diagnosing GHD. Elevated or low levels of IGF-1 alone are not diagnostic.
Question 17:
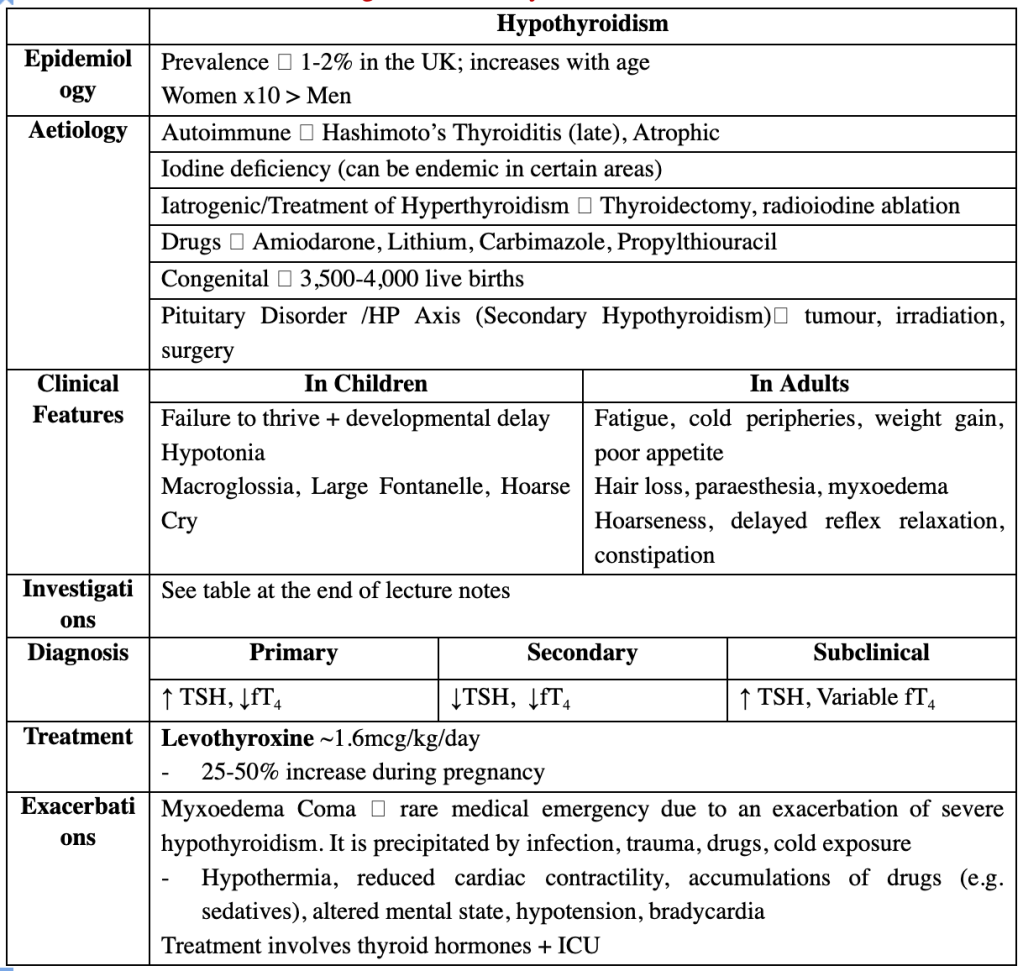
Answer: B) Central hypothyroidism due to lithium-induced pituitary dysfunction
Explanation:
This patient has symptomatic hypothyroidism with low T3/T4 and an inappropriately normal TSH, which strongly suggests secondary (central) hypothyroidism.
- Lithium is a known cause of both thyroid dysfunction (commonly primary) and hypothalamic-pituitary axis disruption, particularly with chronic use, leading to central hypothyroidism.
- In central causes, TSH is low or inappropriately normal despite low T4.
- The absence of anti-TPO antibodies makes autoimmune primary hypothyroidism less likely.
- Hyponatraemia supports hypothyroidism, and her symptoms are consistent with severe underactivity.
Option breakdown:
- A) Subclinical hypothyroidism would have elevated TSH and normal free T4 — this is not the case here.
- C) This is not a myxoedema coma — she is conscious, ambulatory, and not hypothermic or hypotensive.
- D) There’s no lab error suspected; TSH is appropriately measured and not elevated as would be expected in primary disease.
- E) Peripheral T4 to T3 inhibition (e.g. from amiodarone or corticosteroids) would lower T3 but not T4, and is not consistent with the TSH pattern here.
Question 18:
Answer: E) Administer intravenous fluids, beta-blockers, corticosteroids, and potassium iodide
Explanation:
This is a classic case of thyroid storm, a life-threatening exacerbation of hyperthyroidism often triggered by acute illness or surgery (as in this case). The key features pointing to thyroid storm include:
- Hyperpyrexia, tachyarrhythmia (AF), altered mental state, gastrointestinal symptoms, and jaundice
- Suppressed TSH and markedly elevated T4
Management must be immediate and multifactorial:
- IV fluids for support
- Beta-blockers (e.g. propranolol) to control adrenergic symptoms and reduce peripheral T4 to T3 conversion
- Corticosteroids (e.g. hydrocortisone) to reduce hormone release and treat possible adrenal insufficiency
- Potassium iodide to block thyroid hormone release (after antithyroid drug administration)
Option breakdown:
- A) Carbimazole is part of long-term control, but in thyroid storm, urgent multi-drug therapy is needed — not just beta-blocker and carbimazole.
- B) Thyroid uptake scan is contraindicated in unstable patients — do not delay treatment.
- C) Levothyroxine would worsen this case — it is a treatment for hypothyroidism, not thyrotoxicosis.
- D) Thyroidectomy may be a long-term option, but not before stabilisation — this is an emergency requiring medical control first.
Question 19:
Answer: B) Distant metastases are more common in follicular than in papillary carcinoma
Explanation:
- Follicular thyroid carcinoma has a greater tendency to spread haematogenously, most commonly to lungs and bones — explaining the pulmonary nodules in this patient.
- Papillary carcinoma, while more common overall, typically spreads via lymphatics to cervical lymph nodes, with less frequent distant metastasis.
- Medullary carcinoma spreads via lymph and blood but is rare and not the most common cause of pulmonary metastases.
- Vascular invasion is characteristic of follicular carcinoma, distinguishing it histologically from benign follicular adenomas.
Option breakdown:
- A) Incorrect – papillary carcinoma spreads via lymphatics, not follicular.
- B) Correct – follicular carcinoma spreads via blood; distant mets are more frequent.
- C) Incorrect – follicular carcinoma is known for vascular invasion.
- D) Incorrect – haematogenous spread is more typical of follicular, not papillary.
- E) Incorrect – medullary carcinoma can metastasise distantly, but is not the most common.
Question 20:
Answer: C) Anaplastic thyroid carcinoma
Explanation:
This patient presents with rapid growth, compressive symptoms, and vocal cord paralysis, all of which suggest an aggressive thyroid malignancy. The histological findings of highly pleomorphic cells, lack of differentiation, extensive necrosis, and p53 mutation are hallmark features of anaplastic thyroid carcinoma — one of the most aggressive human cancers with very poor prognosis.
Option breakdown:
- A) Papillary carcinoma: Common and indolent, often shows nuclear inclusions, papillary structures, and spreads to lymph nodes — not consistent here.
- B) Follicular carcinoma: Vascular spread and distant metastases (e.g., bone/lung) are more typical. Histology shows follicular architecture.
- C) Correct – Anaplastic carcinoma: Rapid onset, older age, local invasion, necrosis, and undifferentiated cells on biopsy.
- D) Medullary carcinoma: Arises from C-cells, secretes calcitonin (which is negative here), associated with MEN2 syndromes.
- E) Thyroid lymphoma: Also fast-growing, often associated with Hashimoto’s, but FNAC is usually diagnostic, and B-cell markers would be positive.
Question 21:
Answer: C) Adrenal adenoma
Explanation:
This patient has confirmed endogenous Cushing’s Syndrome (based on elevated midnight salivary cortisol and elevated morning cortisol). The key clue here is the low ACTH, which tells us the cortisol excess is ACTH-independent, ruling out:
- B) Pituitary ACTH adenoma → would have normal or high ACTH
- A) Ectopic ACTH (e.g. SCLC) → would also elevate ACTH
- E) ACTH-secreting pheochromocytoma → extremely rare, but ACTH would be high
- D) Pseudo-Cushing’s → typically associated with alcohol use, depression, or severe stress, but ACTH is not typically suppressed, and biochemical abnormalities tend to be less consistent
The most likely cause of ACTH-independent hypercortisolism is an adrenal source — most often a benign adrenal adenoma, which secretes cortisol directly, suppressing ACTH via negative feedback.
Question 22:
Answer: C) Tuberculous adrenalitis; CXR
Explanation:
The patient has primary adrenal insufficiency:
- Hyperpigmentation = elevated ACTH
- Low sodium and low glucose = classic findings
- High ACTH + inadequate response to Synacthen confirms primary (not secondary) adrenal insufficiency
While autoimmune Addison’s is the most common cause in the UK, this patient’s significant weight loss, chronic GI symptoms, and progressive systemic symptoms without other autoimmune features raise strong suspicion for infectious adrenalitis, particularly TB, which remains the most common global cause and should be excluded with a chest X-ray.
Option breakdown:
- A) Secondary adrenal insufficiency; pituitary MRI:
Incorrect — secondary adrenal insufficiency shows low ACTH and normal/increased cortisol with Synacthen. Also, hyperpigmentation would not occur. - B) Autoimmune Addison’s disease; adrenal autoantibodies:
Plausible in the West, but less likely here due to systemic symptoms (e.g. weight loss, GI upset) and infection-related features. CXR is more urgent. - C) Correct – Tuberculous adrenalitis; chest X-ray:
Classic cause of Addison’s disease worldwide, often with insidious onset. TB damages adrenal cortex slowly; X-ray helps confirm the diagnosis. - D) Fungal adrenalitis; serum fungal cultures:
Rare and typically seen in immunocompromised patients (e.g., HIV, transplant recipients). No indication of immunosuppression in this patient. - E) Adrenal infarction; contrast CT of the adrenals:
Typically presents acutely (e.g., in sepsis, antiphospholipid syndrome). This case is chronic with no signs of crisis or bleeding.
Question 23:
Answer: B) Perform adrenal vein sampling
Explanation:
This patient has clinical features consistent with primary hyperaldosteronism (Conn’s syndrome) — young age, resistant hypertension, hypokalaemia, and an elevated aldosterone:renin ratio. Although CT shows an adrenal mass, adrenal vein sampling (AVS) is required to confirm lateralisation and rule out bilateral hyperplasia before proceeding to surgery. CT alone may miss microadenomas or misinterpret non-functioning incidentalomas.
Option breakdown:
- A) Initiate high-dose spironolactone therapy:
Incorrect — This is reserved for bilateral hyperplasia or if the patient is not a surgical candidate. Surgery is preferred in unilateral disease. - B) Correct – Perform adrenal vein sampling:
Essential for differentiating unilateral adenoma (surgical) from bilateral hyperplasia (medical) — especially since non-functioning adenomas are common. - C) Repeat aldosterone:renin ratio off all antihypertensives:
Not needed now — the ARR is already significantly elevated, and CT findings support Conn’s syndrome. We’re now in the localisation stage. - D) Schedule unilateral adrenalectomy:
Premature — AVS is needed first to confirm that the adenoma is responsible for aldosterone excess, as imaging alone is not definitive. - E) Start eplerenone and monitor potassium levels:
Appropriate only in bilateral adrenal disease or where surgery is not feasible.
Question 24:
Answer: C) Initiate alpha-blockade followed by beta-blockade
Explanation:
This patient has a classic presentation of pheochromocytoma (episodic headache, sweating, tachycardia, hypertension), confirmed biochemically by elevated metanephrines and anatomically by adrenal imaging. The cornerstone of safe preoperative management is starting alpha-blockade (e.g. doxazosin) first to prevent hypertensive crises. Beta-blockers should only be added after adequate alpha-blockade to avoid unopposed alpha stimulation, which can precipitate a hypertensive crisis.
Option breakdown:
- A) Immediate surgical resection:
Incorrect — Surgery is curative but must be preceded by medical optimisation (alpha-blockade) to prevent perioperative hypertensive crisis. - B) Beta-blocker therapy:
Incorrect — Starting beta-blockers first is dangerous due to unopposed alpha-adrenergic stimulation, risking a severe hypertensive episode. - C) Correct – Initiate alpha-blockade followed by beta-blockade:
Standard protocol to reduce cardiovascular risk before adrenalectomy. - D) Begin calcium channel blocker therapy only:
Incorrect — CCBs are adjunctive, not first-line; they don’t provide the same protection as alpha-blockers against catecholamine surges. - E) Repeat imaging with MIBG scan for confirmation before any treatment:
Incorrect — Imaging is already conclusive with compatible clinical and biochemical findings. MIBG is reserved for inconclusive cases or suspected metastases.
Question 25:
Answer: A) Hypercalcaemia due to parathyroid hyperplasia
Explanation:
A RET proto-oncogene mutation is associated with Multiple Endocrine Neoplasia type 2 (MEN2)syndromes. These include:
- MEN2A: Medullary thyroid carcinoma, pheochromocytoma, and parathyroid hyperplasia (causing hypercalcaemia).
- MEN2B: Medullary thyroid carcinoma, pheochromocytoma, mucosal neuromas, and marfanoid habitus.
Thus, the most likely associated finding is hypercalcaemia due to parathyroid disease.
Option breakdown:
- A) Correct – Hypercalcaemia due to parathyroid hyperplasia:
Seen in MEN2A, which involves pheochromocytoma and parathyroid overactivity. - B) Increased urinary 5-HIAA:
Incorrect — Suggests carcinoid syndrome, unrelated to pheochromocytoma or RET mutation. - C) Café-au-lait spots and neurofibromas:
Incorrect — These are seen in Neurofibromatosis type 1 (NF1), which can also be associated with pheochromocytomas, but not RET mutations. - D) Flushing and diarrhoea due to serotonin-secreting tumour:
Incorrect — Again points toward carcinoid syndrome, not MEN2. - E) Pancreatic cystadenomas and insulinomas:
Incorrect — These are features of MEN1, not MEN2. MEN1 involves the “3 Ps”: parathyroid, pancreas, pituitary.
Generally, MEN2, NF1 & VHL are all associated with pheochromocytoma.
Question 26:
Answer: C) Asthma
Explanation:
TH2 cells are primarily involved in the immune response against extracellular parasites like helminths, but when dysregulated, they drive allergic responses. They secrete cytokines such as IL-4, IL-5, and IL-13, which are critical in the pathophysiology of asthma, atopic dermatitis, and allergic rhinitis.
Option breakdown:
- A) Type 1 Diabetes Mellitus:
Incorrect — Driven by TH1 cells, which target pancreatic beta cells via a cytotoxic immune response. - B) Multiple Sclerosis:
Incorrect — Also primarily associated with TH1-mediated immune responses against CNS myelin. - C) Correct – Asthma:
TH2 cells promote eosinophilic inflammation, IgE production, and airway hyperresponsiveness, central features of asthma. - D) Rheumatoid Arthritis:
Incorrect — Associated more with TH17 cells, which are pro-inflammatory and play a major role in autoimmune joint destruction. - E) Inflammatory Bowel Disease:
Incorrect — TH17 cells are implicated in chronic inflammation in IBD, particularly Crohn’s disease.
Question 27:
Answer: D) Heterozygosity for HLA-DQβ with aspartate at position 57 (Asp57)
Explanation:
The aspartate (Asp) residue at position 57 of the HLA-DQβ chain plays a critical role in the structure of the MHC class II peptide-binding groove. Its presence stabilises the MHC-peptide complex, allowing for accurate antigen presentation in the thymus, particularly during negative selection of autoreactive T cells.
When Asp57 is absent — as seen in individuals with HLA-DQ2 and HLA-DQ8 — the binding groove is structurally altered, leading to faulty presentation of self-antigens (such as insulin or islet antigens)during thymic education. As a result, autoreactive CD4+ T cells that should have been eliminated may escape into the periphery, ultimately contributing to the development of autoimmunity against pancreatic β-cells.
Thus, individuals who are heterozygous with at least one allele encoding Asp57 are dominantly protected, as the intact peptide-binding groove enables more effective central tolerance.
Option breakdown:
- A) HLA-DR4:
Incorrect — Associated with increased risk of T1DM, not protection. - B) Homozygosity for HLA-DQ8:
Incorrect — Both alleles lack Asp57, impairing thymic deletion of autoreactive T cells. - C) Absence of Asp57:
Incorrect — This is a risk factor, not protective. It disrupts central tolerance. - D) Correct – Heterozygosity with Asp57:
The presence of Asp57 allows for normal peptide-MHC interaction and appropriate deletion of self-reactive T cells during thymic selection, conferring dominant protection. - E) Co-inheritance of HLA-DR3 and HLA-DQ2:
Incorrect — Both alleles are associated with higher susceptibility to T1DM and lack Asp57.
Question 28:
Answer: C) Autoantibodies against adrenal and thyroid tissue associated with HLA-DR3 and HLA-DR4
Explanation:
This patient presents with features of Autoimmune Polyglandular Syndrome Type II (APS-II) — the most common polyglandular autoimmune syndrome. It typically includes Addison’s disease, type 1 diabetes mellitus, and autoimmune thyroid disease (e.g., Hashimoto’s).
APS-II is associated with anti-adrenal and anti-thyroid antibodies and a strong HLA link (HLA-DR3, DR4, DQ2, DQ8). The patient’s symptoms — fatigue, hyperpigmentation, hypotension, hyponatraemia, hyperkalaemia, and low cortisol — are classic for primary adrenal insufficiency (Addison’s). The presence of T1DM and hypothyroidism completes the APS-II triad.
The discordance between monozygotic twins, as in the case of her sister, reflects the role of non-genetic (environmental or epigenetic) factors in disease penetrance, despite shared genetic predisposition.
Option Breakdown:
- A) AIRE gene mutation (APS-1):
Incorrect – This would point toward APS-1, which is much rarer, presents in childhood, and is associated with chronic mucocutaneous candidiasis, hypoparathyroidism, and Addison’s — not seen here. - B) Anti-GAD antibodies:
Incorrect – Anti-GAD antibodies are part of T1DM, but this doesn’t explain the polyglandular presentation or Addisonian features. - C) Correct – Anti-adrenal and anti-thyroid antibodies with HLA-DR3/DR4:
Classic for APS-II, which includes Addison’s, T1DM, and hypothyroidism. This is the best match for the patient’s presentation. - D) Infection-triggered adrenalitis:
Incorrect – There’s no evidence of recent sepsis, meningitis, or TB here. Autoimmune adrenalitis is more likely given the coexisting endocrinopathies. - E) CTLA-4 mutation:
Incorrect – CTLA-4 mutations may cause immune dysregulation syndromes, but these are extremely rare and not the classic mechanism behind APS-II.
Question 29:
Answer: D) Lithium-induced hyperparathyroidism
Explanation:
This patient has hypercalcaemia with elevated PTH and low urinary calcium, along with a history of lithium use. Lithium can alter the set-point of the calcium-sensing receptor (CaSR) in the parathyroid gland, leading to increased PTH secretion despite elevated serum calcium — mimicking primary hyperparathyroidism, but due to medication effect.
Option breakdown:
- A) Primary hyperparathyroidism
Incorrect – While this would show high PTH and high calcium, urinary calcium would typically be normal or elevated. The low urinary calcium suggests a different mechanism. - B) Humoral hypercalcaemia of malignancy
Incorrect – This is a PTH-independent process, with suppressed PTH and often very high calcium. This patient’s PTH is elevated, which rules this out. - C) Familial hypocalciuric hypercalcaemia (FHH)
Incorrect – FHH also shows low urinary calcium and high serum calcium, but it’s genetic and typically diagnosed earlier in life. The presence of lithium therapy in this patient makes lithium-induced more likely. - D) Correct – Lithium-induced hyperparathyroidism
Lithium raises the threshold for calcium sensing by the parathyroid glands, leading to inappropriate PTH secretion in the setting of hypercalcaemia. The low urinary calcium fits the picture. - E) Tertiary hyperparathyroidism
Incorrect – This occurs in chronic renal failure after prolonged secondary hyperparathyroidism. There is no history of CKD or long-standing hypocalcaemia here.
Question 30:
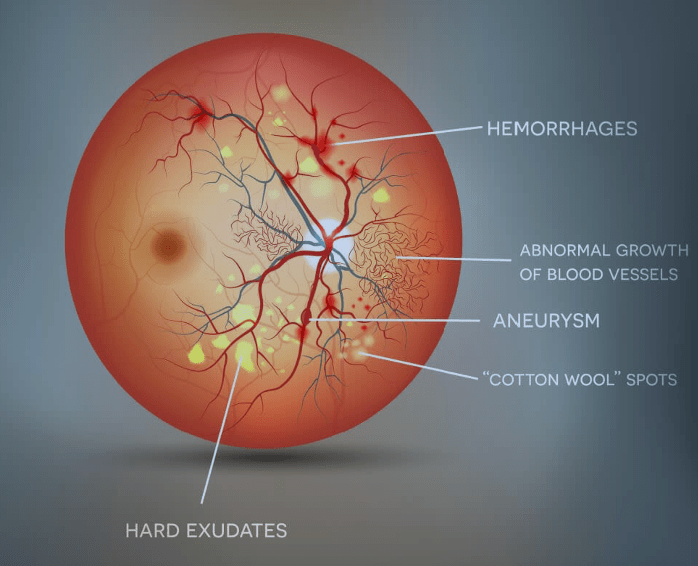
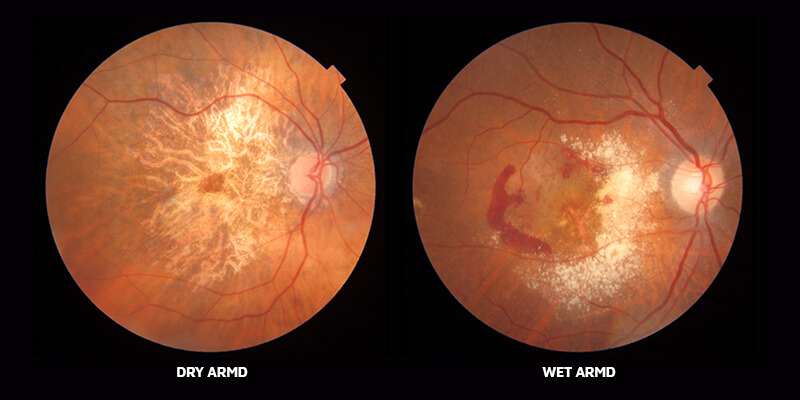
Answer: C) Ischaemic infarcts of the retinal nerve fibre layer
Explanation: Cotton wool spots are small, white, fluffy lesions on the retina that represent localised ischaemia of the retinal nerve fiber layer. This results from occlusion of small retinal arterioles, leading to material buildup in the nerve fibres. In diabetics, these are commonly seen in non-proliferative diabetic retinopathy, but they are non-specific and can also be seen in hypertension.
A) is incorrect, while hypertension can also affect the retina, arteriolar narrowing specifically refers to chronic vasospasm and thickening of arteriolar walls, which leads to signs like “silver-wiring” appearance, and AV nicking—not cotton wool spots.
B) is incorrect as microaneurysms are the earliest visible signs of non-proliferative diabetic retinopathy and are caused by capillary wall weakening due to hyperglycaemia. They appear as tiny red dots, not white cotton wool spots. They can leak fluid or blood, contributing to retinal oedema or haemorrhages, but they are not the same as cotton wool spots.
D) is incorrect because age-related macular degeneration (AMD) affects the macula and leads to central vision loss. It typically presents with drusen (yellow deposits), pigment changes, or neovascularisation in wet AMD. Cotton wool spots are not a feature of AMD and occur in more diffuse retinal diseases rather than macular-specific pathology.
E) is incorrect because vitreous haemorrhage occurs when blood leaks into the vitreous humour, often causing sudden visual loss or “floaters.” It’s commonly caused by trauma, proliferative diabetic retinopathy, or retinal tears. On fundoscopy, you might see obscured retinal structures due to blood—but not cotton wool spots, which are retinal nerve layer infarcts.
Question 31:
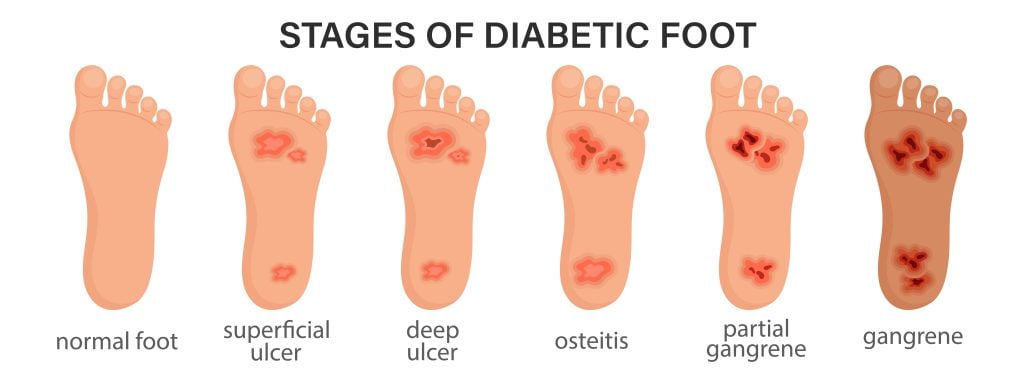
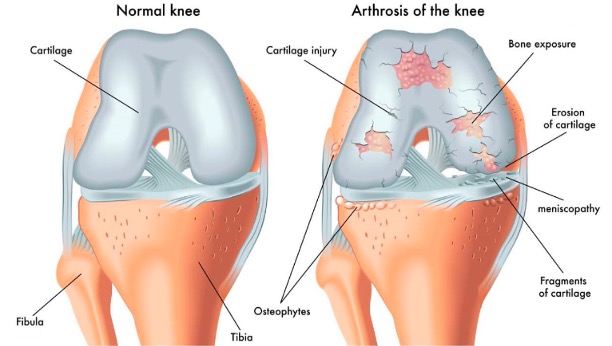
Answer: B) Charcot’s arthropathy
Explanation: Charcot’s arthropathy (Charcot joint) is a progressive, degenerative condition of the bones, joints, and soft tissues, most seen in patients with diabetic peripheral neuropathy. The hallmark findings include painless joint destruction, bone fragmentation, joint dislocation, rocker-bottom deformity, which refers to collapse of the medial longitudinal arch. Loss of protective sensation allows repeated trauma to go unnoticed, eventually leading to severe structural deformities.
A) is incorrect because osteomyelitis (bone infection) is a key differential diagnosis in diabetic foot disease. It often presents with signs of infection (e.g., fever, elevated WBC/CRP, or open ulcers overlying bone). On imaging, you may see bone lysis or periosteal reaction, but not a rocker-bottom deformity or tarsal bone fragmentation in the same way as Charcot’s joint.
C) is incorrect because gout is an inflammatory arthritis caused by uric acid crystal deposition, typically affecting the first metatarsophalangeal joint (great toe). Radiographic features may include “punched-out” erosions with overhanging edges, but not joint dislocation, collapse, or rocker-bottom deformity. Gout is also usually very painful, unlike Charcot joint.
D) is incorrect because osteoarthritis is a degenerative joint disease that commonly affects weight-bearing joints like the knees and hips. In the foot, it may involve the metatarsophalangeal joints. Radiographic features include joint space narrowing and subchondral sclerosis, but not severe joint collapse or bone fragmentation like in Charcot’s arthropathy.
E) is incorrect as although stress fractures are common in diabetics with neuropathy or altered gait, they typically involve a single bone (e.g., metatarsals) and show localised cortical disruption. A stress fracture doesn’t cause the widespread bone destruction, or “rocker-bottom” deformity seen in Charcot’s arthropathy.
Question 32:
Answer: E) Osteoporosis
Explanation: A T-score of -2.5 or lower on a DEXA scan indicates osteoporosis, as defined by the World Health Organization (WHO). The T-score compares the patient’s bone density to that of a healthy 30-year-old adult.
- A T-score of -1.0 to -2.5 = Osteopenia (low bone mass), anything above -1 is normal
- A T-score of -2.5 or lower = Osteoporosis
- If osteoporosis is present with a fragility fracture, it is classified as severe.
Since this patient has a T-score of -3.0 but no fracture is mentioned, the correct classification is osteoporosis.
A) is incorrect because a normal T-score is greater than or equal to -1.0. Since this patient has a T-score of -3.0, her bone density is significantly below normal.
B) is incorrect because osteopenia is defined as a T-score between -1.0 and -2.5. It reflects reduced bone mass, but not enough to meet the threshold for osteoporosis.
C) is incorrect because osteomalacia is a defect in bone mineralisation, often due to vitamin D deficiency, and is not diagnosed by T-score. It’s a different condition from osteoporosis and usually presents with bone pain, muscle weakness, and Looser’s zones (pseudo fractures) on X-ray.
D) is incorrect because severe osteoporosis is diagnosed when the T-score is -2.5 or lower and there is a history of a fragility fracture (e.g., vertebral, hip, or wrist fracture from minimal trauma). Since the case doesn’t mention any fractures, this label does not apply.
Question 33:
Answer: A) Thyroid ultrasound
Explanation: A thyroid ultrasound is the first-line imaging modality for evaluating any palpable thyroid nodule. It is non-invasive, safe, and provides detailed information about the size, composition (solid vs cystic), margins, calcifications, vascularity, and suspicious features that can help guide further management, such as fine-needle aspiration (FNA).
B) is incorrect because a sestamibi scan is used primarily for localizing parathyroid adenomas in the context of primary hyperparathyroidism, not thyroid nodules. It is not used in the routine evaluation of thyroid masses.
C) is incorrect because a CT scan of the neck can be useful for evaluating large goitres, retrosternal extension, airway compression, or suspected malignancy invasion of adjacent structures. However, it is not the first-line investigation for a thyroid nodule and often obscures the thyroid if contrast is used (which can interfere with radioactive iodine uptake later).
D) is incorrect because MRI of the pituitary is done to evaluate pituitary tumours (e.g., prolactinomas, ACTH-secreting tumours). It has no role in the initial evaluation of a thyroid nodule.
E) is incorrect because PET-CT is used in oncologic imaging to detect metastatic disease or unknown primary cancers. It is not first-line for evaluating thyroid nodules and is typically used in thyroid cancer follow-up or in FNA-indeterminate nodules when other results are inconclusive.
Question 34:
Answer: D) FSH
Explanation: 46 XX gonadal dysgenesis is a form of primary ovarian insufficiency where the ovaries are replaced by fibrous streaks and fail to produce normal levels of sex hormones. As a result, there is little or no production of oestradiol or progesterone, leading to loss of negative feedback on the hypothalamic-pituitary axis. This causes elevated FSH and LH levels – a classic feature of hypergonadotropic hypogonadism.
A) is incorrect as oestradiol is decreased or absent in gonadal dysgenesis due to non-functioning ovaries. Low oestradiol is responsible for the absence of secondary sexual characteristics and amenorrhea.
B) is incorrect as progesterone is also low because it is secreted by the corpus luteum after ovulation. In gonadal dysgenesis, ovulation doesn’t occur, so progesterone is not produced.
C) is incorrect because testosterone is typically normal or low in 46 XX individuals. In females, small amounts are produced by the adrenal glands and ovaries. Without functional ovaries, testosterone levels may drop slightly but are not elevated.
E) is incorrect because prolactin is usually normal in gonadal dysgenesis unless there’s an unrelated pituitary disorder. Elevated prolactin is more commonly seen in pituitary adenomas or hypothyroidism, not in ovarian failure.
Question 35:
Answer: B) Papillary carcinoma
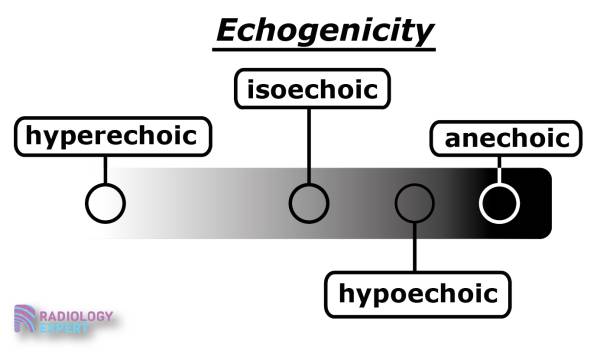
Explanation: Papillary thyroid carcinoma (PTC) is the most common type of thyroid cancer and classically presents on ultrasound as a hypoechoic nodule with microcalcifications, irregular borders, and possibly increased vascularity. Microcalcifications (psammoma bodies) are highly specific for malignancy.
A) is incorrect because colloid nodules are benign and typically appear on ultrasound as spongiform or cystic nodules. They do not show microcalcifications or hypoechoic solid areas.
C) is incorrect because Graves’ disease causes diffuse enlargement of the thyroid with increased vascularity on Doppler ultrasound. It is a form of diffuse autoimmune hyperthyroidism, not associated with solitary nodules or microcalcifications.
D) is incorrect because Hashimoto’s thyroiditis causes a heterogeneous, hypoechoic, and enlarged thyroid gland on ultrasound. While it may increase the risk of lymphoma or carcinoma, it is not characterised by a discrete nodule with microcalcifications.
E) is incorrect because follicular adenomas are benign tumours that often appear as well-circumscribed, isoechoic or hypoechoic nodules. They typically lack microcalcifications and irregular margins. Definitive diagnosis of follicular neoplasm requires histological evidence of capsular or vascular invasion, not ultrasound alone.
Question 36:
Answer: C) FTO
Explanation: The FTO gene (fat mass and obesity-associated gene) is the strongest and most reproducibly associated common genetic variant with obesity and T2DM risk in the general population as it influences appetite regulation and energy homeostasis. Variants in this gene are associated with increased body mass index (BMI), which in turn raises T2DM risk via insulin resistance.
A) is partially incorrect because TCF7L2 (transcription factor 7-like 2) is strongly associated with T2DM, but not with obesity. It affects beta-cell function and insulin secretion. It is one of the most significant diabetes genes in lean individuals with T2DM, not those with obesity-driven insulin resistance.
B) is incorrect because mutations in HNF1α are associated with MODY3 (Maturity-Onset Diabetes of the Young type 3. It is not linked to common obesity or T2DM risk in the general population.
D) is incorrect because SGLT2 is a transporter protein targeted by SGLT2 inhibitors (e.g., dapagliflozin) used in diabetes treatment. Variants in this gene are not a known cause of increased T2DM or obesity risk.
E) is incorrect because GLUT4 is an insulin-responsive glucose transporter in muscle and adipose tissue. While it plays a major role in glucose uptake, genetic variations in GLUT4 are not strongly linked to T2DM or obesity risk in the population.
Question 37:
Answer: E) Impaired fasting glucose (IFG)
Explanation: Impaired fasting glucose is defined by a fasting plasma glucose of 6.1–6.9 mmol/L and/or HbA1c between 42–47 mmol/mol (6.0–6.4%), in the absence of diagnostic criteria for diabetes. This patient has FPG of 6.5 mmol/L and HbA1c of 42 mmol/mol, fitting within the pre-diabetes range. IFG reflects a state of increased risk for diabetes and cardiovascular disease, warranting lifestyle modification and monitoring.
A) is incorrect because normoglycemia is defined as a FPG < 6.1 mmol/L and HbA1c < 42 mmol/mol (6.0%). This patient exceeds both thresholds.
B) is incorrect because gestational diabetes applies only to pregnant women, usually diagnosed between 24–28 weeks gestation. This scenario involves a non-pregnant woman.
C) is incorrect because IGT is diagnosed by a 2-hour plasma glucose of 7.8–11.0 mmol/L during a 75 g oral glucose tolerance test (OGTT). This test wasn’t done in the scenario, and the diagnosis cannot be made from fasting glucose or HbA1c alone.
D) is incorrect because Diabetes is diagnosed by a FPG ≥ 7.0 mmol/L, HbA1c ≥ 48 mmol/mol (6.5%) or a 2-hour OGTT ≥ 11.1 mmol/L. This patient does not meet any of those thresholds.
Question 38:
Answer: A) Sulfonylureas
Explanation: Sulfonylureas (e.g., gliclazide, glimepiride) stimulate insulin release from pancreatic beta cells, regardless of blood glucose levels. This makes them the most likely class to cause hypoglycaemia, particularly in elderly patients, those with irregular meals, or renal impairment. Therefore, they are contraindicated in patients with frequent hypoglycaemia.
B) is incorrect because metformin reduces hepatic gluconeogenesis and improves insulin sensitivity, but it does not stimulate insulin release, so it rarely causes hypoglycaemia, especially when used alone. It is generally safe even in patients with mild hypoglycaemia (but not in renal failure due to lactic acidosis risk).
C) is incorrect because these drugs (e.g., liraglutide, exenatide) enhance glucose-dependent insulin secretion, meaning they only work when glucose is elevated. They have a low risk of hypoglycaemia and are not contraindicated in patients with hypoglycaemia as levels of glucose are low, so they won’t work.
D) is incorrect because DPP-4 inhibitors (e.g., sitagliptin, linagliptin) also act via glucose-dependent mechanisms, making them low-risk for hypoglycaemia. They are generally safe and well tolerated, even in patients with hypoglycaemia.
E) is incorrect because TZDs (e.g., pioglitazone) increase insulin sensitivity but do not increase insulin secretion. Therefore, they rarely cause hypoglycaemia when used alone. Their main concerns include weight gain, fluid retention, and heart failure, but not hypoglycaemia.
Question 39:
Answer: C) C-peptide level
Explanation: C-peptide is released during cleavage of insulin from proinsulin. Very low C-peptide levels indicate an absolute insulin deficiency and are seen in type 1 diabetes due to autoimmune destruction of beta cells. Elevated C-peptide levels may indicate insulin resistance and hyperinsulinemia and are seen in type 2 diabetes due to an increase in insulin at least initially.
A) is incorrect because fasting glucose confirms the presence of diabetes, but it does not distinguish between T1DM and T2DM, as both can cause elevated glucose levels.
B) is incorrect because HbA1c again helps to diagnose and monitor diabetes but cannot differentiate the type.
D) is incorrect because Ketones may be present in T1DM due to insulin deficiency but can also be elevated in stress, fasting, or diabetic keto acidosis-like presentations of T2DM (especially in youth), it can also be absent in both, so it is unreliable.
E) is incorrect because T2DM is often associated with dyslipidaemia, but lipid profile abnormalities are nonspecific and cannot differentiate between T1DM and T2DM.
Question 40:
Answer: D) Growth Hormone (GH)
Explanation: These symptoms all describe acromegaly which is caused by excess growth hormone (GH), usually from a pituitary adenoma, after epiphyseal plate closure. Features include frontal bossing, enlarged jaw (prognathism), macroglossia, increased hand/foot size, organomegaly, and insulin resistance. GH stimulates IGF-1, which mediates most of the tissue overgrowth.
A) is incorrect because excess cortisol causes Cushing’s syndrome, which includes central obesity, moon face, buffalo hump, purple striae, and muscle wasting, but not frontal bossing or acromegalic features.
B) is incorrect because prolactin excess causes galactorrhoea and hypogonadism (amenorrhea in women, low libido in men). It is often co-secreted with GH in pituitary adenomas, but prolactin itself does not cause acromegaly.
C) is incorrect because aldosterone excess (e.g. Conn’s syndrome) leads to hypertension, hypokalaemia, and metabolic alkalosis, but no tissue overgrowth or facial changes.
E) is incorrect because excess thyroxine (hyperthyroidism) leads to weight loss, tremor, heat intolerance, and palpitations, but does not cause tissue enlargement as seen in acromegaly.

Question 41:
Answer: B) Suppressed plasma renin and elevated aldosterone
Explanation: Primary hyperaldosteronism (Conn’s syndrome) is caused by autonomous aldosterone production (often from an adrenal adenoma or hyperplasia). Aldosterone increases sodium and water retention, raising blood pressure, and promotes potassium excretion, causing hypokalaemia. The elevated blood pressure suppresses renin via negative feedback. Thus, the classic diagnostic pattern is high aldosterone, low renin and a high aldosterone-to-renin ratio (ARR). If the ratio is above 4 it suggests the adenoma is unilateral and if it is less than 3 it suggests that its bilateral.
A) is incorrect because this suggests secondary hyperaldosteronism (e.g., in renovascular hypertension, heart failure, or diuretic use), not primary. Renin is high due to reduced renal perfusion, which secondarily raises aldosterone.
C) is incorrect as this is seen in the use of ACE inhibitors but is not consistent with primary hyperaldosteronism.
D) is incorrect because Conn’s syndrome causes hypokalaemia due to excess potassium excretion by the kidneys. Elevated potassium would be the opposite of what’s expected.
E) is incorrect because cortisol is used to diagnose Cushing’s syndrome, not primary aldosteronism.
Question 42:
Answer: D) Von Hippel-Lindau (VHL)
Explanation: VHL is an autosomal dominant condition caused by mutations in the VHL tumour suppressor gene. It is most associated with bilateral pheochromocytomas, as well as hemangioblastomas (brain, retina), renal cell carcinoma, pancreatic cysts or tumours. Pheochromocytomas in VHL are often bilateral and extra-adrenal.
A) is incorrect because MEN1 (Multiple Endocrine Neoplasia type 1) includes parathyroid adenomas, pituitary tumours and pancreatic neuroendocrine tumours, butt is not associated with pheochromocytomas.
B) is incorrect, while pheochromocytomas do occur, they are often unilateral and less commonly bilateral than in VHL.
C) is incorrect because as although pheochromocytomas can occur, they are typically unilateral and less common than in VHL or MEN2.
E) is incorrect because is not associated with tuberous sclerosis
Question 43:
Answer: B) Pioglitazone
Explanation: Pioglitazone is a thiazolidinedione (TZD), a class of drugs that works by improving insulin sensitivity. Thiazolidinediones are associated with fluid retention, which can worsen heart failure and may lead to oedema or even exacerbate congestive heart failure (CHF). Due to this effect, TZDs like pioglitazone are contraindicated in patients with heart failure, especially those with fluid retention.
A) is incorrect because metformin is an oral antihyperglycemic agent that works by reducing hepatic glucose production and improving insulin sensitivity. Metformin is not associated with fluid retention and is generally safe in patients with heart failure, though it should be used cautiously in severe renal impairment.
C) is incorrect because empagliflozin is an SGLT2 inhibitor that works by blocking glucose reabsorption in the kidneys, leading to glucosuria and diuresis. SGLT2 inhibitors have been shown to have a protective effect on heart failure by reducing fluid overload, improving cardiovascular outcomes, and lowering hospitalization rates for heart failure. Therefore, empagliflozin is not contraindicated and may even be beneficial in heart failure.
D) is incorrect because liraglutide is a GLP-1 receptor agonist that helps regulate blood glucose by increasing insulin secretion and suppressing glucagon release. It has neutral effects on fluid retention and is not contraindicated in heart failure. In fact, some GLP-1 agonists have cardioprotective effects.
E) is incorrect because While insulin itself does not directly cause fluid retention, it can lead to weight gain and fluid retention indirectly, especially when used in excess. However, it is not typically contraindicated in heart failure based solely on fluid retention concerns, as its impact on fluid balance is less pronounced compared to drugs like thiazolidinediones.
Question 44:
Answer: C) Medullary carcinoma
Explanation: Medullary thyroid carcinoma (MTC) is the most likely diagnosis in a patient with a solitary thyroid nodule and elevated serum calcitonin. Calcitonin is a hormone produced by parafollicular C-cells in the thyroid, and it is significantly elevated in MTC which can occur sporadically or as part of MEN2A or MEN2B, where patients may also have other manifestations like pheochromocytomas and hyperparathyroidism.
A) is incorrect because papillary thyroid carcinoma (PTC) is the most common form of thyroid cancer, but it is not associated with elevated calcitonin. PTC typically presents with a solitary thyroid nodule, and it is more likely to cause lymph node metastases and may have Psammoma bodies on histology.
B) is incorrect because follicular thyroid carcinoma (FTC) arises from the follicular cells of the thyroid and is not associated with elevated calcitonin. FTC typically presents as a solitary nodule on ultrasound or physical exam, and it is more prone to hematogenous metastasis, often to the lungs and bones.
D) is incorrect because anaplastic thyroid carcinoma is a rare and aggressive form of thyroid cancer that typically occurs in older patients. It is often not associated with elevated calcitonin and presents with a rapidly enlarging thyroid mass, neck pain, and difficulty breathing due to compression of surrounding structures.
E) is incorrect because thyroid lymphoma typically presents as a rapidly growing, painless thyroid mass, often in patients with Hashimoto’s thyroiditis. Lymphomas in the thyroid do not secrete calcitonin and are a very different entity from medullary carcinoma in terms of origin, clinical course, and prognosis.
Question 45:
Answer: E) Non-functioning thyroid tissue
Explanation: A cold nodule on a radioisotope scan (typically using iodine-123 or technetium-99m) indicates a non-functioning or hypofunctioning thyroid nodule. Cold nodules do not take up the radioisotope as much as the surrounding normal thyroid tissue, suggesting that the nodule is not producing thyroid hormones. These nodules can be benign or malignant, but further diagnostic tests (e.g., fine-needle aspiration) are often required to distinguish between these possibilities.
A) is incorrect because hyperfunctioning thyroid tissue would appear as a hot nodule on a radioisotope scan, meaning it takes up more of the radioactive iodine or technetium than surrounding tissue. Hot nodules are typically benign and are often associated with thyroid adenomas or toxic nodular goitre, which secrete excess thyroid hormones.
B) is incorrect because iodine deficiency can cause an enlarged thyroid gland (goitre), but it does not specifically lead to the formation of cold nodules on a radioisotope scan. The thyroid gland might show reduced iodine uptake overall in the setting of iodine deficiency, but this is different from the specific appearance of cold nodules, which suggests non-functioning thyroid tissue.
C) is incorrect because Graves’ disease is an autoimmune condition characterised by diffuse hyperthyroidism and increased uptake of radioactive iodine in the entire thyroid gland (not just a nodule). It typically results in “diffusely hot” thyroid tissue, not cold nodules, and is associated with elevated T3 and T4 levels.
D) is incorrect because thyroiditis, particularly Hashimoto’s thyroiditis, may cause hypothyroidism but does not typically lead to cold nodules on a radioisotope scan. Thyroiditis may present with a diffusely reduced uptake or no uptake in the thyroid, but the clinical presentation and lab findings (e.g., elevated thyroid antibodies) are more indicative of the condition than the radioisotope scan.
Question 46:
Answer: B) Intraductal papilloma
Explanation: Intraductal papilloma is the most common cause of bloody nipple discharge, particularly in premenopausal women. It is a benign tumour that arises in the lactiferous ducts, usually located beneath the areola. The lesion is often not palpable, but discharge may be spontaneous and unilateral. Histologically, it’s characterized by fibrovascular cores lined by both luminal epithelial and myoepithelial cells.
A) is incorrect because fibrocystic changes is a common benign breast condition in women of reproductive age. It presents with lumpy breasts and cyclic pain and not typically bloody.
C) is incorrect because sclerosing adenosis is a benign proliferative lesion of the lobules with fibrosis and glandular crowding, it may mimic carcinoma on imaging, but it is not associated with nipple discharge, especially not bloody discharge.
D) is incorrect because duct ectasia involves dilation and inflammation of subareolar ducts, typically in older women. It may cause thick, greenish or cheesy nipple discharge, nipple retraction, and pain but not typically bloody.
E) is incorrect because phyllodes tumour is a rare fibroepithelial tumour, that may be benign or malignant. It typically presents as a rapidly enlarging, painless breast mass but it is not commonly associated with nipple discharge.
Question 47:
Answer: A) ACTH
Explanation: Addison’s disease is primary adrenal insufficiency, meaning the adrenal cortex itself fails, leading to low cortisol and aldosterone, high ACTH (due to loss of feedback) and features of fatigue, weight loss, hypotension, hyperpigmentation, hyponatremia, hyperkalaemia. In secondary adrenal insufficiency, the problem lies in ACTH deficiency, usually from pituitary dysfunction. This also leads to low cortisol, mimicking Addison’s symptoms except Aldosterone is preserved (regulated by renin-angiotensin system, not ACTH) and there is no hyperpigmentation (ACTH is low).
B) is incorrect because GH deficiency leads to growth retardation in children and reduced muscle mass, fatigue and a poor quality of life in adults. It is not associated with Addisonian symptoms.
C) is incorrect because TSH deficiency causes secondary hypothyroidism: fatigue, cold intolerance, weight gain, bradycardia—but not adrenal insufficiency features.
D) is incorrect because gonadotropin deficiency causes hypogonadism which includes amenorrhea, infertility, decreased libido, reduced secondary sex characteristics but does not mimic Addison’s disease.
E) is incorrect because prolactin deficiency is rare and generally presents with failure of lactation postpartum. It has no link with Addisonian features.
Question 48:
Answer: C) Humoral hypercalcaemia of malignancy
Explanation: Humoral hypercalcaemia of malignancy is a paraneoplastic syndrome characterised by highly elevated serum concentrations of calcium. Many solid tumours (especially squamous cell carcinomas, renal, and breast cancers) secrete PTHrP, which mimics the action of PTH so stimulates bone resorption and increases renal tubular reabsorption of calcium but is not subject to negative feedback This causes PTH to be suppressed due to the hypercalcemia.
A) is incorrect because primary hyperparathyroidism is caused by autonomous PTH secretion (e.g., parathyroid adenoma) so the problem is within the parathyroid gland itself. Bloods show high calcium, high or inappropriately normal PTH whilst PTHrP is normal. So PTH would not be suppressed, and PTHrP wouldn’t be elevated.
B) is incorrect because tertiary hyperparathyroidism is seen in chronic kidney disease after long-standing secondary hyperparathyroidism. This causes the parathyroid gland to become autonomously hyperactive. Bloods will show high calcium, very high PTH and normal PTHrP. Again, PTH would be elevated, not suppressed.
D) is incorrect because Familial hypocalciuric hypercalcemia (FHH) is a genetic condition caused by inactivating mutations in the calcium-sensing receptor. It causes mild asymptomatic hypercalcemia, high-normal PTH, and low urinary calcium excretion. PTH is not suppressed, and PTHrP is not involved.
E) is incorrect because sarcoidosis produces 1,25-dihydroxyvitamin D (calcitriol) which leads to increased intestinal calcium absorption. Therefore, bloods will show high calcium, low or normal PTH, normal PTHrP but high calcitriol. Hypercalcemia here is vitamin D–mediated, not PTHrP-mediated
Question 49:
Answer: D) Prolactin
Explanation: The most common functioning pituitary adenoma is a prolactinoma. A macroadenoma (>10 mm) can compress the optic chiasm, leading to bitemporal hemianopia. It can also cause headache and hypogonadism. It is very common in older women, especially with visual symptoms.
A) is incorrect because Growth hormone (GH) causes acromegaly in adults. GH-secreting adenomas are less common than prolactinomas but can also grow large and compress the optic chiasm. However, prolactinomas are far more common and likely in this scenario unless there are acromegaly-specific features (e.g. enlarged jaw, hands).
B) is incorrect because adrenocorticotropic hormone (ACTH) cause Cushing’s disease when secreted in excess by a pituitary adenoma. ACTH-secreting adenomas tend to be microadenomas and are less likely to grow large enough to compress the optic chiasm.
C) is incorrect because TSH-secreting adenomas are extremely rare. They may present with hyperthyroidism, but not typically with compressive symptoms unless the tumour is unusually large.
E) is incorrect because ADH is secreted by the posterior pituitary or hypothalamus, not by adenomas of the anterior pituitary. It is not associated with macroadenomas or visual field defects. It can cause SIADH or diabetes insipidus, but not compressive symptoms.
Question 50:
Answer: E) Increased urinary metanephrines
Explanation: Pheochromocytomas are catecholamine-secreting tumours (usually of the adrenal medulla). They release epinephrine, norepinephrine, and dopamine, leading to episodic or sustained hypertension, headaches, palpitations, and sweating. The most sensitive test is 24-hour urinary metanephrines or plasma free metanephrines, which detect breakdown products of catecholamines.
A) is incorrect because elevated serum cortisol suggests Cushing’s syndrome, not pheochromocytoma. Cushing’s may also cause hypertension, but the hallmark symptoms (e.g. central obesity, striae, proximal muscle weakness) are not present here.
B) is incorrect because hypoglycaemia is not typical of pheochromocytoma. If anything, pheochromocytomas can cause hyperglycaemia due to catecholamine-induced inhibition of insulin.
C) is incorrect because low plasma renin activity can occur in primary hyperaldosteronism (Conn’s syndrome), another cause of hypertension but is not characteristic of pheochromocytoma. Conn’s syndrome also causes hypokalaemia, which is not mentioned here.
D) is incorrect because although hypercalcaemia is seen in hyperparathyroidism, or as part of MEN 2A, which can include pheochromocytoma, calcium levels are not diagnostic of pheochromocytoma itself.
Question 51:
Answer: B) Osteolytic bone metastases
Explanation: Breast cancer often metastasises to bone, where tumour cells activate osteoclasts, leading to bone resorption and hypercalcemia. This results in high calcium and suppressed PTH. This is a common cause of hypercalcemia in cancer and fits the patient’s context well.
A) is incorrect because ectopic PTH secretion is very rare, they usually secrete PTHrP, not intact PTH and PTH would be elevated, not suppressed, in true PTH ectopic secretion. Breast cancer does not commonly do this.
C) is incorrect because primary hyperparathyroidism is a benign or malignant parathyroid tumour that causes excess PTH secretion. We would expect to find high calcium and high/inappropriately normal PTH which is not consistent with suppressed PTH.
D) is incorrect because vitamin D intoxication causes increased calcium absorption from the gut. This would show high 25(OH)D or 1,25(OH)₂D levels and is less common than bone metastases in cancer patients.
E) is incorrect because FHH is a genetic disorder that is characterised by decreased urinary calcium excretion and (usually asymptomatic) hypercalcemia. PTH levels are normal in most patients, and it is caused by an autosomal dominant mutation of a calcium-sensing receptor in the kidneys and parathyroid gland.
Question 52:
Answer: A) Autoimmune Polyglandular Syndrome Type 1 (APS-1)
Explanation: APS-1 (also called APECED: Autoimmune Poly Endocrinopathy-Candidiasis-Ectodermal Dystrophy) is a rare monogenic autoimmune syndrome caused by mutations in the AIRE gene. The AIRE gene (Autoimmune Regulator) is essential for central tolerance, it promotes expression of self-antigens in the thymus so that autoreactive T cells can be deleted. Defects in AIRE allow autoreactive T cells to escape, leading to multiple autoimmune diseases. It includes chronic mucocutaneous candidiasis, hypoparathyroidism and adrenal insufficiency (Addison’s disease).
B) is incorrect because grave’s is an autoimmune hyperthyroid condition caused by stimulatory TSH receptor autoantibodies, but it is polygenic, not typically associated with AIRE mutations.
C) is incorrect because Hashimoto’s thyroiditis is an autoimmune hypothyroid condition caused by anti-thyroid peroxidase (TPO) and anti-thyroglobulin antibodies. It is also polygenic and not linked to AIRE mutations.
D) is incorrect because SLE is a multisystem autoimmune disorder with complex polygenic and environmental factors. It involves autoantibodies (like anti-dsDNA), but not AIRE mutations.
E) is incorrect because Myasthenia gravis is caused by autoantibodies against acetylcholine receptors, leading to muscle weakness. It’s associated with thymic abnormalities but not with AIRE gene defects.
Question 53:
Answer: C) HLA-DR5
Explanation: Hashimoto’s thyroiditis is a chronic autoimmune thyroid disease characterised by anti-thyroid peroxidase (TPO) and anti-thyroglobulin antibodies. It often leads to hypothyroidism. The strongest HLA association is with HLA-DR5. Hashimoto’s involves cell-mediated cytotoxicity and autoantibodies leading to gradual thyroid destruction.
A) is incorrect because HLA-DR3 is associated with Graves’ disease and Type 1 diabetes, but not the primary risk allele for Hashimoto’s.
B) is incorrect because HLA-DR4 is linked more to rheumatoid arthritis and Type 1 diabetes (often with DQ8), not Hashimoto’s.
D) is incorrect because HLA-DQ2 is primarily associated with celiac disease, not Hashimoto’s.
E) is incorrect because HLA-DQ8 is strongly associated with Type 1 diabetes, especially when combined with DR4.
Question 54:
Answer: A) Asp57
Explanation: The presence of aspartic acid (Asp) at position 57 of the HLA-DQβ chain is protective against Type 1 diabetes mellitus (T1DM). This residue alters peptide presentation to T cells in a way that reduces autoreactivity, thereby lowering the risk of T1DM. Loss of Asp57 (e.g., substitution by Ser, Ala, or Val) is associated with increased risk for T1DM due to a more diabetogenic peptide-binding profile.
Question 55:
Answer: C) Activates GLP-1 receptors
Explanation: Semaglutide is a GLP-1 receptor agonist. It mimics the action of glucagon-like peptide-1, an incretin hormone that enhances glucose-dependent insulin secretion, suppresses glucagon secretion, delays gastric emptying and promotes satiety and weight loss. These effects collectively help in lowering blood glucose levels and aiding weight control in patients with type 2 diabetes.
A) is incorrect because this describes the mechanism of orlistat, used for weight loss, not diabetes.
B and D) are incorrect because they are not relevant here.
E) is incorrect because drugs like spironolactone do this and are useful in conditions like heart failure or hyperaldosteronism, not diabetes.
Question 56:
Answer: A) FTO
Explanation: The FTO (fat mass and obesity-associated) gene is the most well-established genetic factor associated with polygenic obesity. Individuals with high polygenic risk scores involving FTO variants are more likely to develop higher body mass index (BMI), increased fat mass, severe, early-onset, and persistent obesity trajectories. This is because FTO influences appetite regulation, energy homeostasis, and possibly food reward behaviours.
B) is incorrect because BRCA1 is associated with hereditary breast and ovarian cancer, not obesity.
C) is incorrect because APOE is linked to Alzheimer’s disease and lipid metabolism, not specifically obesity.
D) is incorrect because CFTR is mutated in cystic fibrosis, which is often associated with underweight, not obesity.
E) is incorrect because EGFR is related to epithelial growth and cancer, particularly lung and colorectal, not body weight regulation.
