
Gastroenterology (Y2)
Question 1:
Answer: A) Symptoms must be present for at least 3 months, with onset 6 months prior, and include infrequent bowel movements (<3 per week).
Explanation: The Rome IV criteria is used to diagnose functional gastrointestinal disorders, including functional constipation. It includes fewer than 3 spontaneous bowel movements per week, this must occur for at least 3 months, with an onset at least 6 months prior. Symptoms can include straining during defecation, lumpy or hard stools (Bristol Stool Scale types 1–2), the use of manual manoeuvres to facilitate defecation.
B is incorrect because alternating constipation and diarrhoea is more typical of IBS.
C is incorrect because blood in the stool and weight loss suggests colorectal cancer.
D is incorrect as abdominal pain which is relieved by defecation is characteristic of IBS.
E is incorrect because nausea and vomiting are not primary features of functional constipation.

Question 2:
Answer: B) They form a physical barrier to prevent reflux.
Explanation: Alginates are medications (like Gaviscon) that contain polysaccharide polymers derived from brown seaweed and are used to manage reflux symptoms. They react with gastric acid to form a viscous gel that floats on top of the stomach contents, preventing acid from refluxing into the oesophagus.
A) is incorrect because neutralization is the function of antacids, not alginates.
C) is incorrect because alginates do not influence acid secretion, that is the action of proton pump inhibitors (PPIs).
D) is incorrect as alginates do not influence motility either, this is the function of prokinetics.
E) is incorrect because H2 blockers block histamine receptors, not alginates.
Question 3:
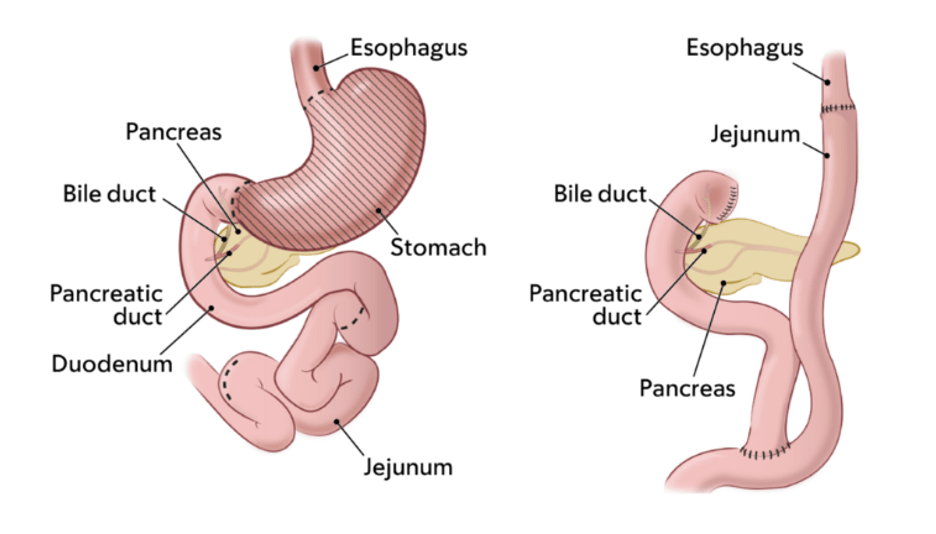
Answer: E) Partial gastrectomy with gastrojejunostomy.
Explanation: Billroth II is a surgical procedure where the stomach is partially removed, and the remaining portion is connected to the jejunum, bypassing the duodenum. Indications include peptic ulcer disease and gastric cancer. However, complications do occur that include Dumping syndrome and nutritional deficiencies (iron, calcium, B12).
A) is incorrect because a partial gastrectomy with anastomosis to the duodenum describes Billroth I.
B) is incorrect because a total gastrectomy with oesophagojejunostomy is used for total gastric removal, not partial.
C) is incorrect because subtotal gastrectomy with ileal bypass is not a standard surgical procedure.
D) is incorrect as this is an example of an ileocecal resection which is unrelated.

Question 4:
Answer: B) Dumping syndrome
Explanation: Dumping syndrome occurs after gastric surgery such as Roux-en-Y and Billroth II. It involves gastric emptying which leads to hyperosmolar chyme entering the small intestine very rapidly. This rapid movement of food into the small intestine causes a shift of fluid into the gut to dilute the food, leading to symptoms like diarrhoea, bloating, and dizziness due to fluid imbalance. Late symptoms (1–3 hours) and include hypoglycaemia from insulin surge. Management involves dietary changes (small, frequent meals and low carbohydrate).
A) is incorrect as postprandial hypoglycaemia occurs when blood sugar drops after eating and does not typically cause diarrhoea but may lead to dizziness, sweating, and shakiness.
C) is incorrect as gastroparesis is delayed stomach emptying, often due to diabetes or nerve damage. Symptoms include nausea, vomiting, and bloating, but not diarrhoea or sweating.
D) is incorrect as reactive hypoglycaemia occurs when blood sugar drops a few hours after eating (not within 30 minutes). Symptoms include sweating, shakiness, and confusion but not diarrhoea.
E) is incorrect because bile acid malabsorption occurs when bile acids are not reabsorbed in the ileum (e.g., after ileal resection). It causes chronic watery diarrhoea, but not dizziness or sweating.
Question 5:
Answer: C) Anastomotic leak
Explanation: Roux-en-Y gastric bypass (RYGB) is a surgical procedure for morbid obesity. The stomach is divided into a small pouch (~30 mL), which is connected directly to the jejunum, bypassing the rest of the stomach and duodenum. The purpose of it is to reduce food intake and absorption. However, complications do occur and involve Dumping syndrome, nutritional deficiencies, and anastomotic leaks. An anastomotic leak is a breakdown at the surgical connection (anastomosis) between the stomach pouch and jejunum causing chyme to leak out into the peritoneum. It is serious because it can lead to peritonitis (inflammation of the peritoneum), sepsis, and multi-organ failure.
A) is incorrect as Dumping syndrome occurs after eating.
B) is incorrect as small bowel obstruction (SBO) is a blockage in the small intestine, often due to adhesions or hernias, symptoms include crampy abdominal pain, vomiting, and distension. Usually there is no fever or tachycardia unless complicated by ischaemia or perforation.
D) is incorrect as a wound infection is an infection at the surgical incision site, with symptoms including localised redness, swelling, and pus. There is no generalised peritonitis.
E) is incorrect because postoperative ileus is the temporary paralysis of intestinal motility. Symptoms include abdominal distension, absent bowel sounds, and delayed flatus (fart). However, there is no fever or signs of systemic inflammation.
Question 6:
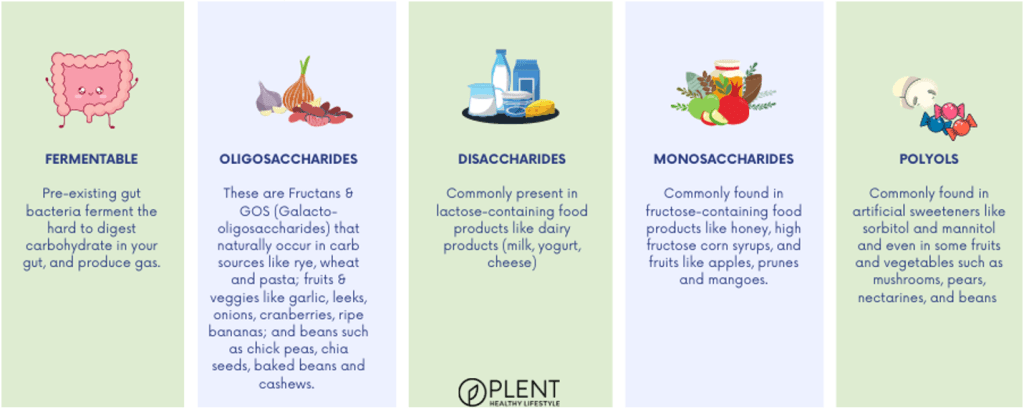
Answer: D) Foods containing fermentable oligosaccharides, disaccharides, monosaccharides, and polyols
Explanation: FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These are short-chain carbohydrates and sugar alcohols that are poorly absorbed in the small intestine. When FODMAPs reach the colon undigested, gut bacteria ferment them, producing gas. This leads to bloating, abdominal pain, and flatulence (farting). In addition, FODMAPs draw water into the intestine, causing diarrhoea in sensitive individuals. Irritable Bowel Syndrome (IBS) is the most common condition where FODMAP restriction helps.
Examples of FODMAPs:
- Oligosaccharides: Found in wheat, onions, garlic, and legumes.
- Disaccharides: Lactose (in milk and dairy products).
- Monosaccharides: Fructose (in honey, apples, and high-fructose corn syrup).
- Polyols: Sorbitol and mannitol (in stone fruits, sugar-free gum, and candies).
A) is incorrect as although high-fat foods can slow gastric emptying and worsen symptoms in conditions like gastroparesis but are not the focus of the FODMAP diet.
B) is incorrect as protein is not a significant contributor to fermentation or osmotic effects in the gut.
C) is not the best answer as gluten is a protein found in wheat, barley, and rye. It is avoided in coeliac disease, but not specifically in the FODMAP diet (though gluten-containing foods may also be high in FODMAPs).
E) is not the best answer either because lactose is a disaccharide and part of the FODMAP group, but the FODMAP diet restricts a broader range of fermentable carbohydrates beyond just lactose.
Question 7:
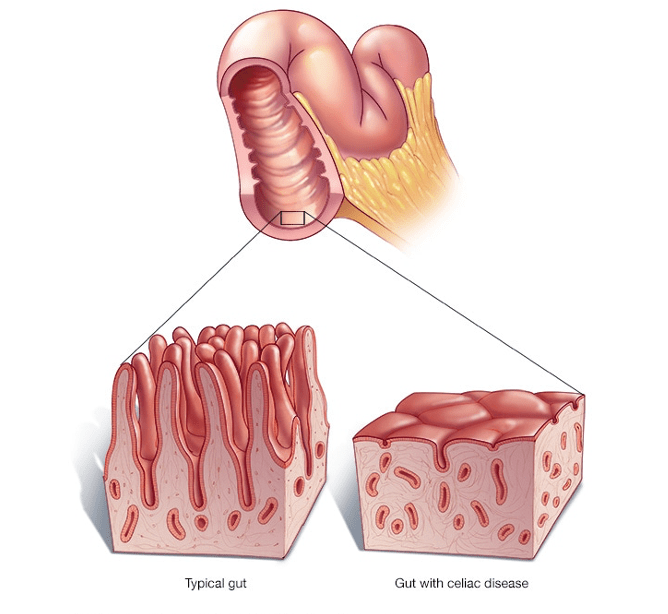
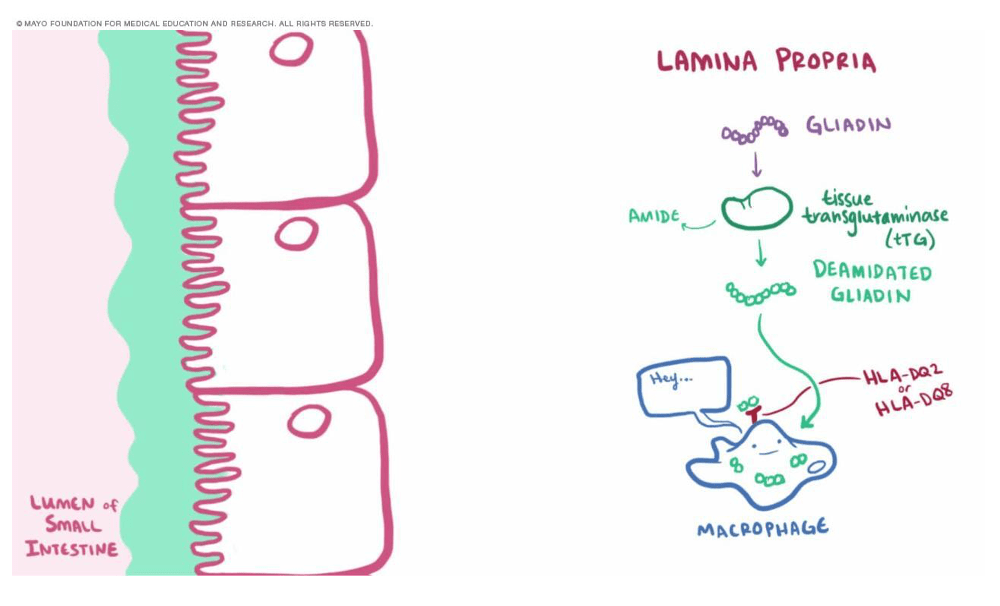
Answer: C) Coeliac Disease
Explanation: Coeliac disease is an autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. In genetically predisposed individuals (with HLA-DQ2 or HLA-DQ8 alleles), gluten ingestion leads to an immune-mediated attack on the small intestinal mucosa. Chronic inflammation leads to villous atrophy, crypt hyperplasia, and lymphocytic infiltration in the small intestine. Symptoms of coeliac disease include: diarrhoea, steatorrhea, abdominal pain, bloating. Nutritional deficiencies can also occur and include: iron-deficiency anaemia (most common). Vitamin D deficiency causing rickets in children and osteomalacia in adults. Symptoms with extraintestinal manifestations may occur in some people but not all too including: dermatitis herpetiformis (pruritic rash), fatigue, weight loss and infertility.
A) is incorrect because although Irritable Bowel Syndrome (IBS) can cause diarrhoea and abdominal pain, it does not lead to malabsorption, anaemia, or elevated anti-tTG antibodies.
B) is incorrect as although Crohn’s Disease may cause anaemia, anti-tTG antibodies are not elevated.
D) is incorrect because lactose intolerance leads to bloating, diarrhoea, and flatulence but does not cause systemic symptoms like weight loss, anaemia, or fatigue.
E) is incorrect because ulcerative colitis does not lead to an increase in IgA tTG levels or any systemic effects such as anaemia.
Question 8:
Answer: D) Microscopic Colitis
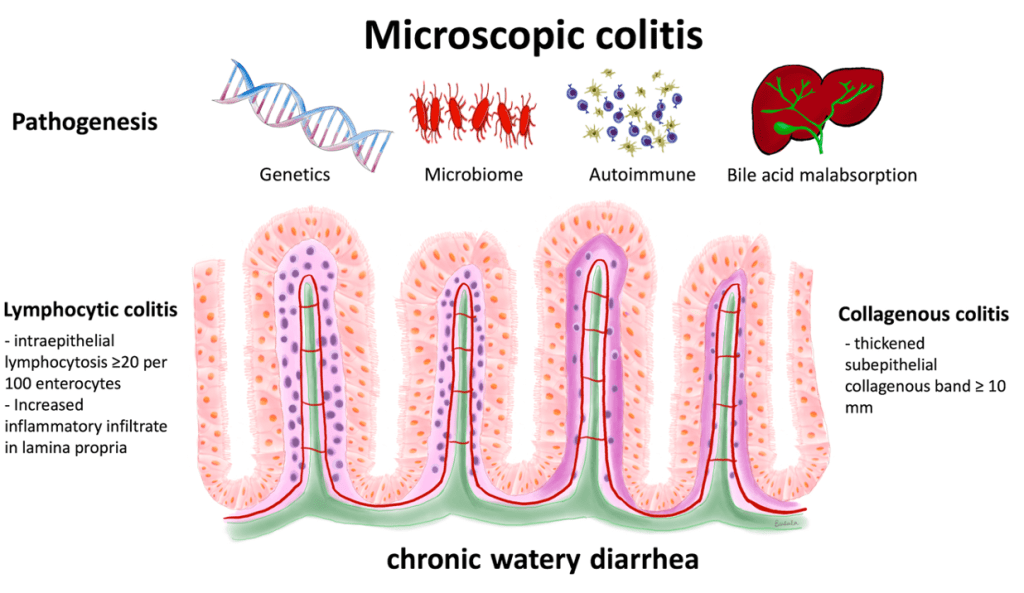
Explanation: Microscopic colitis is an inflammatory condition of the colon that causes chronic watery diarrhoea without visible abnormalities on colonoscopy. It is like Irritable bowel diseases such as Crohn’s and ulcerative colitis but does involves a smaller portion of the colon in comparison to them and there are no systemic symptoms such as weight loss, fever, or anaemia and a normal colonoscopy, distinguishing it from IBD. It is divided into two subtypes:
Collagenous colitis: Characterised by a thickened subepithelial collagen band.
Lymphocytic colitis: Characterised by increased intraepithelial lymphocytes.
A) is incorrect because Crohn’s Disease typically causes transmural inflammation anywhere in the GI tract so may involve the small intestine. It presents with abdominal pain, weight loss, and systemic symptoms, and colonoscopy often shows visible mucosal changes.
B) is incorrect because Irritable Bowel Syndrome (IBS) does not cause histological changes. It is a functional disorder characterised by abdominal pain that is relieved by defecation and altered bowel habits.
C) is incorrect because ulcerative Colitis causes bloody diarrhoea, abdominal pain, and visible mucosal inflammation on colonoscopy.
E) is incorrect because Coeliac Disease causes malabsorption, weight loss, and villous atrophy on small bowel biopsy, not colonic changes.
Question 9:
Answer: A) Peptic Ulcer Disease (PUD)
Explanation: H. pylori is a gram-negative bacterium that colonises the stomach and is a major cause of gastritis, peptic ulcers, and gastric cancer. It is transmitted via the faecal-oral route and often colonises the gastric antrum. It produces urease, which neutralises stomach acid, allowing it to survive in the acidic environment. H-pylori also induces gastritis by disrupting the mucosal barrier and triggering an inflammatory response and increase gastrin secretion, leading to increased acid production, which can result in the formation of peptic ulcers. Symptoms include epigastric pain that is relieved by food or antacids, nausea and bloating and black stools which is suggestive of upper gastrointestinal bleeding due to ulceration.
B) is incorrect because Gastro Oesophageal Reflux Disease (GORD) presents with heartburn and regurgitation, not with epigastric pain and black stools.
C) is incorrect because Helicobacter pylori Infection is the causative factor for PUD, but the question specifically asked for the most likely diagnosis, which is PUD.
D) is incorrect because although gastric Cancer can be caused by H. pylori infection, it typically presents with more advanced symptoms such as weight loss and early satiety.
E) is incorrect because Coeliac Disease presents with malabsorption, diarrhoea, and weight loss, not the symptoms described here.
Question 10:
Answer: B) Gastroschisis
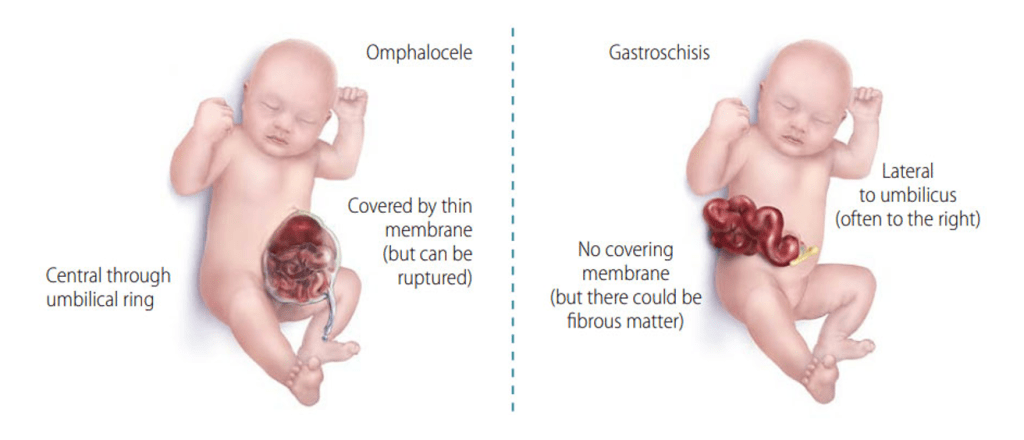
Explanation: Gastroschisis is a congenital abdominal wall defect where the intestines, and sometimes other organs, protrude through the abdominal wall into the umbilical cord. The defect is not covered by a sac, and the intestines are exposed to the amniotic fluid, which can cause ischaemia, adhesions, and intestinal damage. A prenatal ultrasound can show the defect during pregnancy, and it is visible at birth.
A) is incorrect as omphalocele is a congenital defect where abdominal contents protrude through the umbilical cord and are covered by a sac.
C) is incorrect because an umbilical hernia is a small bulge at the belly button, often present in infants, but it is not a congenital defect of the abdominal wall like gastroschisis.
D) is incorrect because a diaphragmatic hernia involves abdominal organs protruding into the chest through a hole in the diaphragm, not through the abdominal wall.
E) is incorrect because Meckel’s diverticulum is a congenital outpouching of the ileum and is unrelated to abdominal wall defects.


Question 11:
Answer: B) Accumulation of ammonia in the bloodstream
Explanation: Hepatic encephalopathy occurs due to the failure of the liver to detoxify ammonia and other neurotoxic substances produced in the gut. In a healthy liver, ammonia is converted into urea in the urea cycle, which is then excreted in urine by the kidneys. In cirrhosis or severe liver disease, hepatocytes lose their ability to metabolise ammonia. Additionally, portal hypertension diverts blood away from the liver (via portosystemic shunting), allowing ammonia to bypass detoxification. Ammonia crosses the blood-brain barrier and disrupts normal neurotransmission. It alters astrocyte function by causing swelling (due to glutamine accumulation) and interferes with synaptic signalling, leading to confusion, lethargy, and in severe cases, coma.
A) is incorrect because bilirubin is a marker of liver dysfunction, its elevation causes jaundice and does not directly affect brain function.
C) is incorrect because portal hypertension contributes indirectly by shunting blood away from the liver, but it is not the direct cause of HE.
D) is incorrect because cirrhosis leads to reduced protein synthesis, not an increase.
E) is incorrect because obstruction of bile flow causes post-hepatic jaundice but does not lead to HE.
Question 12:
Answer: C) Portal hypertension and hypoalbuminemia
Explanation: Ascites is the pathological accumulation of fluid in the peritoneal cavity. Portal hypertension: Cirrhosis causes fibrosis and scarring of the liver, increasing resistance to blood flow in the portal vein. This leads to elevated hydrostatic pressure in the splanchnic (abdominal) circulation, causing fluid to leak out of blood vessels into the peritoneal cavity. The damaged liver reduces albumin production, which decreases oncotic pressure (the ability of the blood to retain fluid). This allows even more fluid to escape into the peritoneal space. The liver’s lymphatic drainage is overwhelmed, and lymph leaks into the peritoneal cavity.
A) is incorrect because decreased ammonia clearance causes HE, not ascites.
B) is incorrect because cirrhosis usually reduces bile production.
D) is incorrect because excessive protein intake is unrelated to ascites formation.
E) is incorrect because obstruction of bile flow leads to jaundice, not ascites.
Question 13:
Answer: E) HPS involves intrapulmonary vasodilation and hypoxemia, while PPH involves pulmonary artery hypertension.
Explanation: In Hepatopulmonary Syndrome (HPS) liver dysfunction and portal hypertension lead to the release of vasodilatory mediators (e.g., nitric oxide) into the bloodstream. These mediators cause dilation of pulmonary capillaries, which disrupts normal oxygen exchange by allowing blood to bypass alveoli without proper oxygenation (ventilation-perfusion mismatch) because blood is passing too quickly for oxygenation to occur this leads to hypoxaemia (low blood oxygen levels).
In Portopulmonary Hypertension (PPH) portal hypertension increases blood flow through the pulmonary circulation, causing remodelling of pulmonary arteries and increased vascular resistance. This leads to elevated pulmonary artery pressures and strain on the right heart causing right heart failure symptoms.
A) is incorrect because HPS this statement describes PPH, not HPS.
B) is incorrect because both occur in chronic liver disease.
C) is incorrect because neither condition involves bile.
D) is incorrect because both conditions can be partially reversible with treatment, but this is not the defining difference.
Question 14:
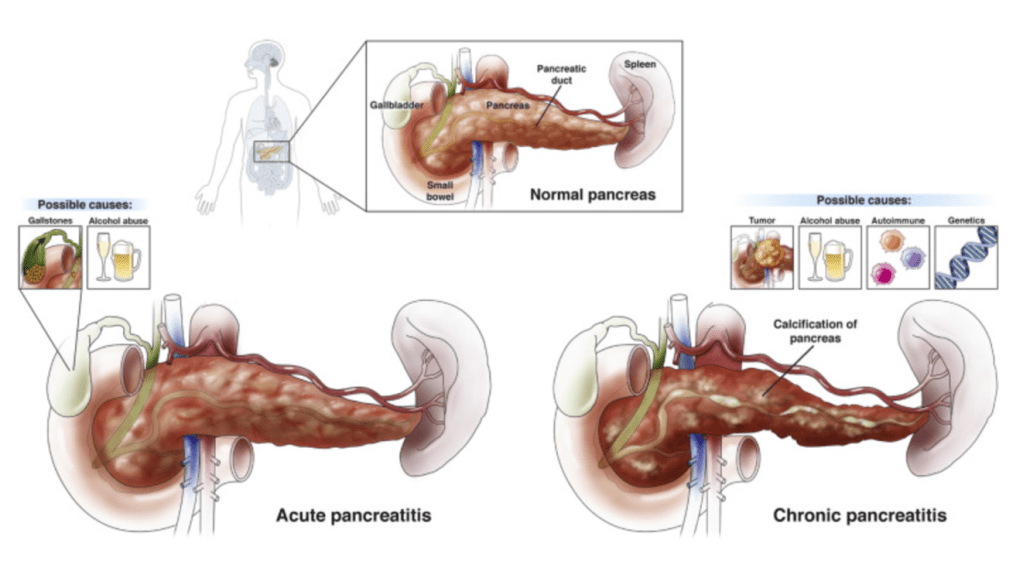
Answer: D) Serum amylase/lipase >3 times the upper limit of normal
Explanation: Serum amylase and lipase are the primary diagnostic markers for acute pancreatitis. Lipase is more specific to the pancreas than amylase and remains elevated for longer. A level >3 times the upper limit of normal is highly suggestive of pancreatitis. Imaging (e.g., CT, MRI, or ultrasound) is used to confirm the diagnosis and identify complications, but elevated lipase/amylase is the key diagnostic feature.
A) is incorrect because elevated serum bilirubin may indicate biliary obstruction or liver involvement but is not specific to pancreatitis.
B) is incorrect because although gallstones are a common cause of pancreatitis they are not diagnostic of the condition itself.
C) is incorrect because jaundice suggests biliary obstruction, which can occur in pancreatitis but is not diagnostic.
E) is incorrect because steatorrhea is a feature of chronic pancreatitis, not acute pancreatitis.
Question 15:
Answer: B) Administer IV crystalloid fluids (Ringer’s lactate)
Explanation: Upper abdominal pain radiating to the back suggests pancreatitis and lipase level 5 times the upper limit of normal suggests acute pancreatitis. There is no curative medication for acute pancreatitis but early and aggressive fluid resuscitation with IV crystalloids (e.g., Ringer’s lactate) helps restore intravascular volume, supports perfusion of the pancreas, and prevents complications like organ failure. The goal is to maintain a heart rate <120/min, urinary output >0.5-1.0 ml/kg/h, and hematocrit between 35-44%.
A) is incorrect because antibiotics are not routinely used unless there is evidence of infected necrosis.
C) is incorrect because Endoscopic retrograde cholangiopancreatography (ERCP) is indicated only in cases of gallstone pancreatitis with cholangitis or persistent biliary obstruction.
D) is incorrect because Schedule Kausch-Whipple resection is a surgical treatment for pancreatic cancer, not acute pancreatitis, it involves removal of the head of the pancreas, part of the duodenum, gallbladder, and bile duct.
E) is incorrect because pancreatic enzyme replacement therapy is used for chronic pancreatitis with malabsorption, not acute pancreatitis.
Question 16:
Answer: A) Intermittent or continuous upper abdominal pain
Explanation: Chronic pancreatitis is characterised by recurrent or persistent upper abdominal pain, often radiating to the back. Pain may be continuous or occur in episodes of acute exacerbations. Over time, it can lead to complications like steatorrhea, malnutrition, and diabetes.
B) is incorrect because persistent jaundice is more commonly associated with pancreatic cancer or biliary obstruction.
C) is incorrect because serum amylase/lipase >3 times the upper limit of normal are markers of acute pancreatitis and are often normal in chronic pancreatitis due to loss of acinar cell function.
D) is incorrect because acute organ failure is a feature of severe acute pancreatitis, not chronic pancreatitis.
E) is not the best answer while diabetes is common in chronic pancreatitis, it often coexists with malabsorption due to exocrine insufficiency.
Question 17:
Answer: C) Smoking and alcohol consumption
Explanation: Smoking and alcohol are the primary risk factors for oesophageal squamous cell carcinoma. These factors cause chronic irritation of the oesophagus, leading to cellular changes that increase the risk of malignancy. The carcinogenic compounds in tobacco and alcohol can damage the DNA of oesophageal epithelial cells, causing mutations that lead to cancer.
A) is incorrect because GORD (gastroesophageal reflux disease) leads to Barrett’s oesophagus, where the normal squamous epithelium of the oesophagus is replaced by columnar epithelium (glandular metaplasia). While Barrett’s oesophagus is a risk factor for adenocarcinoma, GERD itself is not a direct risk factor for oesophageal squamous cell carcinoma (SCC). The squamous cell carcinoma is more closely associated with environmental factors like smoking and alcohol use.
B) is incorrect because Helicobacter pylori infection is a known risk factor for gastric adenocarcinoma and gastric lymphoma (MALT), but it is not a significant risk factor for oesophageal squamous cell carcinoma.
D) is not the best answer as although squamous dysplasia is a premalignant lesion that can progress to squamous cell carcinoma, it is not the most significant risk factor compared to smoking and alcohol. Dysplasia indicates abnormal cellular changes, but it’s more of a precursor to cancer rather than a direct cause.
E) is incorrect because Barrett’s oesophagus is a condition where squamous epithelium is replaced by columnar epithelium, often due to chronic acid reflux (GORD). While Barrett’s oesophagus increases the risk of adenocarcinoma, it does not significantly affect the development of oesophageal squamous cell carcinoma.
Question 18:
Answer: E) Intestinal type adenocarcinoma
Explanation: Intestinal-type adenocarcinoma is the most common form of gastric cancer linked to Helicobacter pylori infection. The infection causes chronic gastritis, leading to intestinal metaplasia, dysplasia, and eventually adenocarcinoma. This form of cancer arises from glandular epithelium that forms glands.
A) is incorrect because diffuse type adenocarcinoma is typically associated with genetic mutations and family history, rather than Helicobacter pylori infection. This type of cancer is characterized by poorly cohesive malignant cells, and it does not arise from the dysplasia seen in intestinal-type adenocarcinoma.
B) is not the best answer because although MALT lymphoma, is associated with H. pylori infection, intestinal-type adenocarcinoma is the most common gastric cancer linked to H. pylori, making this option less accurate in the context of the most common cancer.
C) is incorrect because Gastrointestinal stromal tumour (GIST) are mesenchymal tumours and are unrelated to H. pylori infection.
D) is incorrect because neuroendocrine tumours in the stomach can occur in the context of gastrin-producing tumours or atrophic gastritis but are not typically linked to H. pylori infection. These tumours are often seen in conditions like Zollinger-Ellison syndrome.
Question 19:
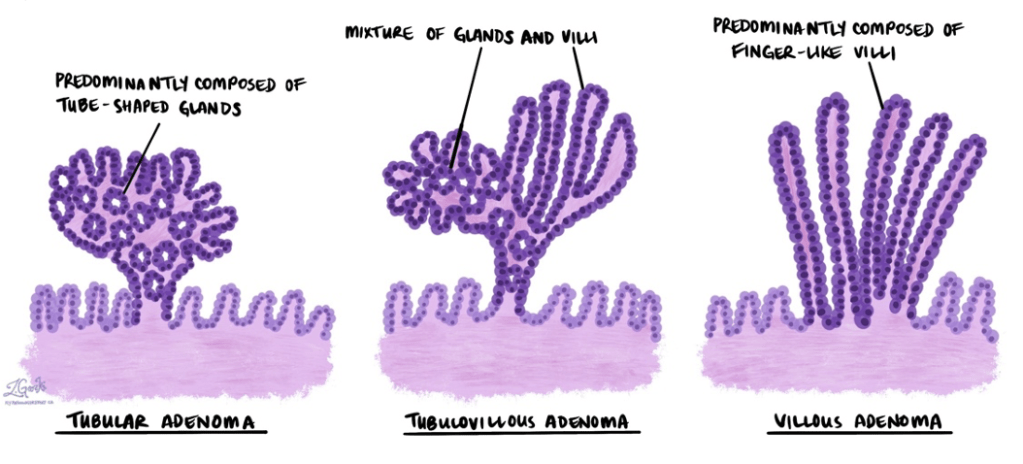
Answer: D) Villous adenoma
Explanation: Villous adenomas are the most likely to undergo malignant transformation and progress to carcinoma. Their structure facilitates rapid cellular turnover and dysplasia, making them the most dangerous type of adenoma.
A) is incorrect because tubular adenomas are the most common type of colonic adenoma and generally have a low risk of malignant transformation, especially when dysplasia is low-grade.
B) is incorrect because tubulovillous adenoma with high-grade dysplasia have an intermediate malignant potential. The presence of high-grade dysplasia increases the risk, but it is still lower than that of villous adenomas.
D) is incorrect because metaplastic polyps are generally considered non-neoplastic and carry no significant malignant potential.
E) is incorrect because hyperplastic polyps are like metaplastic polyps, they are benign lesions and do not progress to cancer.
Question 20:
Answer: B) Hereditary non-polyposis colorectal cancer (HNPCC)
Explanation: HNPCC, also known as Lynch syndrome, is the most common inherited cause of colorectal cancer. It is characterised by microsatellite instability (MSI): A hallmark of defective DNA mismatch repair (MMR) genes. It involves mutations in DNA mismatch repair genes: MSH2 (~60% of cases), MLH1 (~30% of cases) and other genes such as MSH6 and PMS2. It is inherited in autosomal dominant manner and right-sided colon cancers are more common.
A) is incorrect because FAP is caused by mutations in the APC gene, leading to hundreds to thousands of adenomatous polyps. Microsatellite instability is not a feature.
C) is incorrect because Peutz-Jeghers syndrome does not involve mutations in MMR and is characterised by hamartomatous polyps and mucocutaneous pigmentation.
D) is incorrect because Lynch syndrome is another name for HNPCC.
E) is incorrect because juvenile polyposis syndrome is characterized by hamartomatous polyps and mutations in SMAD4, not MMR genes.
Question 21:
Answer: E) A and B
Explanation: Astrovirus typically causes mild gastroenteritis, but certain populations are at higher risk of severe dehydration: Young children have an immature immune systems make them more susceptible to dehydration. Elderly individuals have a weakened immunity, and comorbidities increase the risk of complications.
Pregnant women do not specifically have a higher risk for severe astrovirus infection.
Question 22:
Answer: A) Norovirus
Explanation: Norovirus is the leading cause of viral gastroenteritis across all age groups worldwide. It is highly contagious and spread via the faecal-oral route, contaminated food/water, or contact with infected surfaces. Norovirus involves sudden onset of vomiting, diarrhoea (non-bloody), abdominal pain, and nausea and is responsible for outbreaks in crowded settings such as cruise ships and nursing homes.
B) is incorrect because E-coli cause gastroenteritis, it is bacterial in origin and not viral. It is a common cause of traveller’s diarrhoea.
C) is not the best answer because Rotavirus is the leading cause of severe gastroenteritis in young children, particularly in unvaccinated populations.
D) is not the best answer because Adenovirus is associated with gastroenteritis in infants and children.
E) is not correct because Rhinovirus causes the common cold, not gastroenteritis.
Question 23:
Answer: D) Bacillus cereus
Explanation: Bacillus cereus has two forms: the emetic form linked to reheated rice, causes vomiting and diarrhoeal form linked to contaminated meat or vegetables, causes watery diarrhoea.
A) is incorrect because Yersinia enterocolitica causes watery or bloody diarrhoea, often linked to pork or contaminated milk and is associated with pseudoappendicitis.
B) Is incorrect because although Vibrio cholerae causes severe watery diarrhoea resembling “rice-water stools,” it is associated with contaminated water or seafood, not fried rice.
C) is incorrect because Shigella causes bloody diarrhoea with fever and abdominal pain, often linked to poor hygiene.
E) is incorrect because Clostridium perfringens causes watery diarrhoea due to toxin production, often linked to improperly stored meat dishes.
Question 24:
Answer: C) Listeria monocytogenes
Explanation: Listeria monocytogenes is associated with consumption of unpasteurised dairy products and deli meats. Symptoms include fever, muscle aches, and mild diarrhoea. In pregnancy, Listeria can cause miscarriage, stillbirth, or neonatal sepsis.
A) is incorrect because Salmonella is more commonly linked to eggs or poultry.
B) is incorrect because Campylobacter jejuni causes bloody diarrhoea and abdominal pain but is not typically linked to unpasteurised cheese.
D) is incorrect because Vibrio cholerae causes watery diarrhoea, not systemic symptoms.
E) is incorrect because Clostridium perfringens causes mild watery diarrhoea after consuming improperly stored meat e.g., in buffets.
Question 25:
Answer: B) Luminal obstruction
Explanation: The initial step in appendicitis is luminal obstruction. This is typically caused by fecaliths (hardened faecal matter), lymphoid hyperplasia (common in children due to immune activity), or less commonly by tumours, parasites, or foreign bodies. Obstruction traps normal secretions (mucus) produced by the appendix, leading to increased intraluminal pressure. The pressure compromises venous drainage first (veins are more collapsible than arteries), leading to congestion and swelling of the appendix wall. The trapped mucus also provides a medium for bacterial overgrowth, including organisms like Escherichia coli and Bacteroides fragilis, which exacerbate inflammation. As inflammation progresses, neutrophils infiltrate the mucosa, leading to acute appendicitis.
A) is incorrect because bacterial overgrowth is a later stage caused by an increase in mucus which creates an environment that allows bacteria to flourish.
C) is incorrect because ischaemia of the appendix wall is a later stage caused by increased intraluminal pressure compressing blood vessels.
D) is incorrect because perforation of the appendix is a late complication after necrosis of the appendix wall.
E) is incorrect because necrosis of the appendix occurs after prolonged ischaemia due to prolonged pressure and reduced blood flow.
Question 26:
Answer: E) Primary Sclerosing Cholangitis (PSC)
Explanation: PSC is a chronic, progressive disease characterised by inflammation, fibrosis, and stricturing of both intrahepatic and extrahepatic bile ducts. It is strongly associated with inflammatory bowel disease (IBD), particularly ulcerative colitis (UC) and is more common in males and is characterised by a cholestatic pattern (elevated ALP and bilirubin). Chronic inflammation leads to progressive bile duct destruction, fibrosis, and cholestasis and potentially cholangiocarcinoma.
A) is incorrect because Primary Biliary Cholangitis (PBC) is not usually associated with ulcerative colitis, it is an autoimmune condition seen more commonly in middle-aged women and is characterised by anti-mitochondrial antibodies (AMA) and intrahepatic bile duct destruction, although it still presents with a cholestatic pattern (elevated ALP and bilirubin).
B) is incorrect because autoimmune hepatitis involves immune-mediated hepatocyte destruction. It presents with elevated transaminases, not the cholestatic pattern (elevated ALP and bilirubin) seen in PSC.
C) is incorrect because patients with alcoholic hepatitis present with a history of heavy alcohol use, jaundice, and AST > ALT. It does not involve bile duct disease, and imaging would not show beading, it is unrelated to IBD or bile duct pathology, instead it causes steatosis.
D) is incorrect because Wilson’s disease involves copper accumulation and presents with neurological symptoms.
Question 27:
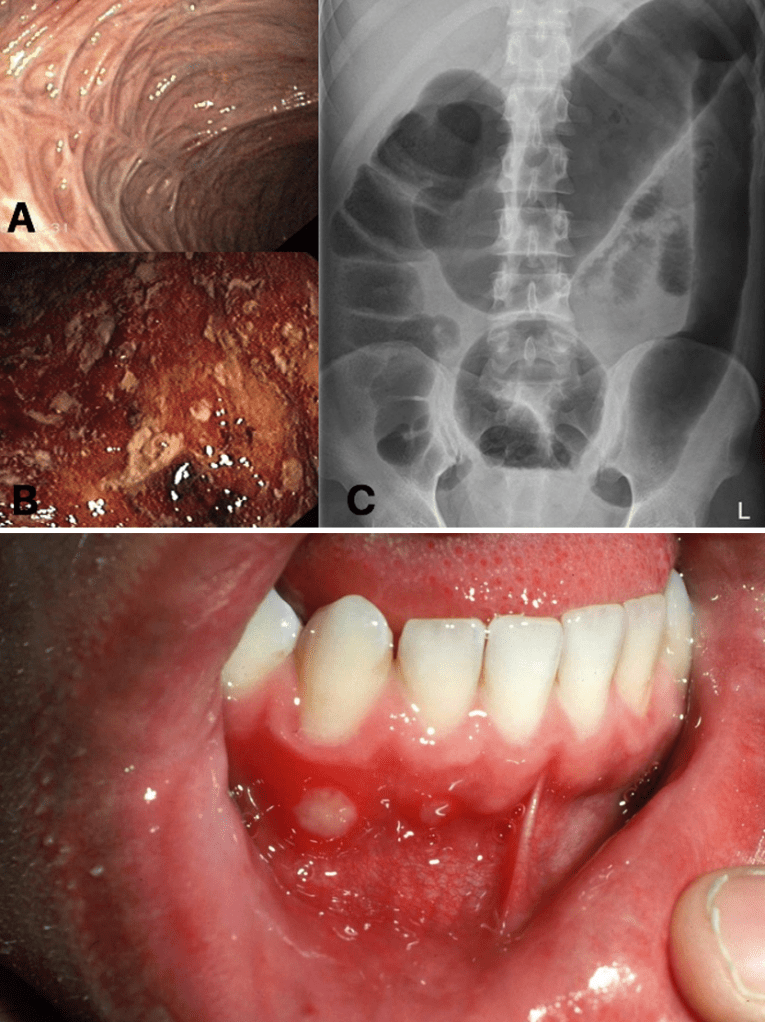
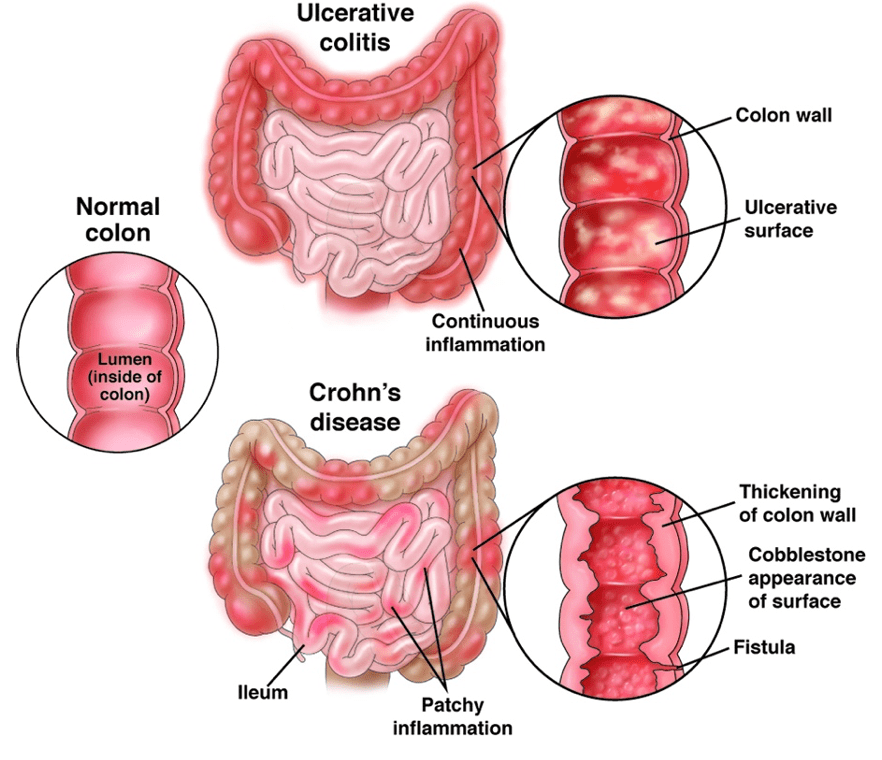
Answer: C) Ulcerative Colitis
Explanation: Ulcerative Colitis is a chronic inflammatory condition of the colon characterised by continuous superficial inflammation in the colon, predominantly the sigmoid colon. Symptoms include bloody diarrhoea, abdominal pain, aphthous ulcers, and tenesmus. Colonoscopy shows continuous inflammation confined to the colon and plain films highlight the loss of haustra in the colon.
A) is incorrect because Crohn’s Disease causes patchy, transmural inflammation, characterised by ‘skip lesions’ that can occur anywhere in the GI tract.
B) is incorrect because IBS is a functional disorder without structural abnormalities or blood in the stool.
D) is incorrect because microscopic Colitis presents with watery diarrhoea not blood in the stool
E) is incorrect because Coeliac Disease involves the small intestine and presents with malabsorption symptoms such as steatorrhea.
Aphthous ulcers
Question 28:
Answer: A) Diverticulitis
Explanation: Diverticulitis is an inflammation or infection of diverticula, commonly affecting the sigmoid colon. Symptoms include eft lower quadrant pain, fever, and changes in bowel habits (constipation or diarrhoea). CT shows colonic wall thickening and peri-colonic fat stranding. Fever indicates inflammation.
B) Diverticulosis is incorrect because it refers to the presence of diverticula that is characterised by the presence of multiple outpouchings at weak points in the colonic wall with no inflammation.
C) is incorrect because colorectal cancer typically presents with weight loss, rectal bleeding, and a change in bowel habits without fever.
D) is incorrect because IBS does not cause fever although it may cause changes in bowel habits.
E) IBD is incorrect because it presents with chronic symptoms and often involves the entire colon or small intestine.

Question 29:
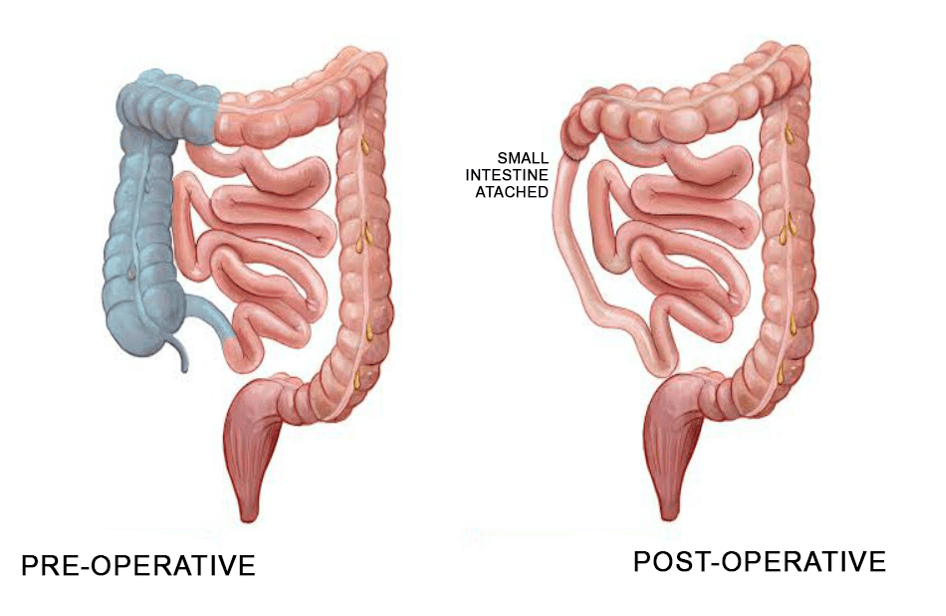
Answer: D) Sigmoid volvulus
Explanation: A coffee bean sign is shown which is an indication of a sigmoid volvulus, which is a condition where the sigmoid colon twists on its mesentery, causing obstruction.
A) is incorrect because thumbprinting is associated with colitis.

B) is incorrect because pneumoperitoneum is associated with Rigler’s sign characterised by the presence of air in the bowel wall (double wall sign).
C) is incorrect because caecal volvulus presents with the kidney bean sign.

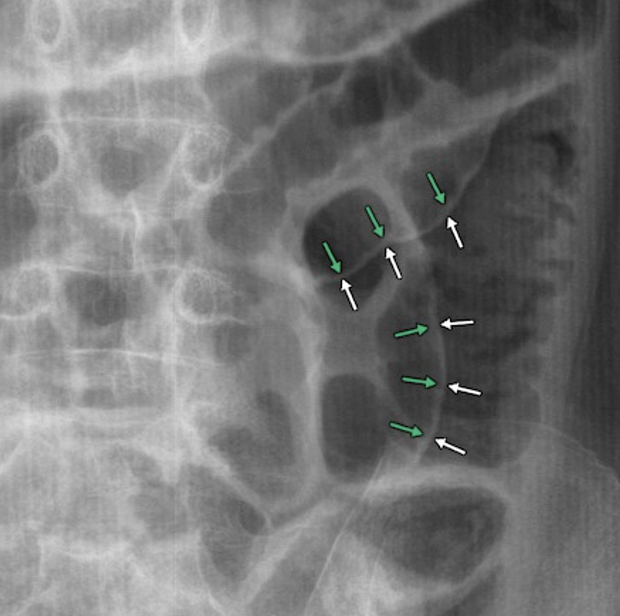
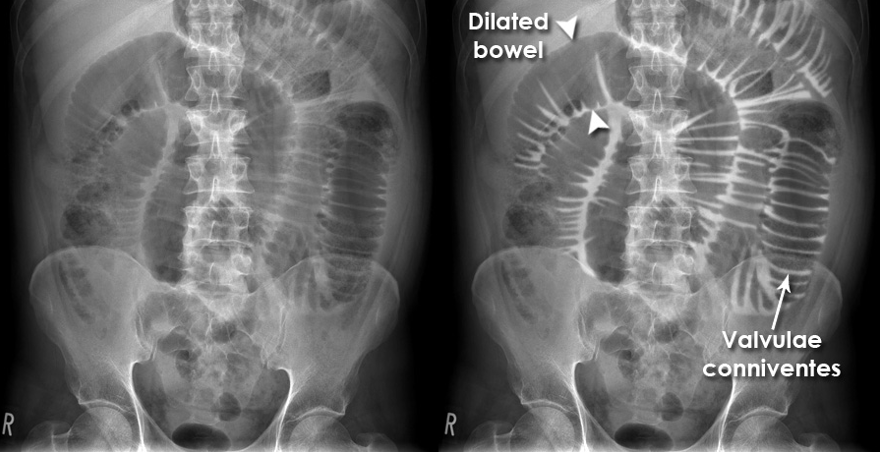
E) is incorrect because small bowel obstruction shows dilatation of more than 3 cm and is characterised by the presence of plicae circularis/valvulae conniventes.
Question 30:
Answer: C) Colonoscopy with Biopsy
Explanation: Colonoscopy with Biopsy is confirmatory because it allows the direct visualisation of the colon, Crohn’s Disease is characterised by patchy inflammation, skip lesions, strictures and fistulas in the entire GI tract, whilst ulcerative Colitis shows continuous inflammation in the colon.
A) is incorrect because a complete blood count (CBC) may show anaemia or leucocytosis but is non-specific to IBD
B) is incorrect because faecal Calprotectin indicates intestinal inflammation but does not confirm IBD, it does however differentiate it from IBS.
D) is incorrect because C-Reactive Protein (CRP) reflects systemic inflammation but is not specific to the gut.
E) is incorrect because a stool culture rules out infectious causes of diarrhoea but does not diagnose IBD.
Question 31:
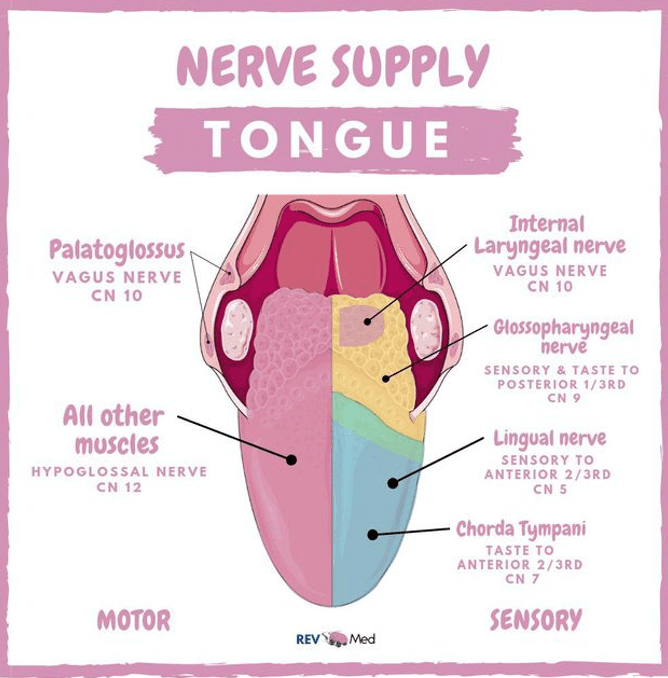
Answer: C) The anterior 1/3 of the tongue receives general sensation from the lingual nerve (CN V3) and taste sensation from the chorda tympani (CN VII).
Explanation: The sensory innervation of the tongue is provided by multiple cranial nerves. The anterior 1/3 of the tongue receives general sensation from the lingual nerve, which is a branch of the mandibular division of the trigeminal nerve (CN V3), and taste sensation from the chorda tympani, a branch of the facial nerve (CN VII).
Option A is incorrect because the glossopharyngeal nerve (CN IX) does not supply the anterior 1/3 of the tongue with taste or general sensation. It is responsible for taste sensation on the posterior 1/3.
Option B is incorrect because the posterior 1/3 of the tongue receives both general sensation and taste sensation from the glossopharyngeal nerve (CN IX), not the lingual nerve or chorda tympani.
Option D is incorrect because the posterior 1/3 of the tongue does not receive sensation from the lingual nerve. It is instead innervated by the glossopharyngeal nerve for both general sensation and taste sensation.
Option E is incorrect because the vagus nerve (CN X) does not provide taste sensation to the posterior 1/3 of the tongue. It is responsible for taste sensation from the epiglottis, not the posterior tongue.
Question 32:
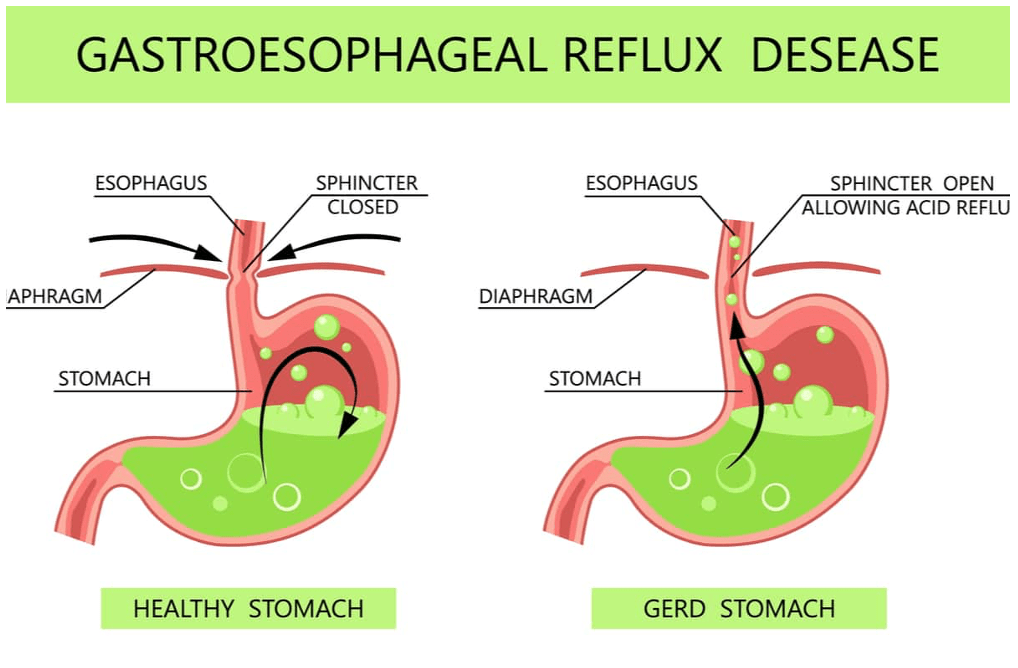
Answer: A) GORD is primarily caused by an abnormal relaxation of the lower oesophageal sphincter (LOS) and can be exacerbated by obesity, smoking, and alcohol consumption.
Explanation: GORD occurs when stomach acid frequently flows back into the oesophagus due to a dysfunction of the lower oesophageal sphincter (LOS), leading to symptoms like heartburn and regurgitation. Factors such as obesity, smoking, and alcohol consumption can exacerbate this condition by weakening the LOS or increasing gastric acid production.
Option B is incorrect because proton pump inhibitors (PPIs) are effective in treating GORD-related symptoms by significantly reducing gastric acid production, which helps heal the oesophagus and reduce symptoms of reflux.
Option C is incorrect because GORD can be diagnosed clinically based on the patient’s symptoms, and esophagogastroduodenoscopy (OGD) is not necessary for diagnosis unless there are alarm features (e.g., weight loss, dysphagia, or gastrointestinal bleeding). Another way to diagnose GORD is via a 24hours pH probe.
Option D is incorrect because lifestyle modifications, such as weight loss, dietary changes, and elevating the head of the bed, are essential in managing GORD and can reduce the frequency and severity of symptoms.
Option E is incorrect because Barrett’s oesophagus, a complication of chronic GORD, is a premalignant condition that increases the risk of oesophageal adenocarcinoma, particularly with prolonged acid exposure.
Question 33:
Which of the following is the most appropriate next step in the diagnosis and management of this patient?
Answer: C) Perform an esophagogastroduodenoscopy (OGD) to evaluate for peptic ulcer disease, excluding malignancy and obtaining a biopsy for histological confirmation.
Explanation: Given the patient’s symptoms of weight loss, early satiety, vomiting, black stools (potentially indicating gastrointestinal bleeding), and a family history of gastric carcinoma, the most appropriate next step is to perform an esophagogastroduodenoscopy (OGD). This will allow for direct visualisation of the stomach, assessment for peptic ulcer disease, and an evaluation for any malignancy. A biopsy should be obtained if a suspicious lesion is identified for histological confirmation.
Option A is incorrect because, while peptic ulcer disease (PUD) is a possibility, the patient’s symptoms (such as unintentional weight loss and black stools) raise concern for malignancy, so empirical treatment without a clear diagnosis would not be appropriate.
Option B is incorrect because chemotherapy is not the first-line management approach without a confirmed diagnosis of gastric cancer. An OGD and biopsy are needed to confirm malignancy before considering chemotherapy.
Option D is incorrect because a barium swallow is not the best choice for diagnosing gastric cancer or peptic ulcer disease. An OGD provides a more accurate assessment and allows for biopsy if necessary.
Option E is incorrect because referring the patient for surgery without a definitive diagnosis would be premature. Gastric cancer requires confirmation through diagnostic testing, such as OGD with biopsy, before considering surgical intervention.
Question 34:
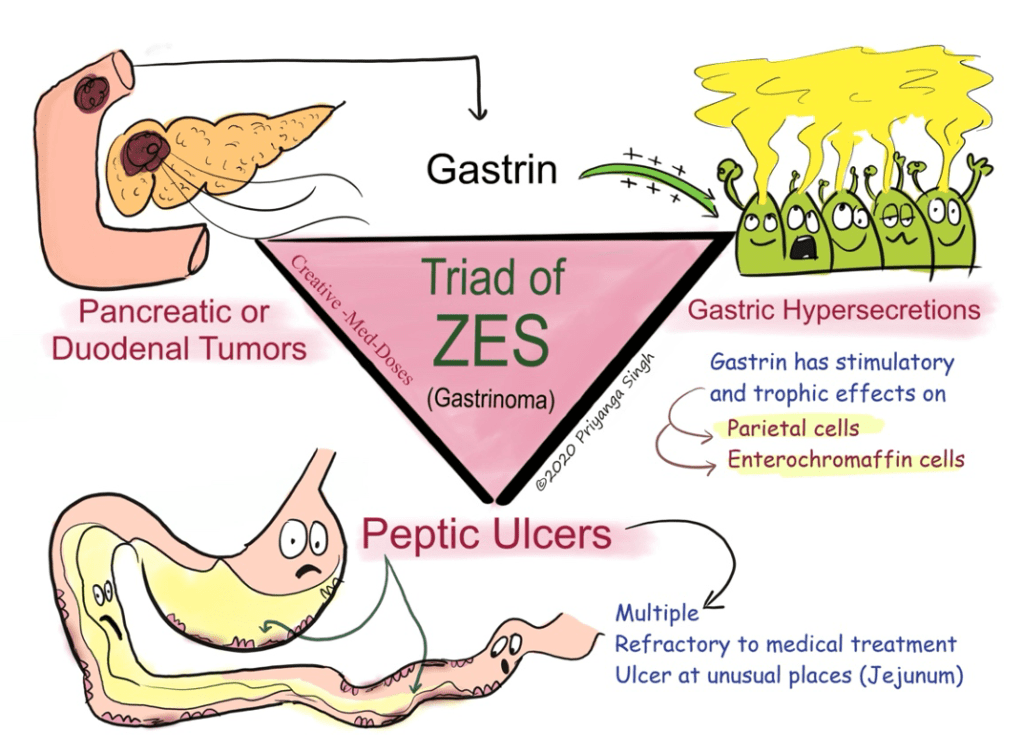
Answer: A) A mutation in the MEN1 gene, which results in the development of multiple endocrine neoplasia type I, leading to the formation of a Zollinger Ellison Syndrome.
Explanation: This patient’s symptoms, including recurrent peptic ulcers, diarrhoea, abdominal pain, weight loss, and elevated serum gastrin levels, suggest Zollinger-Ellison syndrome, a condition commonly associated with tumours (gastrinomas) that secrete excessive amounts of gastrin. The most likely cause of these tumours is a mutation in the MEN1 gene, which is responsible for multiple endocrine neoplasia type I. MEN1 leads to the development of various endocrine tumours, including gastrinomas, which result in hypergastrinemia and subsequent symptoms.
Option B is incorrect because overexpression of the CagA protein by Helicobacter pylori is associated with gastric inflammation and increased risk of peptic ulcers, but it does not typically cause marked elevation in serum gastrin levels. Although in rare instances, H.pylori infection can lead to the development of gastric adenocarcinoma, that stem mentions that the patient has a family history of endocrine disorders, thus option A is the best answer.
Option C is incorrect because autoimmune destruction of parietal cells, leading to pernicious anaemia and B12 deficiency, causes elevated gastrin levels, but it is not typically associated with symptoms like diarrhoea and weight loss to the extent seen in this patient. This mechanism also does not explain the gastrin-producing tumours characteristic of Zollinger-Ellison syndrome.
Option D is incorrect because mutations in the APC gene are linked to familial adenomatous polyposis and colorectal cancer, not to the formation of gastric adenomas that secrete excessive gastrin.
Option E is incorrect because somatostatin is a hormone that inhibits the release of gastrin. An upregulation of the SSTR2 receptor would be more likely to reduce gastrin secretion, not cause hypergastrinemia.
Question 35:
Answer: A) 13C-urea breath test, as it is a non-invasive test that directly detects the presence of active H. pylori infection.
Explanation: The 13C-urea breath test is the most appropriate first-line non-invasive test for diagnosing Helicobacter pylori infection. It detects active infection by measuring the breakdown of urea by the H. pylori bacteria, which produces carbon dioxide. This test is highly sensitive, specific, and can be used to confirm current infection in patients with dyspepsia.
Option B is incorrect because while the faecal antigen test is also a non-invasive and accurate test for detecting H. pylori, it is typically used for follow-up after treatment, not as the first-line test.
Option C is incorrect because serology (IgG) detects antibodies against H. pylori, indicating past or current infection, but it cannot distinguish between active and past infection. It is less reliable for diagnosing current infection compared to the 13C-urea breath test.
Option D is incorrect because a rapid urease test on gastric biopsy requires invasive endoscopy and is typically used when endoscopy is already being performed for other reasons, such as when complications are suspected or when biopsy is necessary.
Option E is incorrect because starting a combination of antibiotics and a proton pump inhibitor (PPI) is not part of the diagnostic process. Treatment should only begin after confirmation of H. pylori infection. Treatment includes triple therapy: Amoxicillin, Clarithromycin & Proton Pump Inhibitors.

Question 36:
Answer: B) In coeliac disease, gliadin, a component of gluten, triggers an immune response that leads to the production of IgA antibodies against both gliadin and transglutaminase, resulting in tissue damage.
Explanation: Coeliac disease is an autoimmune disorder in which the ingestion of gluten (specifically gliadin) triggers an immune response in genetically predisposed individuals. This response involves the production of IgA antibodies against both gliadin and tissue transglutaminase (tTG). These antibodies mediate inflammation and lead to the damage of the small intestine’s villi, impairing nutrient absorption and causing the symptoms seen in coeliac disease, such as diarrhoea, weight loss, and anaemia.
Option A is incorrect because coeliac disease is not primarily mediated by IgE antibodies, which are typical of allergic reactions. The immune response in coeliac disease involves IgA antibodies, not IgE, and is more related to autoimmune processes rather than mast cell degranulation.
Option C is incorrect because coeliac disease is not caused by a viral infection like rotavirus. While infections can trigger or exacerbate the disease, the underlying cause is the immune response to gluten, not a viral infection.
Option D is incorrect because the immune response in coeliac disease is not directed against the HLA-DQ2/DQ8 receptors themselves, but rather the immune system reacts to gluten, leading to tissue damage in individuals with specific HLA genetic markers. The HLA-DQ2/DQ8 genes are associated with the disease but are not the target of the immune response.
Option E is incorrect because coeliac disease is not caused by a deficiency of vitamin D, although vitamin D deficiency may occur as a result of malabsorption in coeliac disease. The primary pathophysiology involves an immune response to gluten, leading to intestinal damage.
Question 37:
Answer: B) Foods containing high levels of fructose, lactose, oligosaccharides, and polyols, as these ferment in the bowel and cause luminal distension.
Explanation: The diet being referred to is the FODMAP diet, which involves avoiding foods that are high in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs). These carbohydrates are poorly absorbed in the small intestine and undergo fermentation in the colon by harmful bacteria, leading to gas production, bloating, and abdominal distension. Foods high in fructose, lactose, oligosaccharides, and polyols are commonly restricted in this diet to alleviate IBS symptoms.
Option A is incorrect because foods high in protein, such as meat and eggs, do not significantly contribute to gas production or fermentation in the bowel. While they can be involved in gut inflammation in some individuals, they are not the primary focus of this specific diet.
Option C is incorrect because while high-fibre foods like whole grains and legumes may affect gut motility, they are not specifically targeted for their ability to ferment and cause bloating. In fact, some high-fibre foods can be included in the FODMAP diet if they are low in fermentable carbohydrates.
Option D is incorrect because high-fat foods, such as butter and oils, do not cause fermentation in the bowel. While high-fat foods may slow digestion, they are not a primary cause of bloating related to fermentation.
Option E is correct because foods rich in soluble fibre, such as oats and beans, are also typically high in FODMAPs and are often restricted on a low FODMAP diet due to their potential to cause gas production and bloating however option B is the better answer since it includes the different components of the FODMAP diet.
Question 38:
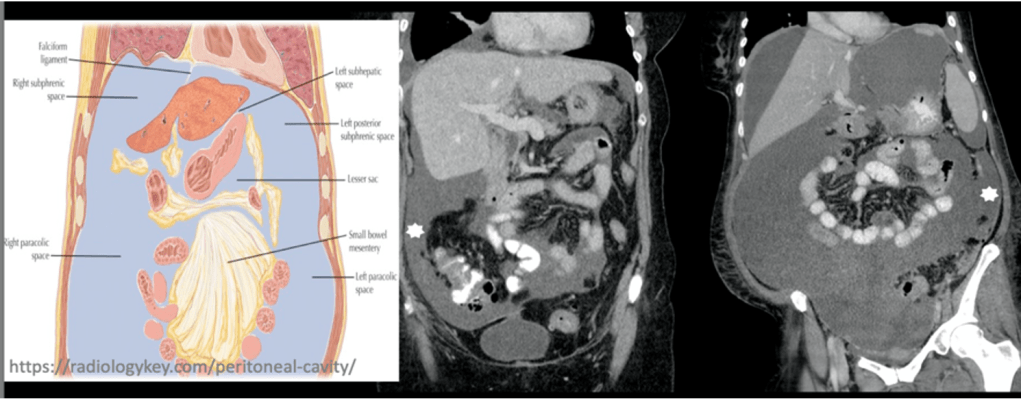
Answer: C) Fluid from the pelvis drains into the right para-colic space and subsequently ascends into the right sub-phrenic space.
Explanation: The peritoneal fluid from the pelvis can drain into the para-colic spaces, which are located next to the colon. Specifically, fluid from the pelvic cavity can move into the right para-colic space and then ascend into the right sub-phrenic space, facilitating the spread of infection or tumour. The para-colic spaces are important anatomical areas for the spread of diseases within the peritoneal cavity.
Option A is incorrect because the left sub-phrenic space does not directly communicate with the pelvis via the gastro-hepatic ligament. The peritoneal fluid’s movement is more complex and involves different routes for spread.
Option B is incorrect because the left sub-hepatic space is not directly continuous with the right para-colic space. The anatomical barrier between these regions limits direct spread of disease between the two spaces.
Option D is incorrect because Morrison’s Pouch, being the most dependent part of the abdomen, actually allows for the accumulation of fluid and can facilitate the spread of infection or tumour rather than preventing it. This pouch connects the right sub-hepatic space with the rest of the abdominal cavity, making it an important pathway for the spread of disease.
Option E is incorrect because peritoneal fluid does accumulate in the paracolic gutters, and it can indeed contribute to the spread of infection or tumour to the sub-phrenic spaces. The paracolic gutters provide a route for fluid and disease spread throughout the abdomen.
Question 39:
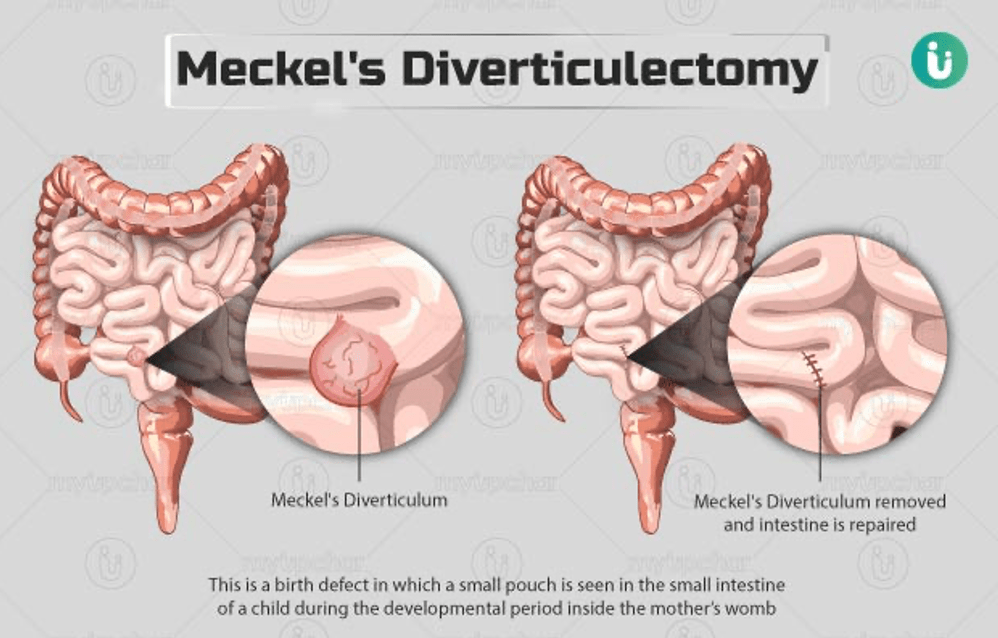
Answer: E) Meckel’s Diverticulum is a failure of the vitellointestinal duct to close, leading to persistent communication between the yolk sac and the midgut, which may cause bleeding, pain, and mimic appendicitis.
Explanation: Meckel’s Diverticulum is a congenital condition caused by the incomplete closure of the vitellointestinal duct (also called the omphalomesenteric duct). This failure results in a diverticulum (outpouching) of the ileum that may contain ectopic tissue, such as gastric mucosa, which can lead to complications like bleeding, pain, and even mimic appendicitis. The condition is often asymptomatic, but when symptomatic, it can cause intestinal obstruction, bleeding, or inflammation.
Option A is incorrect because Meckel’s Diverticulum is not related to an abnormality of the abdominal wall or a para-umbilical herniation. It specifically results from the persistence of the vitellointestinal duct. This is referring to gastroschisis.
Option B is incorrect because while Meckel’s Diverticulum can present with abdominal pain, it is not caused by a malrotation of the bowel or by a defect in the intestinal vasculature. It does not typically present with large abdominal distension and vomiting as primary symptoms.
Option C is incorrect because Meckel’s Diverticulum is not associated with omphalocele, which is a condition where abdominal contents protrude through the umbilical cord and are covered by a membrane. Meckel’s Diverticulum arises from the persistence of the vitellointestinal duct and is located in the ileum.
Option D is incorrect because Meckel’s Diverticulum is not associated with gastroschisis, a condition where bowel herniates through an abdominal wall defect without a membrane covering. Gastroschisis and Meckel’s Diverticulum are separate congenital anomalies with different pathophysiological mechanisms.

Question 40:
Answer: A) Gastroschisis involves a herniation of bowel loops through a para-umbilical defect with no surrounding membrane, whereas omphalocele involves herniated intestines (and sometimes other organs) covered by the peritoneal membrane and amnion.
Explanation: Gastroschisis is a congenital abdominal wall defect where the intestines herniate through a small opening to the right of the umbilicus and are not covered by any membrane. Omphalocele, on the other hand, is a condition where the intestines, and sometimes other organs such as the liver, are contained within a sac formed by the peritoneal membrane and amnion. The key difference lies in the presence or absence of a membrane covering the herniated organs. Omphalocele occurs due failure of the gastrointestinal organs to return back into the abdominal cavity following their herniation through the umbilicus.
Option B is incorrect because the location of the defect in omphalocele is usually central or midline in the umbilicus, not specifically to the right of the umbilicus, while gastroschisis is always located to the right of the umbilicus.
Option C is incorrect because omphalocele is often associated with chromosomal anomalies or genetic syndromes, rather than being solely caused by compromised vasculature. Gastroschisis, however, occurs due to a failure in the closure of the abdominal wall during foetal development, often unrelated to genetic factors.
Option D is incorrect because the intestines in omphalocele are not free-floating; they are enclosed within a sac formed by the peritoneal membrane and amnion. In contrast, in gastroschisis, the intestines are not enclosed by a sac and are exposed outside the abdominal wall.
Option E is incorrect because both gastroschisis and omphalocele involve defects in the abdominal wall, but gastroschisis occurs through a para-umbilical defect, not through the umbilical cord itself. Omphalocele, as mentioned, involves a midline defect, and the herniated organs are covered by a membrane.
Question 41:
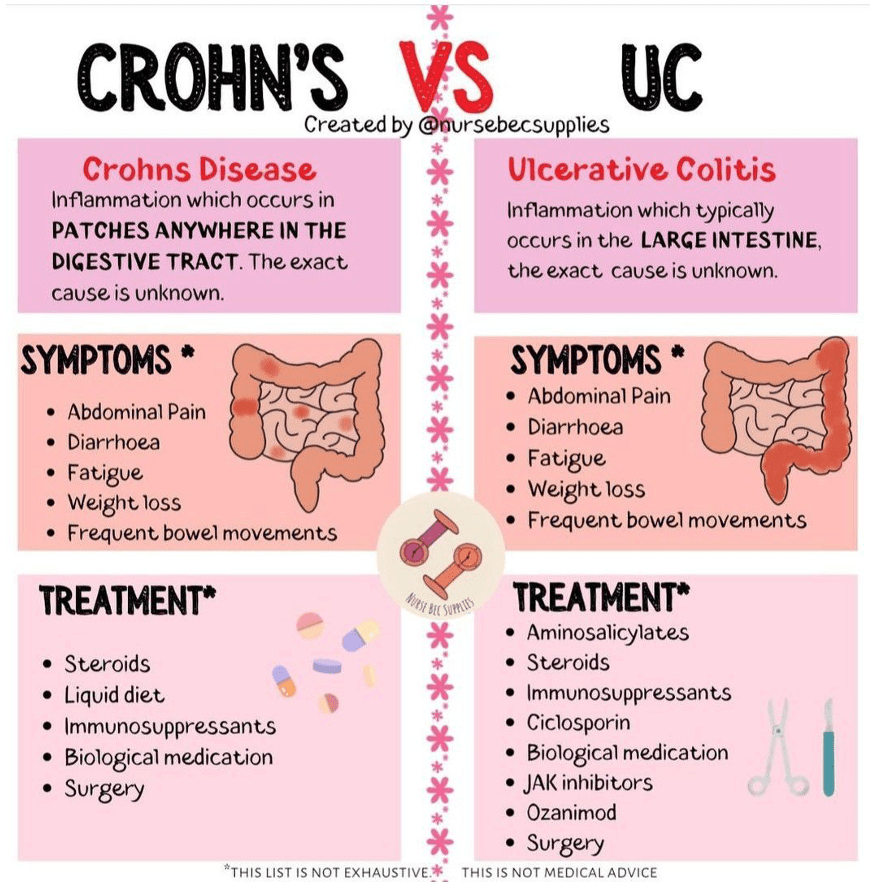
Answer: D) In Crohn’s Disease, strictures and fistulas are common due to transmural inflammation, while in Ulcerative Colitis, superficial inflammation leads to blood in the stool, urgency, and tenesmus, but strictures and fistulas are rare.
Explanation: Crohn’s disease is characterised by transmural inflammation, which affects all layers of the intestinal wall, leading to complications such as strictures (narrowing of the bowel) and fistulas (abnormal connections between bowel segments or to other organs). Ulcerative colitis, on the other hand, involves only superficial inflammation of the mucosa and submucosa, typically limited to the colon. While it causes symptoms such as blood in the stool, urgency, and tenesmus, fistulas and strictures are rare in ulcerative colitis.
Option A is incorrect because Crohn’s disease affects any part of the GI tract, not just the sigmoid colon, and involves transmural inflammation, whereas ulcerative colitis is confined to the colon and involves only superficial inflammation.
Option B is incorrect because Crohn’s disease tends to have a relapsing-remitting course with intermittent flare-ups rather than a singular phase of severe activity. Ulcerative colitis typically presents with continuous inflammation that begins in the rectum and can extend proximally.
Option C is incorrect because while surgery is often curative for ulcerative colitis (due to the possibility of colectomy), it is not curative for Crohn’s disease. Crohn’s disease tends to relapse after surgery due to its transmural and segmental nature, affecting multiple areas of the GI tract.
Option E is incorrect because ulcerative colitis is less likely to be associated with fistula formation and weight loss than Crohn’s disease. Crohn’s disease is more commonly associated with weight loss and fistula formation due to its more severe and widespread involvement of the GI tract.
Question 42:
Answer: C) Neurological damage from pudendal nerve trauma during childbirth, leading to anal sphincter weakness and decreased rectal sensation.
Explanation: The patient’s faecal incontinence, in combination with a history of forceps delivery and perineal numbness, strongly suggests neurological damage to the pudendal nerve, which controls the anal sphincter and rectal sensation. Damage to this nerve during childbirth can lead to anal sphincter weakness, reduced ability to control defecation, and diminished rectal sensation, resulting in incontinence.
Option A is incorrect because overflow incontinence is typically associated with faecal retention and gradual leakage due to incomplete rectal emptying, often linked to conditions like chronic constipation or rectal hypomotility, but it does not typically explain the symptoms of urgency and awareness of the need to defecate.
Option B is incorrect because chronic proctitis and decreased rectal compliance would more likely result in symptoms of urgency and the inability to store stool, but this is not consistent with the patient’s history of childbirth trauma or perineal numbness.
Option D is incorrect because passive incontinence from diabetes would typically involve complete loss of rectal sensation, leading to involuntary stool loss without awareness, but this patient’s symptoms indicate awareness of the need to defecate, which suggests some level of sensation is intact & that her incontinence is active.
Option E is incorrect because idiopathic incontinence with an undiagnosed sacral nerve injury does not fit the clinical history of childbirth trauma and perineal numbness, which point more directly to pudendal nerve damage.
Question 43:
Answer: E) Rapid gastric emptying causing an osmotic load that leads to fluid shifts into the small bowel.
Explanation: This patient’s symptoms, including nausea, fullness, abdominal cramping, diarrhoea, light-headedness, and rapid heart rate after eating, are consistent with dumping syndrome, which often occurs after partial gastrectomy and jejunal reconstruction. Dumping syndrome results from rapid gastric emptying, where undigested food moves too quickly into the small intestine. This causes an osmotic load that draws fluid into the small bowel, leading to the symptoms of cramping, diarrhoea, and dizziness. The rapid gastric emptying also triggers the release of insulin, which can cause hypoglycaemia after meals.
Option A is incorrect because while excessive insulin secretion can cause hypoglycaemia, the full constellation of symptoms in this case, particularly the abdominal cramping and diarrhoea, points more to dumping syndrome rather than insulin-related hypoglycaemia alone.
Option B is incorrect because increased gastric acid secretion typically causes symptoms such as heartburn, epigastric pain, or gastric irritation, which are not prominent in this patient’s presentation. Dumping syndrome is more likely given her surgical history.
Option C is incorrect because small bowel bacterial overgrowth (SIBO) usually causes symptoms like bloating, malabsorption, and weight loss, but it does not explain the postprandial dizziness, rapid heart rate, and cramping associated with this patient’s symptoms.
Option D is incorrect because pancreatic insufficiency would lead to symptoms related to fat malabsorption (steatorrhea), which is not a feature of this patient’s presentation. The primary issue here is rapid gastric emptying after surgery, not pancreatic enzyme deficiency.

Question 44:
Answer: B) Increased permeability of the colon allowing luminal antigens to promote inflammation, impairing sodium and chloride absorption.
Explanation: This patient’s symptoms and biopsy findings are consistent with microscopic colitis, a condition that causes chronic watery diarrhoea with normal colonoscopy results. Microscopic colitis is characterised by histological inflammation in the absence of gross abnormalities on endoscopy. The most common forms are lymphocytic colitis and collagenous colitis, where there is inflammation and increased permeability of the colon, leading to impaired absorption of electrolytes like sodium and chloride, resulting in watery diarrhoea. NSAID use, such as ibuprofen, has been associated with the development of microscopic colitis, which is consistent with this patient’s medical history.
Option A is incorrect because increased gastric acid secretion typically leads to symptoms like heartburn or ulceration, not chronic watery diarrhoea, and there is no indication of acid-related malabsorption in this case.
Option C is incorrect because chronic use of proton pump inhibitors leading to small bowel bacterial overgrowth (SIBO) might cause diarrhoea, but there is no mention of PPI use in this patient, and her biopsy findings do not suggest SIBO.
Option D is incorrect because autoimmune-mediated destruction of the enteric nervous system typically causes motility issues, not the inflammation and impaired absorption characteristic of microscopic colitis.
Option E is incorrect because impaired absorption of bile acids is typically associated with osmotic diarrhoea, which is not the predominant issue in microscopic colitis. The diarrhoea here is more likely due to inflammation and increased permeability in the colon.
Question 45:
Answer: B) Bacillus cereus
Explanation: This patient’s symptoms, including the rapid onset of abdominal pain, vomiting, and watery diarrhoea following the consumption of food, are most consistent with food poisoning caused by Bacillus cereus. This bacterium can produce two types of toxins: an emetic toxin (causing vomiting) and a diarrhoeal toxin (causing watery diarrhoea). The onset of symptoms within a few hours after eating, especially after a buffet meal, suggests foodborne intoxication, which is characteristic of Bacillus cereus.
Option A is incorrect because Vibrio cholerae causes profuse watery diarrhoea and is usually associated with cholera outbreaks, often linked to contaminated water, and typically causes more severe dehydration and a longer incubation period.
Option C is incorrect because Yersinia enterocolitica typically causes a more gradual onset of symptoms and is often associated with contaminated pork or unpasteurised milk. It can cause abdominal pain that mimics appendicitis but does not typically cause the rapid onset of symptoms seen in this case.
Option D is incorrect because Campylobacter jejuni usually causes a slower onset of diarrhoea, often accompanied by fever, and is typically associated with undercooked poultry or contaminated water. It also typically causes bloody diarrhoea rather than the watery diarrhoea described here.
Option E is incorrect because Salmonella (non-typhoidal) generally causes diarrhoea, fever, and abdominal cramps, with symptoms developing over a longer incubation period, typically 6–72 hours after exposure. This patient’s rapid onset of symptoms makes Salmonella less likely in this case.
Question 46:
Answer: B) Escherichia coli O157:H7
Explanation: This patient’s presentation of crampy abdominal pain, fever, and bloody diarrhoea following the consumption of undercooked chicken and raw vegetables is highly suggestive of an infection with Escherichia coli O157:H7. This strain of E. coli produces a potent shiga-like toxin and can cause bloody diarrhoea, often with a risk of developing haemolytic uremic syndrome (HUS), especially in young children and the elderly.
Option A is incorrect because Shigella dysenteriae typically causes bloody diarrhoea, fever, and abdominal cramps, but it is more often associated with human-to-human transmission through faecal-oral routes, especially in crowded environments. It does not have the same link to undercooked poultry as E. coli O157:H7.
Option C is incorrect because Clostridium difficile is more commonly associated with recent antibiotic use and presents with watery diarrhoea, abdominal cramping, and sometimes pseudomembranous colitis. It is not typically linked to undercooked food or raw vegetables.
Option D is incorrect because Listeria monocytogenes is usually associated with soft cheeses, deli meats, and unpasteurised dairy products, not undercooked poultry. It can cause gastrointestinal symptoms but is more often seen in pregnant women, the elderly, and immunocompromised patients.
Option E is incorrect because Giardia lamblia usually causes prolonged, non-bloody diarrhoea with greasy stools and is more commonly contracted from contaminated water sources rather than undercooked food or raw vegetables.
Question 47:
Answer: A) The child is more likely to experience severe dehydration and a longer duration of diarrhoea, while the elderly patient is more likely to have a sudden onset of vomiting and diarrhoea that lasts for a shorter period.
Explanation: In the child, rotavirus is a leading cause of severe gastroenteritis, particularly in unvaccinated children, and is associated with profuse watery diarrhoea, significant dehydration, and a longer illness duration. By contrast, in the elderly patient, norovirus is a common cause of gastroenteritis in nursing home settings and is characterised by abrupt onset of vomiting and diarrhoea, usually resolving within 24 to 48 hours, although complications like dehydration can occur.
Option B is incorrect because the child is more prone to severe dehydration and prolonged symptoms, whereas the elderly patient typically has a shorter duration of illness with norovirus.
Option C is incorrect because symptoms differ significantly between the two age groups; children often have more prolonged and severe diarrhoea due to rotavirus, whereas norovirus in the elderly tends to be shorter in duration.
Option D is incorrect because both vomiting and diarrhoea can be severe in rotavirus for the child, and norovirus in the elderly typically resolves quicker.
Option E is incorrect because the elderly patient’s symptoms with norovirus usually improve within a few days, while the child’s symptoms with rotavirus tend to be more severe and prolonged without vaccination.
Question 48:
Answer: C) Villous adenomas confer the highest malignant potential, especially when larger than 2 cm.
Explanation: Among colonic polyps, the degree of malignancy risk is influenced by both histological type and size. Villous adenomas are known to have the highest malignant potential compared to tubular and tubulo-villous adenomas, particularly when larger than 2 cm. Tubulo-villous adenomas carry an intermediate risk of malignancy, while tubular adenomas have the lowest risk of progression to colorectal cancer.
Option A is incorrect because tubular adenomas have a lower malignant potential compared to villous or tubulo-villous adenomas.
Option B is incorrect because tubulo-villous adenomas have moderate malignant potential and are not negligible in comparison.
Option D is incorrect because histological type is also a key determinant of malignant potential, not just size.
Option E is incorrect because tubulo-villous adenomas have intermediate risk, not the highest risk, which is associated with villous adenomas.
Question 49:
Answer: D) FAP is caused by mutations in the APC tumour suppressor gene, while Lynch Syndrome involves mutations in DNA mismatch repair genes such as MLH1 and MSH2.
Explanation: Familial Adenomatous Polyposis (FAP) is an autosomal dominant condition caused by mutations in the APC gene, leading to the development of hundreds to thousands of adenomatous polyps and a nearly 100% lifetime risk of colorectal cancer if left untreated. Lynch Syndrome, also known as hereditary non-polyposis colorectal cancer (HNPCC), is caused by germline mutations in DNA mismatch repair (MMR) genes such as MLH1, MSH2, MSH6, or PMS2. It is associated with microsatellite instability and an increased risk of colorectal and extra-colonic cancers, particularly endometrial cancer.
Option A is incorrect because only Lynch Syndrome involves mutations in DNA mismatch repair genes and microsatellite instability.
Option B is incorrect because Lynch Syndrome, not FAP, is more commonly associated with extra-colonic cancers like endometrial and ovarian cancer.
Option C is incorrect because Lynch Syndrome is not caused by APC mutations, nor does it present with numerous polyps.
Option E is incorrect because FAP involves extensive polyposis, while Lynch Syndrome typically does not present with polyposis, but its cancer risk is significant for multiple organ systems.
Question 50:
Answer: D) Encapsulation and lack of invasion in the surrounding tissue
Explanation: The presence of encapsulation and the absence of invasion into surrounding tissue are key features that distinguish benign tumours from malignant ones. Benign tumours are typically well-circumscribed and encapsulated, which prevents them from spreading to adjacent tissues. Malignant tumours, on the other hand, tend to invade local structures and lack clear boundaries.
Option A is incorrect because pleomorphism, while more commonly associated with malignancy, can also be seen in benign tumours. Therefore, it does not reliably distinguish benign from malignant tumours.
Option B is incorrect because a homogenous cut-surface can be seen in both benign and malignant tumours, and it does not specifically indicate benignity.
Option C is incorrect because a high mitotic index is indicative of malignancy, suggesting rapid cell division, which is uncommon in benign tumours.
Option E is incorrect because an increased cytoplasmic-to-nuclear ratio is typically seen in malignant tumours, where the nuclei are often enlarged relative to the cytoplasm, a hallmark of malignancy.
Question 51:
Answer: C) A diffuse infiltration of poorly cohesive cancer cells with a poor prognosis
Explanation: This patient’s condition is consistent with diffuse gastric cancer, characterised by poorly cohesive malignant cells, including signet-ring cells, which are indicative of a more aggressive and poorly differentiated tumour. This type of gastric cancer tends to have a poor prognosis due to its diffuse infiltration of the stomach wall, which leads to thickening and a leather-bottle appearance (desmoplastic reaction).
Option A is incorrect because a well-localised carcinoma, typically associated with intestinal-type gastric cancer, would have a better prognosis than the diffuse form described here.
Option B is incorrect because glandular dysplasia without evidence of malignant invasion is not consistent with the findings of a poorly cohesive adenocarcinoma with invasion.
Option D is incorrect because intestinal metaplasia refers to a condition that may predispose to gastric cancer but does not have significant clinical consequences by itself. It is not the same as the invasive cancer described in this case.
Option E is incorrect because a solitary polyp-like lesion confined to the mucosal layer is more indicative of an early-stage gastric cancer, not the diffuse, invasive form that is described here.


Question 52:
Answer: C) G-cells in the antrum producing excessive gastrin in response to low stomach acid levels
Explanation: This patient’s symptoms, including recurrent peptic ulcers that do not respond to proton pump inhibitors and elevated gastrin levels, are indicative of Zollinger-Ellison syndrome. This condition is caused by a gastrin-secreting neuroendocrine tumour, typically located in the pancreas or duodenum, that leads to excessive gastrin production. Gastrin stimulates the parietal cells in the stomach to produce acid, which causes the formation of multiple ulcers. The excess gastrin production is often a compensatory response to low stomach acid levels.
Option A is incorrect because a mutation in the APC gene is associated with familial adenomatous polyposis, which primarily affects the colon, not the stomach.
Option B is incorrect because chronic inflammation of the gastric mucosa may cause ulcers, but it does not explain the elevated gastrin levels seen in this patient. The overproduction of acid is due to a gastrin-secreting tumour (neuroendocrine tumour), not chronic inflammation.
Option D is incorrect because the destruction of parietal cells leads to decreased gastric acid production, which would not explain the elevated gastrin levels in this patient. This is more characteristic of conditions such as autoimmune gastritis.
Option E is incorrect because mesenchymal tumours typically involve stromal cells and are not associated with excessive gastrin production. This description is more typical of gastrointestinal stromal tumours (GISTs), which are not the cause in this patient.
Question 53:
Answer: B) Acute pancreatitis due to alcohol consumption, leading to the activation of pancreatic enzymes
Explanation: This patient’s presentation of severe upper abdominal pain radiating to the back, nausea, vomiting, and elevated serum amylase and lipase levels is characteristic of acute pancreatitis. Given the history of heavy alcohol consumption, the most likely cause is alcohol-induced pancreatitis. Alcohol causes premature activation of pancreatic enzymes, such as trypsin, within the pancreas itself, leading to pancreatic inflammation and damage.
Option A is incorrect because although gallstones are the most common cause of acute pancreatitis, they typically cause obstruction of the common bile duct, leading to retrograde flow of bile into the pancreas. However, the patient’s history of alcohol use and lack of biliary obstruction on imaging makes gallstones less likely in this case.
Option C is incorrect because chronic pancreatitis is a long-term condition caused by repeated episodes of inflammation and damage to the pancreas, often due to alcohol use. This patient’s acute symptoms and elevated enzyme levels suggest an acute episode rather than chronic pancreatitis.
Option D is incorrect because pancreatic carcinoma usually presents with more chronic, insidious symptoms such as weight loss, jaundice, and fatigue. The patient’s acute symptoms and the lack of significant findings on imaging make pancreatic cancer unlikely in this case.
Option E is incorrect because acute cholecystitis, an inflammation of the gallbladder, typically causes right upper quadrant pain, fever, and leucocytosis. Although it can lead to bile duct obstruction and secondary pancreatitis, this patient’s symptoms and history are more consistent with acute pancreatitis directly caused by alcohol consumption.
Question 54:
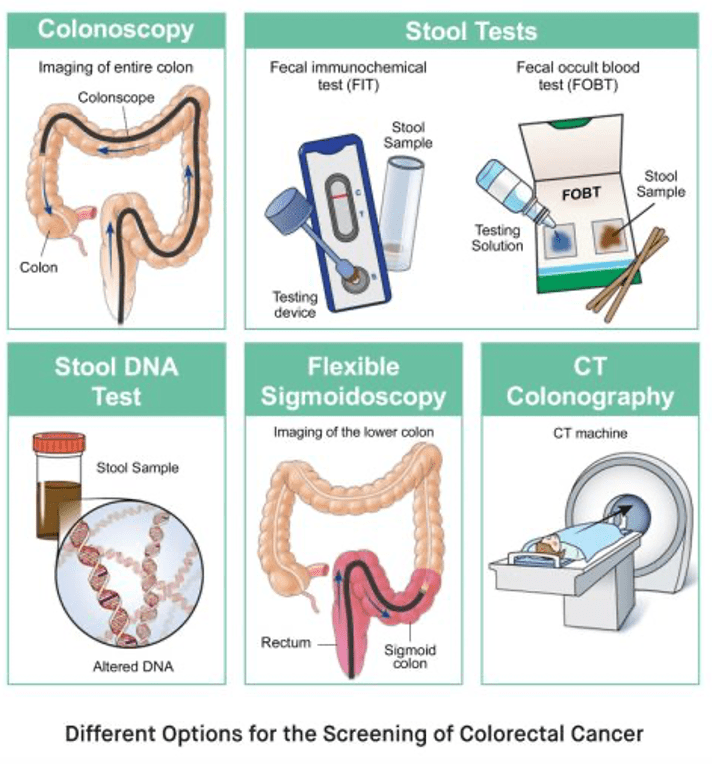
Answer: B) The current stool sample test (FOB) has poor specificity so is being replaced by a test that detects FIT blood
Explanation: The faecal occult blood (FOB) test is used in colorectal cancer (CRC) screening to detect hidden blood in stool, which may indicate the presence of colorectal cancer or advanced adenomas. However, the FOB test has relatively poor specificity, meaning it can produce false positives, where blood may be detected in the stool without an underlying malignancy. To improve this, the faecal immunochemical test (FIT) is being adopted in place of the FOB test. The FIT test detects human haemoglobin specifically and has higher specificity for detecting CRC, with fewer false positives compared to FOB.
Option A is incorrect because while the FOB test is widely used, it is not highly specific but quite sensitive (low false negatives). It can lead to false positive results due to other conditions, such as haemorrhoids or gastrointestinal bleeding unrelated to cancer.
Option C is incorrect because flexible sigmoidoscopy is part of the Bowel Scope programme, which targets individuals aged 55 to 64. It is used to examine the lower part of the colon to identify abnormalities that may indicate cancer or precancerous lesions.
Option D is incorrect because the FIT test has a higher sensitivity and specificity than the FOB test, not a reduced sensitivity. FIT is more specific for detecting blood from the lower gastrointestinal tract, leading to fewer false positives.
Option E is incorrect because the Bowel Scope programme uses flexible sigmoidoscopy for individuals aged 55 to 64, whereas stool tests such as FOB or FIT are used in the broader screening programme for those aged 60 to 74. The interval for screening using these tests is typically every 2 years in the UK.
Question 55:
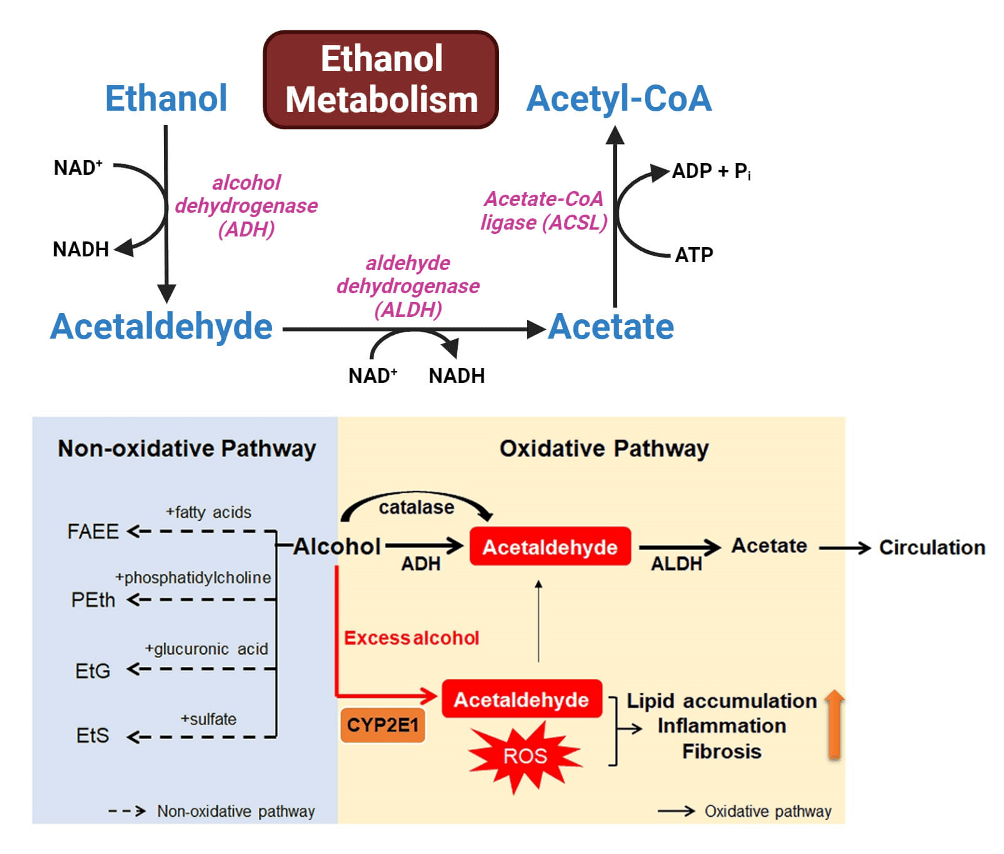
Answer: B) Induction of the microsomal ethanol oxidising system (MEOS) by chronic alcohol use
Explanation: In patients with chronic alcohol consumption, the liver adapts to increased alcohol intake by inducing the microsomal ethanol oxidising system (MEOS), which consists of cytochrome P450 enzymes, particularly CYP2E1. This system is responsible for metabolising alcohol at higher rates than the alcohol dehydrogenase (ADH) pathway, especially when blood alcohol levels are elevated. Over time, chronic alcohol consumption leads to the increased activity of MEOS, allowing for faster metabolism of ethanol.
Option A is incorrect because while Alcohol Dehydrogenase (ADH) and Acetaldehyde Dehydrogenase (ALDH) are involved in alcohol metabolism, their activities do not significantly increase due to chronic alcohol use. The MEOS system plays a more prominent role in this context.
Option C is incorrect because decreased NADH production would not lead to faster alcohol metabolism. In fact, chronic alcohol use increases NADH levels, which can impair the functioning of other metabolic processes, including oxidative phosphorylation.
Option D is incorrect because chronic alcohol consumption actually increases the activity of Cytochrome P450IIE1 (part of MEOS), not reduces it. The increased activity of this enzyme contributes to the faster metabolism of alcohol in chronic drinkers.
Option E is incorrect because high blood acetate levels are a by-product of alcohol metabolism, and they do not inhibit alcohol metabolism. In fact, acetate is further metabolised and used as an energy source in various tissues.
Question 56:
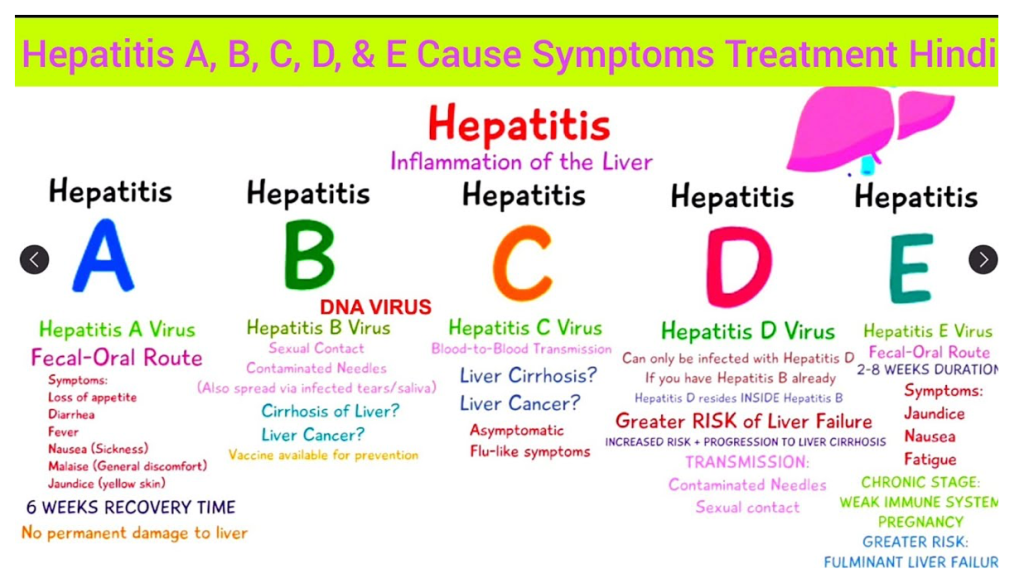
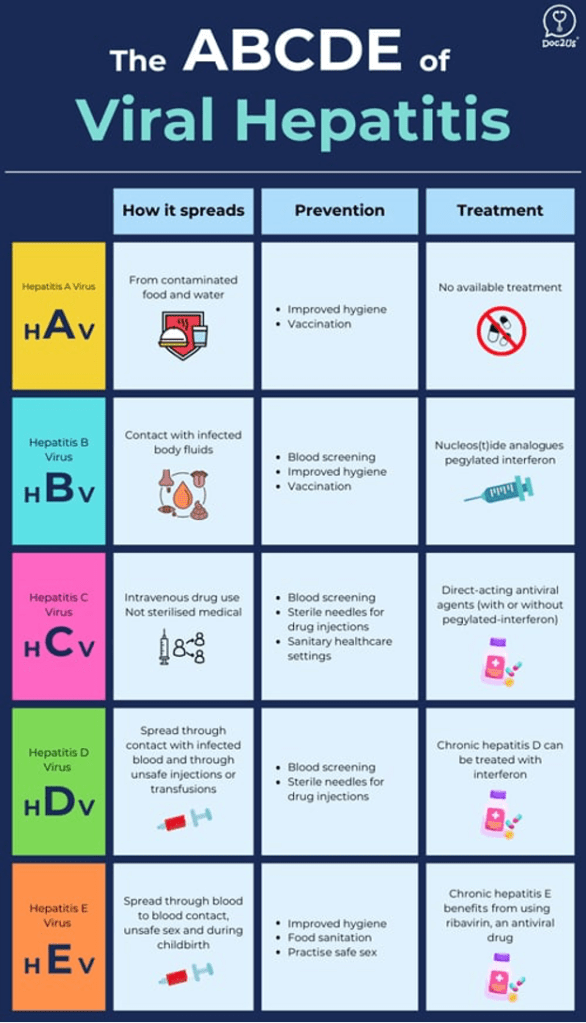
Answer: B) The most likely infection is Hepatitis C, which can lead to a chronic infection in 80% of cases, with a risk of cirrhosis and hepatocellular carcinoma over time.
Explanation: Hepatitis C virus (HCV) is most commonly transmitted through blood-to-blood contact, such as through intravenous drug use. Infected individuals may experience an acute phase with symptoms like jaundice, fatigue, and upper abdominal discomfort, as seen in this patient. Approximately 80% of acute HCV infections progress to chronic infection, which can lead to long-term complications, including cirrhosis and hepatocellular carcinoma. The patient’s history of intravenous drug use and travel to Southeast Asia also raises suspicion for HCV, as it is endemic in these regions.
Option A is incorrect because while Hepatitis B is a potential cause of viral hepatitis, it is less likely in this patient without a known risk factor for HBV, such as sexual contact with an infected person or perinatal exposure. Hepatitis B can lead to chronic infection and liver disease, but it is less common in individuals without these risk factors.
Option C is incorrect because Hepatitis E typically occurs in regions with poor sanitation and is more common in travellers from endemic areas. While it is generally self-limiting and resolves without long-term complications in immunocompetent individuals, it is less likely in this patient based on the history provided.
Option D is incorrect because Hepatitis D only occurs in individuals already infected with Hepatitis B, as it requires the Hepatitis B virus for co-infection. The patient does not have a known history of Hepatitis B, making this less likely.
Option E is incorrect because Hepatitis A typically presents with a self-limiting infection, and while alcohol should be avoided during recovery to prevent further liver damage, the patient’s risk factors point more toward Hepatitis C. Hepatitis A is transmitted through the faecal-oral route, and the patient’s history does not suggest this mode of transmission.
Question 57:
Answer: E) Stage 4 – Decompensated cirrhosis with first non-bleeding decompensation
Explanation: This patient is showing signs of decompensated cirrhosis, including jaundice, weight loss, abdominal distension (likely due to ascites), and elevated liver enzymes. His clinical presentation with ascites and liver dysfunction (low albumin, elevated bilirubin) suggests that the liver is no longer able to maintain normal function, a characteristic of decompensated cirrhosis. Stage 4 cirrhosis is characterised by decompensation without bleeding complications, and ascites is often one of the first manifestations of decompensation.
Option A is incorrect because Stage 0 typically refers to no significant liver damage or portal hypertension, which does not apply in this patient given the clinical and laboratory evidence of cirrhosis.
Option B is incorrect because Stage 1 cirrhosis refers to compensated cirrhosis without significant clinical signs of decompensation. This patient is already showing signs of decompensation such as ascites and jaundice.
Option C is incorrect because Stage 2 would involve compensated cirrhosis with varices, but the patient’s presentation is more consistent with decompensated cirrhosis, which is beyond Stage 2.
Option D is incorrect because Stage 3 refers to decompensated cirrhosis with complications like bleeding, but this patient does not present with active bleeding symptoms, which would be a hallmark of Stage 3.
Option E is the correct answer because it fits with the patient’s presentation of decompensated cirrhosis with ascites as the first non-bleeding complication.

Question 58:
Answer: E) Reduced sodium levels (hyponatremia)
Explanation: This patient’s presentation, including chronic alcohol use, jaundice, ascites, and splenomegaly, suggests liver cirrhosis with complications such as portal hypertension and fluid retention. A common complication of cirrhosis is the development of hyponatremia, which results from impaired renal function and fluid retention due to portal hypertension and activation of hormonal systems (RAAS and ADH). This results in dilution of sodium in the body.
Option A is incorrect because while renal function may be normal early in cirrhosis, the development of ascites and splenomegaly is suggestive of advanced liver disease, and renal dysfunction, including hepatorenal syndrome, can occur in decompensated cirrhosis.
Option B is incorrect because hypoxemia and arterial oxygen desaturation are not typically associated with cirrhosis unless there are additional pulmonary complications (e.g., hepatopulmonary syndrome), which are not suggested in this case.
Option C is incorrect because in cirrhosis, platelet count is usually decreased due to splenomegaly (which causes sequestration of platelets) and impaired platelet production in the bone marrow due to liver dysfunction.
Option D is incorrect because elevated alkaline phosphatase (ALP) is more commonly seen in cholestatic liver diseases (e.g., primary biliary cholangitis, biliary obstruction), but it is not a typical finding in cirrhosis, where other liver enzymes (e.g., AST, ALT) are more likely to be elevated.
Option E is the correct answer because hyponatremia is a common finding in patients with advanced cirrhosis, particularly those with ascites, due to water retention and dilutional effects.
Question 59:
Answer: A) Mirizzi Syndrome
Explanation: Mirizzi syndrome occurs when a large gallstone becomes impacted in the cystic duct or neck of the gallbladder, causing extrinsic compression of the common bile duct, which leads to obstructive jaundice and cholangitis. In some cases, as in this patient, the stone can erode through the gallbladder wall into the common bile duct, causing the symptoms of biliary obstruction.
Option B is incorrect because gallbladder carcinoma typically presents with symptoms like weight loss, nausea, and vomiting, and is less likely to cause the acute biliary obstruction seen in this patient. Gallbladder carcinoma is also not typically associated with the presence of large stones eroding into the bile duct.
Option C is incorrect because choledochal cysts are congenital dilations of the biliary tree, which present with biliary obstruction and jaundice, but they do not involve a gallstone eroding through the gallbladder wall into the bile duct, as seen in this case.
Option D is incorrect because while pancreatitis can cause abdominal pain and jaundice, it is not typically associated with a stone eroding through the gallbladder wall into the common bile duct. Pancreatitis is usually caused by gallstones or alcohol use, but it does not specifically match the described scenario. Furthermore, pancreatitis causes epigastric pain that radiates to the back rather than right upper quadrant pain.
Option E is incorrect because gallstone ileus occurs when a large gallstone passes into the intestines through a fistula, causing a mechanical obstruction. This condition does not cause obstructive jaundice or cholangitis, as seen in this patient.
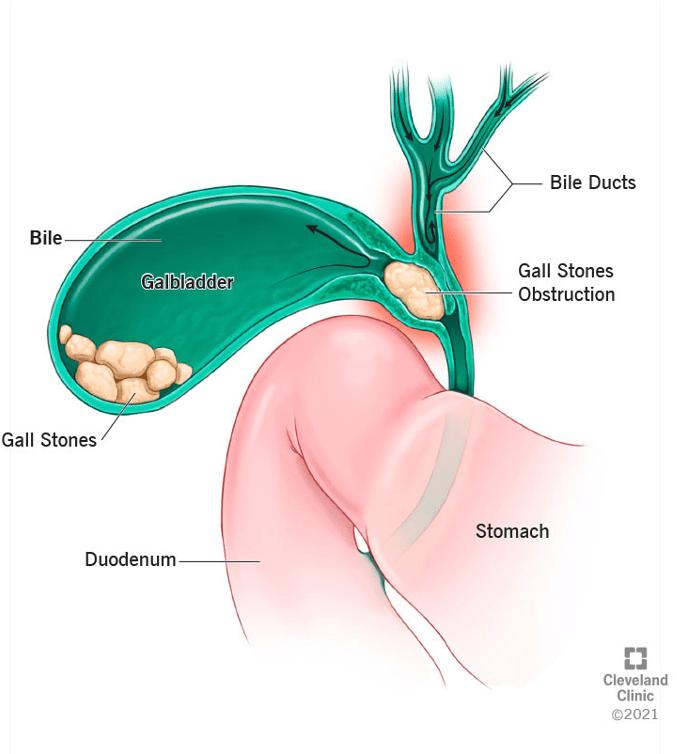
Question 60:
Answer: B) Endoscopic Retrograde Cholangio-pancreatography (ERCP) to directly visualise the biliary tree and obtain biopsies if necessary.
Explanation: The patient’s presentation with jaundice, dark urine, and a palpable right upper quadrant mass, along with raised conjugated bilirubin and alkaline phosphatase (ALP), suggests a biliary obstruction. Ultrasound revealing biliary duct dilation without visible stones raises concern for a malignancy or other obstruction not detected on ultrasound, such as cholangiocarcinoma or pancreatic cancer. ERCP allows direct visualisation of the biliary tree and can be used to obtain biopsies for histological confirmation, as well as facilitate therapeutic intervention, such as stent placement if needed.
Option A is incorrect because a CT scan can help evaluate for liver metastases and structural abnormalities but would not be the next step in the investigation when a biliary obstruction is suspected, as ERCP would provide more detailed diagnostic and therapeutic options for the biliary tree.
Option C is incorrect because MRI can be useful for assessing liver lesions, but ERCP provides a more direct assessment of the biliary duct system. MRI may be an adjunct, but ERCP is preferred for suspected biliary obstruction.
Option D is incorrect because while endoscopic ultrasound is useful for evaluating biliary strictures, ERCP is typically the preferred procedure for both diagnosis and potential therapeutic intervention in this scenario, as it allows for direct visualisation and biopsy.
Option E is incorrect because a liver biopsy is not appropriate at this stage. The patient’s presentation suggests a biliary obstruction rather than primary liver disease such as cirrhosis or fibrosis. The primary focus should be on evaluating the biliary tree for potential malignancy or obstruction.
