
Gastrointestinal
Question 1:
Answer: c) Small intestine – absorption of nutrients through segmentation
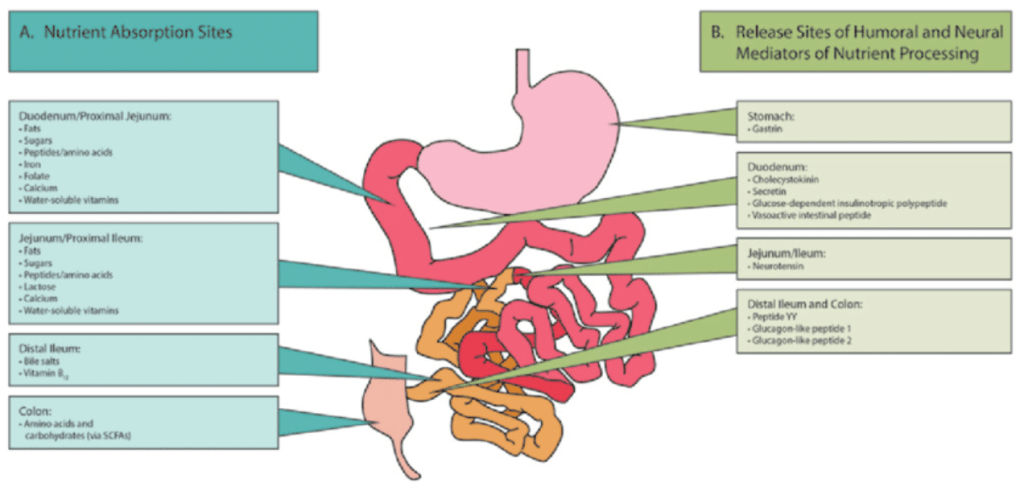
Explanation: The small intestine is primarily responsible for the absorption of nutrients, including carbohydrates, proteins, lipids, iron, and calcium. It is where most of the digestion and nutrient absorption occurs.
A is incorrect since the mouth initially digests starch by salivary amylase.
B is incorrect since lipids are not digested in the stomach, they are digested in the small intestine and pepsin is responsible for digesting proteins.
D is incorrect as carbohydrate digestion begins in the mouth.
E is incorrect as above the bolus it is the circular muscle that contracts and longitudinal muscle which relaxes.
Question 2:
Answer: b) It involves signalling molecules acting on neighbouring cells.
Explanation: Paracrine control in the GI tract involves signalling molecules (paracrine factors) that act on nearby cells to regulate various functions. An example is histamine acting on parietal cells to release HCl and on chief cells to release pepsinogen.
A is incorrect although the GRP acting on ECL cells to release histamine is correct as it is paracrine, the rest of the answer is describing endocrine signalling.
C is incorrect as it involves the autonomic and enteric nervous system which are involuntary.
Question 3:
Answer: b) Fundus and body of the stomach
Explanation: Receptive relaxation is a function of the fundus and body of the stomach, allowing it to accommodate ingested food.
A is incorrect as the pyloric sphincter regulates food passage into the duodenum.
C is incorrect as the lower oesophageal sphincter is responsible for preventing acid reflux.
D is incorrect as the antrum is responsible for retropulsion and mechanical digestion of the food, whilst the pylorus is responsible for regulating the passage of chyme into the duodenum.
E is incorrect as both the cecum and ascending colon are part of the large intestine not the stomach.
Question 4:
Answer: e) It involves squirting chyme back into the stomach from the antrum.
Explanation: Retropulsion in the stomach is the process by which chyme, the partially digested food, is periodically squirted back into the stomach from the antrum. This allows for further mixing and churning with gastric juices to aid in digestion.
A is incorrect as this is describing the function of the antrum, the fundus is responsible for receptive relaxation and a reservoir for food before it is released into the stomach for further digestion.
B is incorrect as retropulsion refers to a process in the stomach not in the rectum.
C is incorrect as it describes the function of forward propulsion into the duodenum, not retropulsion.
D describes the function of the LOS which is correct but has nothing to do with retropulsion, so it is incorrect.
Question 5:
Answer: a) Parietal cells produce HCl via the proton pump mechanism.
Explanation: In gastric secretion, parietal cells are responsible for producing gastric acid (HCl) in the stomach. They achieve this through the proton pump mechanism, which involves actively transporting hydrogen ions (protons) from the cytoplasm into the stomach’s lumen. This transport process requires the presence of the H+/K+ ATPase enzyme, known as the proton pump. This mechanism generates a highly acidic environment in the stomach, crucial for digesting food by activating pepsinogen into pepsin and providing a defence against pathogens.
B is incorrect as chief cells produce pepsinogen which is then converted into pepsin due to HCl and intrinsic factor is produced by parietal cells not chief cells, although they are in the fundus and body.
C is incorrect as although G cells are enteroendocrine cells and are found in the antrum, they produce gastrin not histamine which is produced by ECL cells.
D is incorrect as they are in the antrum and produce somatostatin which inhibits the release of HCl.
Question 6:
Answer: c) The cephalic phase is initiated by the sight, smell, taste, or even thought of food.
Explanation: The cephalic phase of gastric secretion is initiated by sensory stimuli related to food, such as the sight, smell, taste, or even thinking about food. These stimuli send signals to the brain, specifically the vagus nerve, which then stimulates gastric secretions. It is a preparatory phase that readies the stomach for food digestion by increasing saliva production, promoting the release of gastrin, and activating the secretion of gastric juices. This phase plays a crucial role in the digestive process, as it anticipates the arrival of food and gets the digestive system ready for the upcoming meal.
A is incorrect since Gastrin release from G cells occurs primarily in the gastric phase of gastric secretion, not the cephalic phase.
B is incorrect as this occurs in the intestinal phase of digestion not cephalic.
D is incorrect as Pepsinogen release occurs in the gastric phase when food reaches the stomach and stimulates chief cells, not in the cephalic phase.
E is incorrect as bile production is unrelated to gastric secretion phases and occurs in the liver and is stored in the gallbladder.
Question 7:
Answer: c) Somatic nervous system via the pudendal nerve
Explanation: The contraction of the external anal sphincter during voluntary defecation is under the control of the somatic nervous system. This conscious control allows us to delay or initiate bowel movements voluntarily, ensuring faecal continence. In contrast, the autonomic nervous system controls involuntary GI functions, such as peristalsis and secretion.
A is incorrect as the sympathetic nervous system primarily controls involuntary actions and does not directly innervate the external anal sphincter for voluntary control.
B is incorrect as the parasympathetic nervous system does not directly control the voluntary contraction of the external anal sphincter and the nerve roots are that of the pudendal nerve.
D is incorrect as the enteric nervous system primarily governs the function of the gastrointestinal tract not the voluntary external anal sphincter.
E is incorrect as the autonomic nervous system includes both sympathetic and parasympathetic components and primarily controls involuntary functions.
Question 8:
Answer: e) Segmentation
Explanation: During fasting, segmentation is the primary motility pattern in the small intestine. Segmentation involves mixing and churning of intestinal contents, aiding in nutrient absorption by bringing them into contact with the absorptive surfaces of the intestinal lining.
A is incorrect as although pendular movement do occur in the small intestine, they primarily serve to mix the contents and not to facilitate nutrient absorption.
B is incorrect as haustrations are characteristic of the large intestine (colon) and are not the small intestine.
C is incorrect as mass movements are powerful, wave-like contractions that occur in the large intestine to move faecal matter toward the rectum not nutrient absorption.
D is incorrect as although peristalsis does occur in the small intestine, it is primarily responsible for moving the chyme along rather than for absorption.
Question 9:
Answer: b) Parietal cells produce intrinsic factor via the release of gastrin.
Explanation: Parietal cells in the stomach produce intrinsic factor, a glycoprotein necessary for vitamin B12 absorption. Gastrin, released in response to food, stimulates the production of intrinsic factor by parietal cells.
A is incorrect as chief cells are responsible for producing pepsinogen, the precursor to pepsin, but they do not produce intrinsic factor.
C is incorrect as G cells produce gastrin, a hormone that stimulates the secretion of gastric acid by parietal cells but do not produce intrinsic factor.
D is incorrect as D cells produce somatostatin, which inhibits the secretion of several other hormones, including gastrin, but they do not produce intrinsic factor.
E is incorrect as mucous cells produce mucus to protect the stomach lining but do not produce intrinsic factor.
Question 10:
Answer: b) Gastric phase
Explanation: The gastric phase of gastric secretion is characterized by the release of gastrin, histamine, and acetylcholine, which stimulate gastric acid secretion in response to the presence of food in the stomach.
A is incorrect as the cephalic phase is triggered by the sight, smell, taste, or thought of food, and involves the release of Ach and Gastrin not histamine.
C is incorrect as the primary hormones involved in this phase include secretin and cholecystokinin (CCK), which generally inhibit gastric secretion to slow down the gastric emptying rate.
D and E are incorrect as these are not phases of gastric secretion.
Question 11:
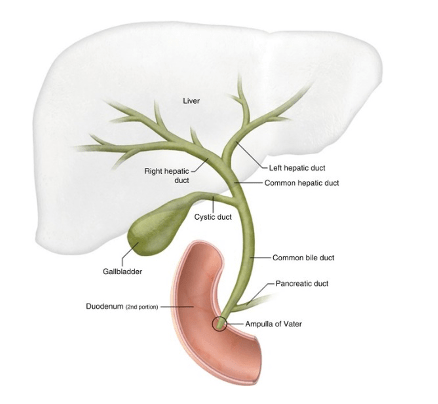
Answer: b) It controls the release of bile and pancreatic juices into the duodenum.
Explanation: The sphincter of Oddi, located in the duodenum, controls the release of bile from the common bile duct and pancreatic juices from the pancreatic duct into the duodenum, where they aid in digestion.
A is incorrect because the sphincter of Oddi does not regulate the entry of food into the stomach. This function is performed by the lower oesophageal sphincter.
C is incorrect as the sphincter of Oddi does not facilitate nutrient absorption. Its role is to control the flow of bile and pancreatic juices into the duodenum to aid in digestion.
D is incorrect as food does not pass through the common bile duct or the pancreatic duct. The sphincter of Oddi regulates bile and pancreatic juice flow into the duodenum.
E is incorrect as the internal and external anal sphincters control the passage of faeces from the rectum.
Question 12:
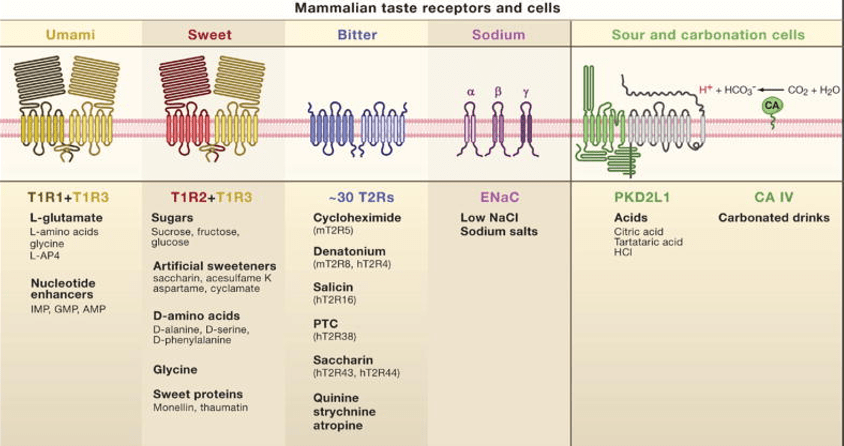
Answer: d) Umami receptors – T1R1 + T1R3
Explanation: Umami, associated with savoury and meaty flavours, is primarily detected by umami receptors. These receptors respond to the amino acid glutamate, commonly found in foods like meat, cheese, and soy sauce.
Question 13:
Answer: d) Microbiota ferment dietary fibre to produce SCFAs, which are absorbed and used for energy.
Explanation: The gut microbiota ferment dietary fibre in the large intestine, producing short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate. These SCFAs are absorbed and used for energy by colonocyte, and they play important roles in gut health.
A is incorrect as while microbiota do play a role in breaking down certain carbohydrates, the primary production and absorption of glucose occur in the small intestine.
B is incorrect as bile salts are produced by the liver and stored in the gallbladder, not by microbiota.
C is incorrect as microbiota do not synthesize these specific vitamins. They can produce certain B vitamins and vitamin K, but not vitamins A, D, and E.
E is incorrect as although microbiota can contribute to protein metabolism to some extent, the primary breakdown of proteins into amino acids occurs in the stomach and small intestine enzymes like pepsin and trypsin.
Question 14:
Answer: e) It provides a protective layer that shields the gastrointestinal lining from acidic and enzymatic damage.
Explanation: The primary function of the mucus-bicarbonate barrier in the gastrointestinal tract is to protect the lining of the stomach and intestines from the corrosive effects of stomach acid and digestive enzymes.
B is incorrect as while mucus does help lubricate the gastrointestinal tract, this is not the primary function of the mucus-bicarbonate barrier. The main function of this barrier is to protect against acid and enzymatic damage.
C is incorrect as the activation of digestive enzymes typically occurs due to other factors such as pH changes not because of the mucus-bicarbonate barrier.
D is incorrect because the conversion of pepsinogen to pepsin is primarily facilitated by the acidic environment of the stomach (hydrochloric acid), not by the mucus-bicarbonate barrier.
Question 15:
Answer: c) It regulates the passage of chyme from the stomach to the duodenum.
Explanation: The pyloric sphincter is a muscular ring that separates the stomach from the duodenum. Its primary function is to regulate the controlled release of chyme (partially digested food) from the stomach into the small intestine (duodenum) for further digestion and absorption.
A is incorrect as the backflow of acid is primarily prevented by the actions of the lower oesophageal sphincter.
B is incorrect as the release of pancreatic juices into the small intestine is controlled by the sphincter of Oddi, not the pyloric sphincter.
D is incorrect as although the pyloric sphincter does regulate food entry into the small intestine, its main role is not directly related to nutrient absorption but rather to control the passage rate of chyme.
E is incorrect because the pyloric sphincter does not secrete digestive enzymes. Digestive enzymes in the stomach are primarily secreted by gastric glands.
Question 16:
Answer: d) Pepsin
Explanation: Pepsin is the enzyme responsible for digesting proteins in the stomach. It is secreted in its inactive form, pepsinogen, by chief cells. Upon activation by the acidic environment in the stomach, it breaks down proteins into smaller peptides.
A is incorrect because intrinsic factor is a glycoprotein produced by the parietal cells of the stomach that is essential for the absorption of vitamin B12 in the small intestine.
B is incorrect because haptocorrin (also known as R-protein or transcobalamin I) is a protein that binds to vitamin B12 in the stomach and protects it from degradation.
C is incorrect because trypsin is an enzyme that digests proteins in the small intestine, not the stomach. It is secreted by the pancreas in the form of trypsinogen and activated in the small intestine by enterokinases (aka enteropeptidases).
E is incorrect because chymotrypsinogen is the inactive precursor of chymotrypsin, an enzyme that digests proteins in the small intestine. It is secreted by the pancreas and activated in the small intestine by trypsin.
Question 17:
Answer: d) It facilitates the absorption of water and electrolytes; forms stool, and the colon bacteria produce SCFAs from dietary fibre.
Explanation: The primary function of the large intestine (colon) is the absorption of water, electrolytes, synthesising SCFA, and some vitamins (K and B) produced by intestinal bacteria. It also plays a role in absorbing remaining nutrients like certain fatty acids.
A is incorrect Vitamin B12 absorption occurs in the terminal ileum, not the colon.
B is incorrect because SCFAs are primarily synthesized by gut bacteria in the colon, not directly by the colon itself although conversion of primary to secondary bile acids occurs in the colon e.g. cholic acid to deoxycholic acid.
C is incorrect because SCFAs are not converted into primary bile acids in the colon.
E is incorrect because vitamin B12 synthesis occurs in the ileum and is not a function of the colon. Additionally, regulation of SCFA production primarily involves gut microbiota in the colon, not the colon itself.
Question 18:
Answer: c) It concentrates and stores bile produced by the liver, releasing it into the small intestine to aid in fat digestion.
Explanation: The gallbladder stores and concentrates bile produced by the liver. When needed, it releases concentrated bile into the small intestine to aid in the digestion and absorption of lipids.
A is incorrect because bile salts are produced by the liver, not by the gallbladder. Their function is to emulsify fats in the small intestine, not to neutralize stomach acid.
B is incorrect as this is the function of bile not the gallbladder.
D is incorrect as cholic and chenodeoxycholic acid are primary bile acids made by the liver and stored in the gallbladder.
E is incorrect because digestive enzymes are primarily produced by the pancreas (lipase) and secreted into the small intestine, not by the gallbladder.
Question 19:
Answer: d) Secretin
Explanation: Secretin is the hormone responsible for stimulating the release of bicarbonate into the small intestine. It is released in response to the acidic chyme entering the duodenum.
A is incorrect because CCK primarily stimulates the release of digestive enzymes from the pancreatic acinar cells and bile from the gallbladder in response to the presence of fats and proteins in the small intestine.
B is incorrect because VIP is involved in various functions including relaxation of smooth muscle in the GI tract and secretion of water and electrolytes, but it does not primarily stimulate bicarbonate release.
C is incorrect because Somatostatin inhibits the release of various hormones including gastrin and insulin, but it is not primarily responsible for stimulating bicarbonate release.
E is incorrect because PP regulates pancreatic and gastrointestinal activities, including enzyme secretion and gallbladder contraction, but it is not primarily responsible for stimulating bicarbonate release.
Question 20:
Answer: d) It governs GI function, including motility and secretion, autonomously, contrasting with the ANS’s regulation of smooth muscle and glandular activity.
Explanation: The Enteric Nervous System (ENS) primarily operates locally within the GI tract, regulating processes like motility and secretion. In contrast, the Autonomic Nervous System (ANS) provides broader control and coordination of various bodily functions, including the GI tract, on a systemic level both involuntarily.
A is incorrect because while the ENS does coordinate peristalsis and regulate blood flow within the GI tract, the ANS also plays a role in regulating blood flow and hormone release, this is not the best answer.
B is incorrect because the release of digestive enzymes and hormones is primarily controlled by the endocrine and exocrine systems, not specifically by the ENS. The ANS does not directly regulate cardiac muscle contraction; that is controlled by the cardiac conduction system.
C is incorrect because while the ENS does manage GI motility and local secretion independently, the ANS is not primarily involved in sensory perception but rather in regulating involuntary actions such as heart rate and digestion.
E is incorrect because while the ENS does play a role in moderating GI blood flow and mucosal immune responses, the ANS does not regulate skeletal muscle contraction directly; that is under voluntary control via the somatic nervous system.
Question 21:
Answer: d) Gastrin release is stimulated by amino acids in the stomach, and it stimulates gastric acid secretion.
Explanation: Gastrin release is primarily stimulated by the presence of amino acids in the stomach. Its main function is to stimulate the secretion of gastric acid (HCl) by parietal cells in the stomach, aiding in protein digestion.
A is incorrect because Gastrin release is stimulated by the presence of peptides and amino acids in the stomach, rather than by low stomach pH and its main function is to stimulate gastric acid secretion, not pancreatic enzyme secretion.
B is incorrect because gastrin primarily stimulates gastric acid secretion, not small intestine motility and it is in response to peptides and amino acids.
C is incorrect for the same reason and gastric acid production is inhibited by somatostatin not gastrin.
E is incorrect gastrin’s main function is not to activate bile release; bile release is primarily regulated by hormones like cholecystokinin (CCK).
Question 22:
Answer: c) Vitamin D (cholecalciferol)
Explanation: Vitamin D is a fat-soluble vitamin that is primarily absorbed in the small intestine by forming micelles with dietary lipids. It plays a crucial role in calcium absorption and bone health. All these vitamins (A, D, E, and K) are absorbed by forming micelles with dietary lipids in the small intestine as they are all fat soluble.
A is incorrect as Vitamin C is water-soluble and is primarily absorbed in the small intestine through active transport mechanisms, not by forming micelles with dietary lipids.
B is incorrect as Vitamin B6 is water-soluble and is absorbed in the small intestine through passive diffusion and active transport, not by forming micelles with dietary lipids.
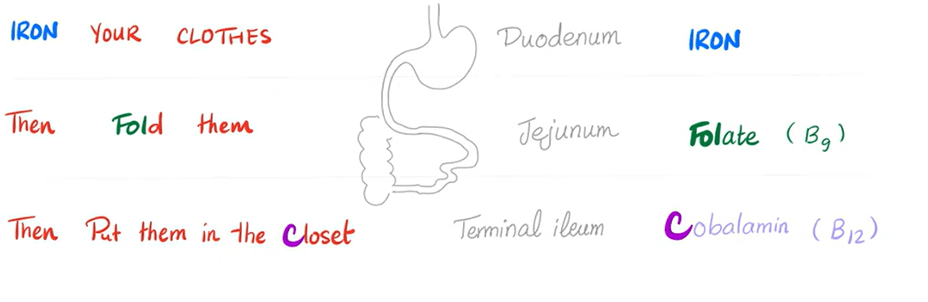
D is incorrect as Folic acid is absorbed in the small intestine through active transport mechanisms, primarily in the jejunum. It does not require micelles for absorption.
E is incorrect as Vitamin B12 is water-soluble and is absorbed in the terminal ileum of the small intestine, where it binds to intrinsic factor, not by forming micelles with dietary lipids.
Question 23:
Answer: b) Gastric phase
Explanation: The gastric phase of gastric secretion is triggered by the presence of food in the stomach. During this phase, gastric acid and pepsinogen are released to aid in digestion.
A is incorrect as the cephalic phase occurs before food enters the stomach and involves the sight, smell, taste, or even thought of food, triggering the release of gastrin, which stimulates gastric acid secretion and prepares the stomach for digestion no pepsinogen is released.
C is incorrect because the intestinal phase occurs when partially digested food (chyme) enters the duodenum. It involves the release of hormones such as secretin and cholecystokinin (CCK) from the duodenal mucosa, which inhibit gastric acid secretion and promote pancreatic enzyme secretion.
D and E are both incorrect as they are not phases.
Question 24:
Answer: b) Week 6
Explanation: Gut rotation is a critical process during gastrointestinal embryology that occurs during the sixth week of gestation. During this process, the gut tube undergoes significant changes in position and rotation around the superior mesenteric artery, ultimately forming the anatomical structures of the digestive tract.
A is incorrect as during week 3 of gestation, the primitive gut tube forms from the embryonic endoderm. This is the initial formation of the gastrointestinal tract.
C is incorrect because by week 9, gut rotation is mostly complete. The midgut returns to the abdominal cavity, and the small intestine resumes its coiled configuration.
D and E are incorrect as by this time gut rotation is fully complete and by week 22 villi are beginning to form.
Question 25:
Answer: b) Cholecystokinin (CCK)
Explanation: Cholecystokinin (CCK) is a gastrointestinal hormone that plays a crucial role in digestion. It stimulates the pancreas to release digestive enzymes and the gallbladder to contract and release bile into the duodenum. This hormone is released in response to the presence of fatty acids and amino acids in the small intestine.
A is incorrect as Gastrin primarily stimulates gastric acid secretion in the stomach and does not directly affect the pancreas or gallbladder.
C is incorrect as Somatostatin inhibits the release of various hormones, including gastrin and pepsinogen, but it does not stimulate pancreatic enzyme release or gallbladder contraction.
D is incorrect as Secretin is released from the duodenum in response to acidic chyme entering the duodenum. It stimulates the pancreatic ductal cells to release bicarbonate-rich pancreatic juice, which helps neutralize the acidic chyme. Secretin does not directly stimulate digestive enzyme release or gallbladder contraction.
E is incorrect VIP primarily functions as a neurotransmitter and vasodilator in the gastrointestinal and stimulating secretion of water and electrolytes, but it does not directly stimulate pancreatic enzyme release or gallbladder contraction.
Question 26:
Answer: c) Ileum
Explanation: Vitamin B12 absorption primarily occurs in the ileum of the small intestine. In the stomach, hydrochloric acid and pepsin help release B12 from food proteins and it binds to haptocorrin (R factor) to prevent it being digested by stomach acid. Once released, B12 binds to a protein called intrinsic factor, produced by gastric parietal cells and is released from haptocorrin since the pH is no longer acidic in the small intestines. This B12-intrinsic factor complex travels to the ileum, where specialized receptors facilitate absorption into the bloodstream.
A is incorrect as the duodenum is primarily responsible for the initial stages of digestion and absorption of nutrients such as iron and calcium, but not vitamin B12.
B is incorrect as the jejunum is involved in the absorption of various nutrients such as vitamin A,C,D,E, K and some Bs, but vitamin B12 absorption primarily occurs in the ileum.
D is incorrect as Vitamin B12 is released from dietary proteins in the stomach and then binds to intrinsic factor, but absorption occurs in the ileum, not the stomach.
E is incorrect as the colon primarily absorbs water, not vitamin B12.
Question 27:
Answer: a) Myenteric (Auerbach’s) plexus
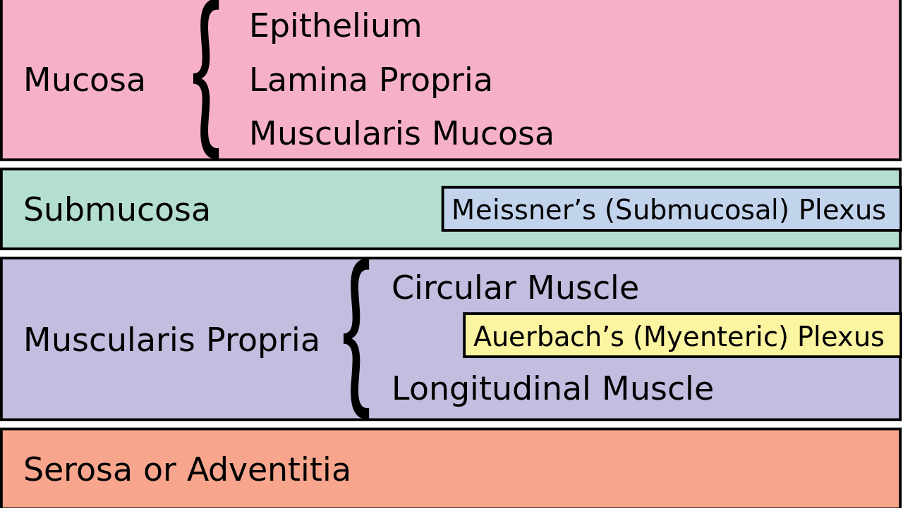
Explanation: The myenteric plexus, also known as Auerbach’s plexus, is a key component of the enteric nervous system (ENS) that resides within the muscular layers of the gastrointestinal tract. It primarily controls and regulates gastrointestinal motility, including peristalsis and segmentation, which propels food through the digestive system. Myenteric = movement. Submucosal = Secretion
B is incorrect as the submucosal plexus is involved in regulating secretions from glands and controlling blood flow in the mucosa.
C is incorrect as the celiac plexus is a network of nerves located in the abdomen that primarily innervates the upper abdominal organs, including the stomach and proximal duodenum, but it is not directly involved in coordinating digestive movements within the GI tract itself.
D is incorrect as the hypogastric plexus is in the pelvis and innervates the lower abdominal and pelvic organs, not specifically involved in regulating movements within the gastrointestinal tract.
E is incorrect these ganglia are part of the sympathetic nervous system and provide sympathetic innervation to various organs, including the gastrointestinal tract, but they do not form a plexus directly involved in coordinating and regulating digestive movements.

Question 28:
Answer: c) Somatostatin
Explanation: Somatostatin is produced by D cells in the gastrointestinal mucosa. It acts as a potent inhibitor of gastric acid secretion in the stomach. This hormone serves as a negative feedback mechanism to regulate and reduce gastric acidity when necessary.
A is incorrect as Gastrin is produced by G cells in the stomach and stimulates gastric acid secretion.
B is incorrect as CCK is produced by I cells in the duodenum and stimulates pancreatic enzyme secretion and gallbladder contraction, but it does not directly inhibit acid secretion in the stomach.
D is incorrect as Secretin is produced by S cells in the duodenum and stimulates pancreatic bicarbonate secretion to neutralize acidic chyme entering from the stomach, but it does not directly inhibit acid secretion in the stomach.
E is incorrect as Ghrelin is produced mainly by the stomach and stimulates hunger and gastric motility. It does not inhibit acid secretion in the stomach.
Question 29:
Answer: b) Gastric phase
Explanation: In the gastric phase of gastric secretion, the gastric mucosa releases intrinsic factor, which is vital for the absorption of vitamin B12 in the ileum. This phase is initiated in response to the presence of food in the stomach and prepares nutrients for further digestion and absorption.
Question 30:
Answer: a) Hypothalamus
Explanation: The hypothalamus, a region of the brain, plays a pivotal role in regulating appetite and satiety. It contains specialized nuclei that control hunger and fullness signals, making it the “satiety centre” responsible for maintaining energy balance.
B is incorrect as the amygdala is involved in processing emotions and emotional responses such as anger and fear but is not primarily responsible for regulating appetite and satiety.
C is incorrect as the hippocampus is primarily involved in memory formation and spatial navigation, rather than appetite regulation.
D is incorrect as the thalamus relays sensory and motor signals to the cerebral cortex (gateway to consciousness) but does not have a primary role in appetite regulation.
E is incorrect as the medulla oblongata controls vital functions such as breathing, heart rate, and blood pressure, but it is not directly involved in appetite regulation.
Question 31:
Answer: c) Dysbiosis is an imbalance in gut microbial communities, potentially leading to digestive disorders and inflammation.
Explanation: Dysbiosis refers to an imbalance in gut microbial communities, where harmful bacteria may outnumber beneficial ones. This imbalance can lead to digestive disorders, inflammation, and various health issues. Maintaining a healthy gut microbiota balance is crucial for overall well-being.
Question 32:
Answer: c) Immune regulation
Explanation: Kupffer cells are specialized resident macrophages within the liver, helping to maintain overall body health.
A is incorrect as this function is primarily carried out by hepatocytes, the main parenchymal cells of the liver.
B is incorrect as bile synthesis is also mainly performed by hepatocytes, which produce bile acids needed for fat digestion and absorption.
D is incorrect as stellate cells (perisinusoidal cells) in the liver store vitamin A, not Kupffer cells.
E is incorrect as this function is carried out by hepatocytes, they regulate blood glucose levels by storing glucose as glycogen (glycogenesis) or releasing glucose into the bloodstream (glycogenolysis and gluconeogenesis)
Question 33:
Answer: b) Storage of fat and vitamin A
Explanation: Stellate cells (aka ITO cells) are specialized cells in the liver responsible for storing fat and vitamin A. They play a crucial role in maintaining liver function and overall health.
A is incorrect as bile acids such as cholic acid and chenodeoxycholic acid are synthesized mainly by hepatocytes, not stellate cells.
C and D are incorrect as this function is primarily carried out by hepatocytes, the main functional cells of the liver.
E is incorrect as albumin, the most abundant protein in blood plasma, is synthesized by hepatocytes, not stellate cells.
Question 34:
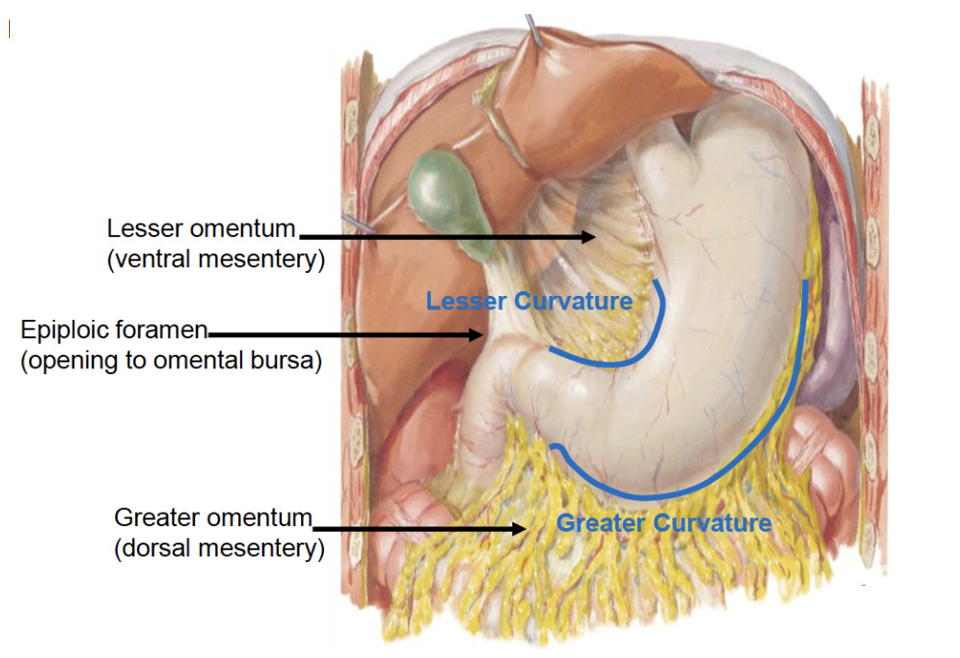
Answer: b) Mesentery
Explanation: The mesentery is the anatomical structure primarily responsible for attaching the small intestine to the posterior abdominal wall and facilitating its mobility for efficient digestion and absorption. It provides stability while allowing for the necessary movements involved in digestion and absorption, such as peristalsis and segmentation.
A is incorrect as the mesocolon attaches the colon to the posterior abdominal wall, not the small intestine.
C is incorrect the omentum (greater and lesser) is another fold of peritoneum that primarily attaches the stomach and proximal duodenum to adjacent organs and the abdominal wall. It does not attach the small intestine to the posterior abdominal wall.
D is incorrect as the peritoneum is a serous membrane that lines the abdominal cavity and covers its organs, providing support and facilitating movement but not specifically responsible for attaching the small intestine to the posterior abdominal wall.
E is incorrect as the parietal peritoneum is the outer layer of the peritoneum that lines the abdominal cavity.
Question 35:
Answer: c) Insulin sensitivity decreases in adipocytes
Explanation:In obesity, adipocytes (fat cells) often become less sensitive to insulin, a condition known as insulin resistance. This decreased insulin sensitivity can contribute to metabolic abnormalities associated with obesity, such as type 2 diabetes.
Question 36:
Answer: c) Portal circulation
Explanation: The portal circulation carries blood from the intestines to the liver for processing before it enters the systemic circulation.
A is incorrect as this the circulation of blood from the heart to the rest of the body and back to the heart, delivering oxygen and nutrients to tissues.
B is incorrect as this is the circulation of blood between the heart and the lungs, where blood picks up oxygen and releases carbon dioxide.
D is incorrect as this system transports lymph, a clear fluid containing white blood cells and waste products and plays a role in immune function and fat absorption.
E is incorrect as this is the circulation of blood through the kidneys, where waste products are filtered out of the blood and urine is produced.
Question 37:
Answer: d) Greater Curvature Stomach
Explanation: The greater omentum attaches to the greater curvature of the stomach and then drapes over the abdominal organs, like an apron. It plays a role in fat storage and immune function, helping to “wall off” areas of infection or inflammation within the abdomen.
A is incorrect the fundus is the upper portion of the stomach that expands as it fills with food. It is not primarily attached to the greater omentum.
B is incorrect as the pylorus is the lower part of the stomach that connects to the duodenum. It is not primarily attached to the greater omentum.
C is incorrect as the cardia is the area surrounding the upper opening of the stomach where the lower oesophageal sphincter is located. It is not primarily attached to the greater omentum.
E is incorrect as the lesser curvature is attached to the lesser omentum.
Question 38:
Answer: c) Acinar cells
Explanation: Acinar cells in the exocrine portion of the pancreas produce and secrete digestive enzymes, such as trypsinogens, amylases, proteases, and lipases, into the small intestine. These enzymes play a crucial role in breaking down carbohydrates, proteins, and fats from ingested food, facilitating their absorption. In contrast, alpha and beta cells are part of the endocrine pancreas, responsible for hormone production (glucagon and insulin), while duct cells are involved in transporting pancreatic secretions.
A is incorrect as alpha cells secrete glucagon in response to hypoglycaemia (e.g. during fasting) to increase blood glucose.
B is incorrect as beta cells secrete insulin in response to hyperglycaemia (e.g. after a meal) to decrease blood glucose.
D is incorrect as islets include alpha and beta cells, as well as delta cells (which produce somatostatin). They are involved in regulating blood glucose levels and do not directly produce digestive enzymes.
E is incorrect as ductal cells are responsible for the passage of digestive enzymes from acinar cells and producing bicarbonate.
Question 39:
Answer: c) Alanine aminotransferase (ALT)
Explanation: Alanine aminotransferase (ALT) is a liver enzyme primarily found within hepatocytes. When liver cells are damaged or undergo necrosis, ALT is released into the bloodstream, resulting in elevated serum ALT levels. This makes it a valuable marker for hepatocellular damage, often seen in conditions like viral hepatitis or drug-induced liver injury. The other enzymes listed are also involved in liver function but are less specific for hepatocellular damage compared to ALT.
A is incorrect as ALP is an enzyme found in many tissues throughout the body, including the liver, bones, kidneys, and intestines. Elevated ALP levels may indicate liver or bone disease or bile obstruction, but it is not specific to hepatocellular damage.
B is incorrect as albumin is a protein synthesized by the liver and is important for maintaining oncotic pressure in the blood. Its levels may decrease in chronic liver disease, but it is not used as a marker for hepatocellular damage.
D is incorrect as GGT is another enzyme found in the liver and other tissues. Elevated GGT levels can indicate liver disease or bile duct obstruction, but it is less specific for hepatocellular damage compared to ALT as it can also increase during pregnancy and due to alcohol.
E is incorrect as PT measures the time it takes for blood to clot. It is used to assess the clotting ability of the blood and is prolonged in liver disease due to impaired production of clotting factors by the liver. However, it is not a direct marker for hepatocellular damage like ALT.
Question 40:
Answer: b) Treg and Trefoil peptides
Explanation: Trefoil peptides promote cell migration and proliferation of epithelial cells, aiding in the repair of damaged mucosa and are involved in mucosal restitution after injury, helping to restore the integrity of the epithelial barrier. Treg cells play a role in modulating immune responses and preventing excessive inflammation that could damage the GI epithelium.
A is incorrect as the vomiting reflex is a protective mechanism to expel harmful substances from the stomach but does not directly contribute to maintaining the integrity of the gastrointestinal epithelium during injury.
C is incorrect as mucosal secretion of mucus and bicarbonate helps protect the gastrointestinal epithelium from acidic gastric contents and other irritants, but it primarily serves as a protective barrier rather than directly repairing injured epithelium.
D is incorrect as although gastrin is involved in maintaining the physiology of the stomach it is not the main factor that does, also hypovolaemia would decrease blood to the site of injury which is the opposite of what usually happens as usually hypervolemia occurs whereby there is more CGRP and NO so that the damaged area receives more growth factors and immune cells.
E is incorrect as defecation is the process of eliminating waste from the body and does not contribute to maintaining gastrointestinal epithelial integrity in response to injury.
Question 41:
Answer: a) Sodium-glucose transporter (SGLT)
Explanation: The sodium-glucose transporter (SGLT) is responsible for the active absorption of monosaccharides, such as glucose and galactose, in the small intestine via cotransport system with Sodium.
B is incorrect as the Na+/K+ pump maintains the sodium and potassium gradients across the cell membrane, which are crucial for the function of SGLT in transporting glucose and galactose. This not the best answer.
C is incorrect as GLUT 2 is a glucose transporter that facilitates the movement of glucose, galactose, and fructose across the basolateral membrane of enterocytes (small intestine cells) into the bloodstream after absorption. It is not primarily responsible for absorption from the lumen into the small intestine. This would’ve been correct if the question asked about the transport of monosaccharides from the small intestine into the blood.
D is incorrect as GLUT 4 is primarily found in muscle and adipose tissue and is involved in insulin-mediated glucose uptake into these tissues, rather than intestinal absorption.
E is incorrect as GLUT 5 transports fructose across the apical membrane of enterocytes. It is responsible for the absorption of dietary fructose rather than glucose or galactose.
Question 42:
Answer: c) M cells
Explanation: M cells, also known as microfold cells, are specialized cells found in Peyer’s patches and other lymphoid tissues in the gastrointestinal tract. Their primary function is to capture and transport antigens from the gut lumen to immune cells in the underlying lymphoid tissue, initiating an immune response to potential pathogens and antigens.
A is incorrect as goblet cells secrete mucus to lubricate and protect the epithelial surface of the intestines. They do not play a direct role in capturing and presenting antigens.
B is incorrect as paneth cells secrete antimicrobial peptides. They are involved in innate immune defence rather than antigen presentation.
D is incorrect as immunoglobulin A (IgA) is an antibody secreted by Peyer’s patches in the lamina propria of the ileum. While IgA plays a critical role in mucosal immunity by neutralizing pathogens and toxins, it is not a cell type involved in antigen capture and presentation.
E is incorrect as p cells are not a cell type in the context of gut-associated lymphoid tissue (GALT) or antigen presentation.
Question 43:
Answer: a) Activation of CFTR channels
Explanation: Cholera toxin binds to GM1 receptors on intestinal epithelial cells and enters the cells. The A subunit of the toxin catalyses the transfer of an ADP-ribose group from NAD+ (nicotinamide adenine dinucleotide) to a G protein (Gs) alpha subunit. This ADP-ribosylation modifies the G protein, preventing it from hydrolysing GTP to GDP, thereby locking the G protein in its active GTP-bound state, this activates adenylate cyclase. This activation increases intracellular levels of cyclic AMP (cAMP), which in turn phosphorylates and opens CFTR (Cystic Fibrosis Transmembrane Conductance Regulator) channels on the apical surface of the intestinal epithelial cells. CFTR channels allow chloride ions (Cl⁻) to move from the cytoplasm into the intestinal lumen. This creates an osmotic gradient that drives the secretion of sodium ions (Na⁺) and water into the lumen through paracellular and sometimes transcellular routes, leading to diarrhoea.
B is incorrect as inhibition of sodium-potassium ATPase would impair active transport of ions across the cell membrane, potentially leading to reduced ion and water secretion, rather than excessive secretion characteristic of secretory diarrhoea.
C is partially correct as cholera does activate GPCR but the main reason for excessive water secretion is CFTR, therefore this is not the best answer.
D is incorrect as inhibition of aquaporins would reduce water movement which would therefore reduce diarrhoea.
E is partially correct but not the best answer as although both paracellular and transcellular transport routes can contribute to the movement of ions and water in secretory diarrhoea, they are not the primary mechanisms induced by cholera toxin. Cholera toxin primarily induces secretion via CFTR activation and subsequent ion transport.
Question 44:
Answer: d) Pancreas
Explanation: Trypsinogen, the inactive precursor of trypsin, is initially secreted by the pancreas. It is later activated into trypsin within the small intestine, where it plays a crucial role in protein digestion. It is then activated by enterokinases/ enteropeptidases in the duodenum into trypsin, and then trypsin activates the other zymogens such as chymotrypsinogen into trypsin.
Question 45:
Answer: b) Vitamin C
Explanation: Vitamin C, also known as ascorbic acid, is primarily absorbed in the small intestine and plays essential roles in collagen formation essential for wound healing and the maintenance of skin, cartilage, tendons, ligaments, and blood vessels. It also functions as a potent antioxidant, protecting cells from oxidative stress and supporting the immune system. Knowing that only Vitamin A, D, E and K are fat-soluble, you can come to conclusion that Vitamin C is water soluble.
A is incorrect as Vitamin A is a fat-soluble vitamin important for vision, immune function, and skin health.
C is incorrect as Vitamin D is a fat-soluble vitamin vital for calcium absorption and bone health.
D is incorrect as Vitamin E is a fat-soluble antioxidant that protects cell membranes from oxidative damage.
E is incorrect as Vitamin K is a fat-soluble vitamin essential for blood clotting.
Question 46:
Answer: e) Detection and response to luminal contents and reflexes in the mucosa
Explanation: The submucosal plexus plays a key role in detecting and responding to luminal contents, as well as coordinating reflexes within the mucosa of the gastrointestinal tract. It is involved in regulating various aspects of gut function, including local reflexes related to digestion and absorption, sensory functions, local blood flow regulation and secretion.
Question 47:
Answer: c) Meissner’s plexus is involved in secretion and absorption, whereas Myenteric plexus mainly coordinates muscle contractions and motility.
Explanation:
Meissner’s plexus primarily regulates activities related to the mucosal layer, including secretion and absorption, while Myenteric plexus is mainly responsible for controlling muscle contractions and motility throughout the gastrointestinal tract. This distinction highlights their complementary roles within the enteric nervous system. Myenteric plexus = motility/movement Submucosal plexus = Secretion
Question 48:
Answer: e) Cholestasis
Explanation: Cholestasis is one of the conditions that can result in elevated levels of bilirubin, alkaline phosphatase (ALP), and gamma-glutamyl transferase (GGT) in liver function tests (LFTs). This combination of abnormal markers often indicates impaired or blocked bile flow within the liver or bile ducts.
Question 49:
Answer: d) Albumin is a marker for synthetic function, as it is primarily synthesized by the liver.
Explanation: Albumin is a key protein produced by the liver, and its presence in the blood serves as a marker for the liver’s synthetic function. A decrease in serum albumin levels can indicate impaired liver synthetic function, which can occur in various liver diseases or conditions affecting the liver’s ability to produce proteins.
A is incorrect as hepatocellular injury is better indicated by elevated levels of enzymes such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST) not albumin.
B is incorrect as clotting function is more directly assessed by other markers such as prothrombin time (PT) and international normalized ratio (INR).
C is incorrect as bile duct obstruction is better indicated by elevated levels of enzymes such as alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT).
Question 50:
Answer: e) diarrhoea
Explanation: Excessive hypermotility in the GI tract can result in rapid transit of food and fluids, leading to diarrhoea, diarrhoea is characterized by increased frequency and loose or watery stools, often due to reduced absorption time in the intestine.
A is incorrect as this is usually a result of hypomotility, not hypermotility.
B is incorrect as hypermotility would likely decrease nutrient absorption due to faster transit time through the gut.
C is incorrect as constipation is typically associated with hypomotility, where the movement through the intestines is slower than normal.
D is incorrect as hypermotility does not directly cause excessive bile secretion.
Question 51:
Answer: d) Promotion of blood flow to the GI mucosa
Explanation: One of the primary functions of prostaglandins in the GI mucosa is the promotion of blood flow. Prostaglandins can dilate blood vessels in the mucosal layer, helping to ensure an adequate supply of oxygen and nutrients, and contributing to the mucosal defence mechanisms.
Question 52:
Answer: a) Immunoglobulin A (IgA)
Explanation: The polymeric immunoglobulin receptor (pIgR) transports and secretes Immunoglobulin A (IgA) across mucosal surfaces, including the gastrointestinal tract. IgA plays a critical role in mucosal immunity, where it helps protect against pathogens and antigens in the mucosal environment.
B is incorrect as IgG is primarily found in blood and extracellular fluid, produced during secondary exposure to an antigen and passed down from the mother to foetus via the placenta; not transported via pIgR.
C is incorrect as IgM is found in the blood and is the first antibody produced during an immune response; not the primary immunoglobulin transported by pIgR.
D is incorrect as it functions mainly as a receptor on B cells and is not involved in mucosal transport.
E is incorrect as IgE is involved in allergic responses and defence against parasitic infections; not transported by pIgR.
Question 53:
Answer: c) Trigeminal nerve (cranial nerve V)
Explanation: The trigeminal nerve (cranial nerve V) is primarily responsible for motor control during mastication. It innervates the muscles involved in chewing, including the temporalis and masseter muscles.
A is incorrect because the vagus nerve is not responsible for mastication but is involved in parasympathetic control of the GI tract.
B is incorrect as the glossopharyngeal nerve is involved in taste and other functions in the oropharynx, but not in mastication.
D is incorrect as the hypoglossal nerve controls tongue movements but not the muscles of mastication.
E is incorrect as the accessory nerve innervates the sternocleidomastoid and trapezius muscles (neck muscles), but not the muscles involved in mastication.
Question 54:
Answer: b) Parotid gland – Innervated by the glossopharyngeal nerve (cranial nerve IX); Sublingual and Submandibular glands – Innervated by the facial nerve (cranial nerve VII)
Explanation: The parotid gland is primarily innervated by the glossopharyngeal nerve (cranial nerve IX), while both the sublingual and submandibular glands are primarily innervated by the facial nerve (cranial nerve VII). These innervation patterns are based on the most common patterns observed in human anatomy.
Question 55:
Answer: c) Sympathetic innervation stimulates the secretion of protein-rich saliva.
Explanation: In the context of salivary glands, sympathetic innervation typically stimulates the secretion of protein-rich saliva. This protein-rich saliva contains enzymes for initial digestion. Parasympathetic stimulation causes secretion of fluid.
A is incorrect watery, enzyme rich saliva is stimulated by parasympathetic innervation.
D is partially correct as it does enhance specific components of saliva, but this is not the best answer since there is no mention to proteins.
Question 56:
Answer: b) ICC generate and propagate electrical slow waves that coordinate smooth muscle contractions.
Explanation: The primary role of interstitial cells of Cajal (ICC) in the gastrointestinal system is to regulate peristalsis and gastrointestinal motility by generating slow waves the cause these peristaltic contractions. They serve as pacemaker cells that generate electrical impulses to coordinate the rhythmic contractions of the gut, facilitating the movement of food through the digestive tract.
A is incorrect because the primary role of ICC is not directly related to nutrient absorption or villus motility.
C is incorrect because, while ICC can respond to mechanical stimuli and play a role in mechanical transduction, their primary function is generating and propagating electrical slow waves for coordinated muscle contractions.
D is incorrect because ICC do not secrete digestive enzymes. The secretion of digestive enzymes is mainly the role of other cells in the gastrointestinal tract, such as the acinar cells in the pancreas and chief cells in the stomach.
E is incorrect because ICC are not primarily involved in mediating immune responses. Immune functions in the gastrointestinal tract are primarily handled by other cells such as immune cells in the gut-associated lymphoid tissue (GALT) such as Peyer’s patches.
Question 57:
Answer: d) Hypoglossal nerve (cranial nerve XII)
Explanation: The hypoglossal nerve (cranial nerve XII) is primarily responsible for controlling the voluntary movement of the tongue’s intrinsic and extrinsic muscles, allowing for functions like speech and swallowing.
A is incorrect as the trigeminal nerve is primarily responsible for mastication and motor functions such as biting and chewing, but it does not control the muscles of the tongue.
B is incorrect the facial nerve controls the muscles of facial expression and the secretion of saliva and tears by innervating the anterior 1/3 of the tongue and the submandibular and sublingual glands, but it does not control the tongue’s movement.
C is incorrect as the glossopharyngeal nerve is involved in taste sensation from the posterior one-third of the tongue, innervating the parotid gland for secretion of saliva and some motor function in the pharynx, but it is not primarily responsible for tongue movement.
E is incorrect as the vagus nerve controls many functions, including heart rate, gastrointestinal peristalsis, and muscle movements in the larynx, but it is not the main nerve for tongue movement.
Question 58:
Answer: e) GLUT5
Explanation: Fructose is transported into enterocytes (cells of the small intestine) primarily by the GLUT5 transporter protein. This facilitated diffusion allows fructose to enter the bloodstream for further metabolism.
A is incorrect as GLUT1 is responsible for the basal glucose uptake in many tissues, including the brain and red blood cells. It ensures a constant supply of glucose for cellular metabolism.
B is incorrect as GLUT2 is a low-affinity, high-capacity glucose transporter found in the liver, pancreas, kidneys, and the basolateral membrane of enterocytes. It plays a key role in glucose sensing and regulation, facilitating the transport of glucose, galactose, and fructose out of the enterocytes into the bloodstream.
C is incorrect as GLUT3 is a high-affinity glucose transporter predominantly found in neurons and the placenta. It ensures efficient glucose uptake in cells with high glucose demands, such as neurons.
D is incorrect as GLUT4 is an insulin-regulated glucose transporter primarily found in adipose tissue and striated muscle (skeletal and cardiac muscles). It plays a crucial role in glucose uptake in response to insulin, especially postprandially (after eating).
Question 59:
Answer: c) Gastrin stimulates cell proliferation and mucosal growth.
Explanation: Gastrin stimulates the proliferation of certain cells in the gastrointestinal mucosa, promoting mucosal growth and repair. This hormone plays a crucial role in maintaining the integrity of the GI tract.
A is incorrect as it is true, it does not address the repair and maintenance of the GI mucosa. Gastrin does indeed stimulate gastric acid (HCl) secretion by parietal cells in the stomach, but this function is not related to mucosal repair. B is incorrect as Gastrin does not inhibit bicarbonate production. Secretin is the hormone that stimulates the production of bicarbonate.
D is incorrect as Gastrin does not decrease blood flow to the GI mucosa. In fact, adequate blood flow is essential for delivering nutrients and oxygen for tissue repair. Prostaglandins and other local factors such as CGRP and NO are more involved in regulating mucosal blood flow.
E is incorrect as Gastrin does not activate enzymes that digest the mucosal lining. Pepsin, an enzyme that digests proteins, is activated in the stomach, but it is not activated by gastrin. Instead, pepsinogen is converted to pepsin by the acidic environment in the stomach (which gastrin helps to create by stimulating acid production).
Question 60:
Answer: b) Two layers of mucus
Explanation: The large intestine, or colon, usually has two layers of mucus. These layers help protect the intestinal epithelium from mechanical damage and play a role in facilitating the movement of stool through the colon. Inner layer is firmly attached to the epithelial cells and is dense and thick, providing a barrier against bacteria and other potentially harmful substances. The outer layer is looser and thicker, allowing for the lubrication and smooth passage of stool. The oesophagus has a single layer of mucus which helps protect the oesophageal epithelium from damage due to the passage of food and liquids. The stomach also has a single continuous layer of mucus which helps protect the stomach lining from the acidic environment and digestive enzymes present in gastric juice. The small intestine has a single discontinuous layer of mucus that is not uniformly distributed but is instead produced in response to local stimuli and protects the epithelium from mechanical damage and chemical irritation.
Question 61:
Answer: d) Increased levels of SCFA and gram-positive bacteria
Explanation: A high fruit and legume fibre diet is associated with increased production of short-chain fatty acids (SCFA), which contribute to a healthier gut environment by inhibiting the establishment of pathogenic bacteria and supporting the growth of beneficial gut microbes.
A is incorrect because a diet high in fruits and legumes is rich in dietary fibre promotes the production of SCFAs through fermentation by beneficial gut bacteria, including many gram-positive bacteria.
B is incorrect because a diet high in fruits and legumes generally supports a healthy gut microbiome, reducing the risk of pathogenic bacteria colonization. The fibre in such diets supports beneficial bacteria that outcompete harmful bacteria.
C is incorrect because a high-fibre diet from fruits and legumes tends to support the growth of beneficial bacteria rather than harmful ones. SCFAs produced from fibre fermentation create an environment that is less favourable for harmful gram-negative bacteria.
E is incorrect because the question focuses on a diet rich in fruits and legumes, not animal proteins. Such a diet promotes beneficial bacteria that thrive on fibre, not the bacteria that digest animal proteins. Additionally, gram-negative bacteria are more commonly associated with less beneficial or harmful gut flora.
Question 62:
Answer: c) SCFAs increase insulin sensitivity in muscle.
Explanation: SCFAs are known to increase insulin sensitivity in muscle tissue. This effect promotes glucose uptake by muscle cells, contributing to improved glucose regulation in the body.
Question 63:
Answer: c) Incretins stimulate insulin secretion and inhibit glucagon release from the pancreas.
Explanation: Incretins, such as GIP and GLP-1, stimulate the secretion of insulin from the pancreas and inhibit the release of glucagon. These actions contribute to the regulation of blood glucose levels by promoting glucose uptake and reducing glucose production.
A is incorrect because incretins like GIP and GLP-1 increase insulin release from the pancreas in response to food intake, thereby helping to lower blood glucose levels.
B is incorrect because incretins do not primarily act on the liver to release glucose. Instead, they stimulate insulin secretion from the pancreas and inhibit glucagon release, both of which help lower blood glucose levels. The hormone glucagon, not incretins, primarily acts on the liver to release glucose into the bloodstream.
D is incorrect because incretins have a significant effect on blood glucose levels. They help lower blood glucose by stimulating insulin secretion and inhibiting glucagon release.
E is incorrect absorption of nutrients into the small intestine is not facilitated by incretins, this is managed by other enzymes and transport proteins.
Question 64:
Answer: d) Motilin enhances GI motility and clears residual material from the gut.
Explanation: During fasting, motilin plays a role in enhancing gastrointestinal motility, particularly in the stomach and small intestine. This action helps clear residual material from the GI tract, preparing it for the next intake of food.
A is incorrect because motilin does not primarily stimulate the release of digestive enzymes from the pancreas. This function is mainly carried out by cholecystokinin (CCK), which stimulates the pancreas to release digestive enzymes in response to the presence of fats and proteins in the small intestine.
B is incorrect because motilin does not primarily stimulate hydrochloric acid secretion. Gastrin is the hormone primarily responsible for stimulating hydrochloric acid secretion in the stomach.
C is incorrect because motilin stimulates smooth muscle contractions to enhance GI motility. The inhibition of smooth muscle contractions can be carried out by neurotransmitters like nitric oxide and VIP.
E is incorrect because motilin does not primarily affect blood flow to the GI mucosa. Blood flow regulation in the GI tract is influenced by various factors, like prostaglandins, and neural control like CGRP and NO, rather than motilin.
Question 65:
Answer: d) MMC moves undigested food and bacteria from the stomach and small intestine to the colon during fasting.
Explanation: The primary function of the migrating myoelectric complex (MMC) is to enhance gastrointestinal motility and clear residual material from the gut during fasting. This cyclic pattern helps prepare the GI tract for the next intake of food and to maintain the guts cleanliness during fasting.
A is incorrect because the MMC primarily functions during fasting, not in response to food intake. The secretion of bile and pancreatic juice in response to food intake is mainly stimulated by the hormone cholecystokinin (CCK).
B is incorrect because nutrient absorption occurs primarily through the coordinated action of digestive enzymes and the epithelial cells lining the small intestine, facilitated by the presence of food. The MMC is involved in cleaning the gut during fasting, not in nutrient absorption.
C is incorrect because the release of gastric acid is primarily triggered by the hormone gastrin, particularly in response to food in the stomach.
E is incorrect because the relaxation of the lower oesophageal sphincter to allow food entry into the stomach is primarily regulated by neural mechanisms involving the vagus nerve.
Question 66:
Answer: e) Myenteric plexus
Explanation: The myenteric plexus is the neural network situated within the tissue layer between the circular and longitudinal muscle layers of the GI tract. It plays a crucial role in regulating GI motility, including processes like peristalsis, and mixing of food with digestive enzymes.
Question 67:
Answer: a) Stomach
Explanation: The stomach is the digestive organ that contains specialized oblique muscles within its muscular layers. These oblique muscles enable the stomach to perform twisting and squeezing motions, aiding in the mechanical digestion of food.
Question 68:
Answer: c) It is a feedback loop that includes both afferent and efferent branches of the vagus nerve, aiding in GI regulation.
Explanation: The vago-vagal reflex is a sophisticated neural mechanism that facilitates communication between the gastrointestinal (GI) tract and the brain. It involves a two-way interaction mediated by the vagus nerve (cranial nerve X). This reflex serves as a feedback loop, where afferent (sensory) signals from the GI tract are transmitted to the brain, providing information about various aspects of GI function, such as distension, pH, and nutrient content. Subsequently, efferent (motor) signals are sent back to the GI tract to modulate activities like peristalsis, secretion, and motility.
Question 69:
Answer: c) Chylomicrons transport dietary lipids, such as triglycerides, from the small intestine to peripheral tissues.
Explanation: Chylomicrons play a crucial role in the transport of dietary lipids for example LCFA, particularly triglycerides, from the small intestine to peripheral tissues, where they can be used for energy or stored. This process ensures the efficient utilization of dietary fats for various physiological functions.
A is incorrect as glucose storage in the liver is primarily facilitated by glycogen, not chylomicrons.
B is incorrect as water-soluble vitamins (such as vitamin C and B-complex vitamins) are absorbed through specific transport mechanisms in the small intestine, not via chylomicrons.
D is incorrect as digestive enzymes (such as pepsin) are secreted by cells in the stomach such as chief cells, not by chylomicrons.
E is incorrect as blood glucose levels are primarily regulated by insulin and glucagon, hormones produced by the pancreas, and not by chylomicrons.
Question 70:
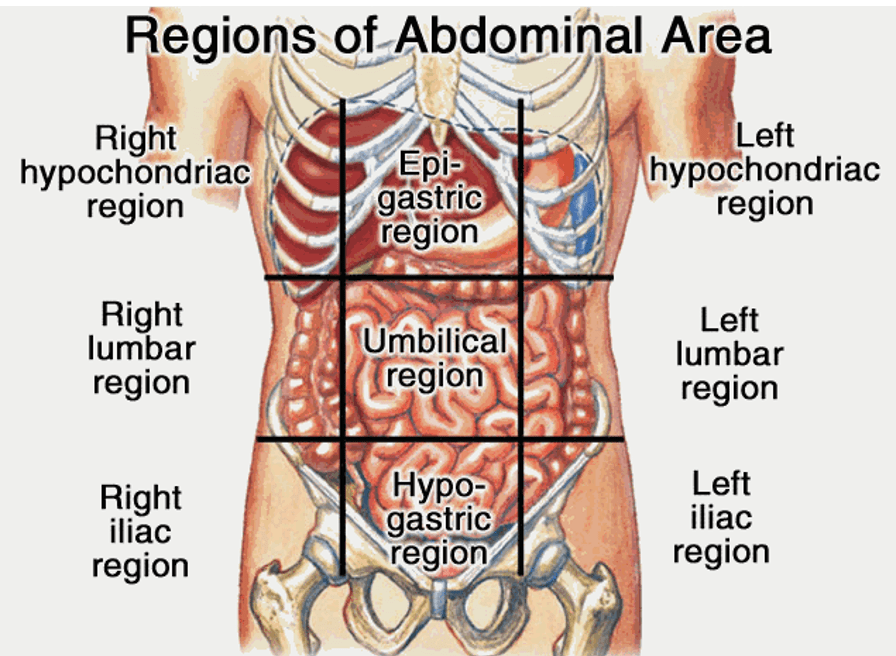
Answer: e) They are in the upper lateral parts of the abdomen, on either side of the epigastric region.
Explanation: The hypochondriac regions are in the upper lateral parts of the abdomen, on either side of the epigastric region. They are important anatomical reference points and are often used in medical examinations to describe the location of abdominal structures or symptoms.
Question 71:
Answer: c) Peristalsis in the oesophagus involves simultaneous contraction of circular and longitudinal muscle layers.
Explanation: Peristalsis in the oesophagus involves a coordinated sequence of contractions that includes both circular and longitudinal muscle layers working together to propel food downward. It is a reflexive, involuntary process, not under conscious control. Peristalsis is characterized by alternating contractions and relaxations of the circular and longitudinal muscles in the GI tract. Above the bolus the longitudinal muscle relaxes due to VIP and NO whilst the circular muscle contracts due ACH and tachykinin whilst around the bolus the stretch is detected by serotonin. Serotonin activates intrinsic primary afferent neurons (IPANs) in the enteric nervous system, initiating the peristaltic reflex and creating contractions. These contractions create waves that push the contents forward through the digestive system. Below the bolus the circular muscle relaxes and the longitudinal muscle contracts. This is regulated by the autonomic nervous system and the enteric nervous system and occurs throughout the GI tract: in the oesophagus, stomach, small intestines, and colon. Parasympathetic Nervous System enhances peristalsis through the action of the vagus nerve, which releases acetylcholine. Sympathetic Nervous System inhibits peristalsis and relaxes the muscle tone through the release of norepinephrine/noradrenaline.
Question 72:
Answer: c) Porta hepatis denotes the site where the hepatic artery, portal vein, and common bile duct enter and exit the liver.
Explanation: The term “porta hepatis” refers to a crucial anatomical location in the liver where the hepatic artery, portal vein, and common bile duct enter and exit. This site is of great importance for the liver’s vascular supply and the transport of bile.
Question 73:
Explanation: The central vein, also known as the central venule or intralobular vein, is located at the central region of a liver lobule. It collects blood from hepatic sinusoids and serves as the starting point for larger hepatic veins, which are responsible for draining blood from the liver. This central vein plays a key role in the hepatic circulation and the overall function of the liver lobule.
Question 74:
Answer: a) Vitamin A
Explanation: Bile is essential for the digestion and absorption of fat-soluble vitamins, including vitamin A. Bile emulsifies dietary fats, allowing the enzymes and intestinal mucosa to access and absorb fat-soluble vitamins efficiently. Vitamin A is important for vision, immune function, and skin health, and its absorption is closely linked to the presence of bile in the digestive process. The other vitamins also dependent on bile for absorption are Vitamin D: Crucial for calcium absorption and bone health, Vitamin K: Important for blood clotting and bone health and Vitamin E: An antioxidant that protects cells from damage.
B and C are incorrect as they are water soluble vitamins that require their own transport channels for absorption.
D is incorrect as Vitamin B12 (cobalamin) is a water-soluble vitamin and does not rely on bile for absorption. Instead, it requires intrinsic factor, a protein secreted by the stomach, for its absorption in the ileum.
E is incorrect as Vitamin C water-soluble vitamin, which is absorbed directly into the bloodstream from the small intestine via active transport mechanisms and does not require bile.
Question 75:
Answer: d) In the liver
Explanation: Bile is primarily produced in the liver as a crucial digestive fluid that aids in the emulsification and absorption of dietary fats.
A is incorrect the pancreas produces digestive enzymes (such as trypsinogen, chymotripsogen, amylase, lipase, and proteases) and bicarbonate. These enzymes are released into the duodenum to aid in the digestion of carbohydrates, fats, and proteins. Additionally, the pancreas produces insulin and glucagon to regulate blood sugar levels.
B is incorrect as the stomach produces gastric juice, which contains hydrochloric acid (HCl) and pepsinogen. HCl helps break down food and activates pepsinogen (made in chief cells) to pepsin, an enzyme that begins protein digestion. The stomach also produces intrinsic factor from parietal cells, essential for the absorption of Vitamin B12 in the small intestine.
C is incorrect as the small intestine is the primary site for digestion and absorption of nutrients. It produces enzymes such as lactase, maltase, and sucrase to digest carbohydrates. It also receives bile from the liver and digestive enzymes from the pancreas to further aid in the digestion and absorption of fats, proteins, and carbohydrates.
E is incorrect the gallbladder stores and concentrates bile produced by the liver. When food, especially fatty food, enters the small intestine, the gallbladder releases bile into the small intestine to aid in fat digestion and absorption.
Question 76:
Answer: a) Hepatocytes
Explanation: Hepatocytes, the main functional cells of the liver, are primarily responsible to produce bile.
B is incorrect as acinar cells are found in the pancreas and are responsible for producing digestive enzymes such as trypsinogen, amylase, lipase, and proteases. These enzymes are secreted into the pancreatic ducts and then into the duodenum to aid in digestion.
C is incorrect as stellate cells aka ITO cells are involved in the storage of vitamin A and the regulation of extracellular matrix production. They play a role in liver fibrosis when activated.
D is incorrect as Kupffer cells are specialized macrophages located in the liver and are involved in the removal of pathogens, dead cells, and debris from the blood as it passes through the liver.
E is incorrect as mucous cells are found in various parts of the gastrointestinal tract, including the stomach and intestines. They produce mucus, which lubricates and protects the lining of the GI tract from mechanical damage and the acidic environment of the stomach.
Question 77:
Answer: a) Cystic duct
Explanation: The cystic duct connects the gallbladder to the common bile duct, allowing bile to be stored and released as needed for digestion in the small intestine.
Question 78:
Answer: b) Tinea coli assists in the mixing and propulsion of faecal material.
Explanation: The tinea coli, or taenia coli, are three longitudinal bands of smooth muscle in the colon. They play a crucial role in the mixing and propelling of faecal material through the colon, contributing to the process of peristalsis and the formation of haustra, the characteristic sac-like structures in the colon.
Question 79:
Answer: c) Because diverticula bud from the duodenum during embryonic development.
Explanation: During embryonic development, diverticula (outpouchings) bud from the duodenum, giving rise to the liver, pancreas, and gall bladder. These organs maintain their anatomical connection to the duodenum as they develop. Consequently, their secretions, including bile from the gall bladder, pancreatic enzymes, and liver-produced substances like bile, are directed into the duodenum to facilitate digestion and absorption of nutrients at the beginning of the small intestine. This developmental origin explains why these organs empty into the duodenum. Also, the duodenum receives acidic chyme from the stomach, and it is essential to neutralize this acid to protect the intestinal lining and provide an optimal pH for enzyme activity. The pancreas secretes bicarbonate along with digestive enzymes to neutralize the acid, while bile from the liver emulsifies fats, aiding in their digestion and absorption which occurs due to its embryological origin.
Question 80:
Answer: c) 270 degrees around the superior mesenteric artery.
Explanation: During embryonic development, the midgut rotates approximately 270 degrees around the axis formed by the superior mesenteric artery (SMA) as it herniates into the umbilical cord and subsequently returns to the abdominal cavity. Understanding these rotations is crucial in comprehending the final anatomical positions of the midgut structures.
Question 81:
Answer: c) Pudendal nerve, originating from the sacral spine (S2-S4).
Explanation: The pudendal nerve, originating from the sacral spine (S2-S4), provides voluntary control over the external anal sphincter, allowing individuals to regulate the opening and closing of the anal canal. This control is essential for faecal continence and the regulation of defecation.
A is incorrect because the pelvic splanchnic nerves provide parasympathetic innervation to the internal anal sphincter, not voluntary control over the external anal sphincter.
B is incorrect because the superior rectal nerve is a branch of the inferior mesenteric nerve and innervates the upper part of the rectum, not the external anal sphincter.
E is incorrect as provides sensory innervation to the skin around the coccyx and the anal canal. It does not have motor control over any of the sphincters in the pelvic region.
Question 82:
Answer: b) Masseter muscle
Explanation: The masseter muscle is one of the primary muscles responsible for closing the jaw during activities such as chewing, biting, and clenching. It is a powerful muscle located in the jaw area. While the other muscles listed have important roles in head and neck movements, they are not primarily responsible for closing the jaw.
A is incorrect as the digastric muscle is involved in opening the jaw rather than closing it. It helps with actions like swallowing and speaking.
C is incorrect as lateral pterygoid plays a role in opening the jaw by pulling the condyle of the mandible forward. It is involved in lateral and protrusive movements of the jaw rather than closing it.
D is incorrect as it is in the neck and is involved in various movements of the head and neck and in inspiration, but it does not directly participate in the closure of the jaw.
E is incorrect as is primarily involved in movements of the shoulder and neck, such as raising and lowering the shoulders and extending the head, but it is not involved in jaw closure.
Question 83:
Answer: c) Saliva provides a source of calcium and phosphate ions.
Explanation: Saliva contains calcium and phosphate ions that help buffer the acidic environment in the mouth. These ions can remineralize enamel, counteracting the demineralization caused by acids. Demineralization weakens the enamel, making teeth more susceptible to decay. Saliva helps to neutralize acids and replenish minerals, thereby strengthening and protecting tooth enamel. Additionally, saliva helps maintain a stable oral pH, further protecting teeth from acid attack and promoting overall oral health.
A is incorrect as although saliva does buffer acids in the mouth to some extent, its primary role is not to neutralize acids but rather to help maintain a slightly alkaline pH in the oral cavity, which is optimal for oral health. Therefore, this is not the best answer.
B is incorrect as although saliva does contain proteins that can form a film on tooth surfaces, this barrier is more for lubrication and protection against mechanical forces rather than a direct protective barrier against acids or bacteria.
While D is true that saliva contains components that can help control bacterial growth in the mouth, such as antimicrobial proteins, its primary protective function for teeth lies in providing minerals for remineralization rather than directly inhibiting acid-producing bacteria. Therefore, this isn’t the best answer either.
E is partially correct but not the best answer because saliva does contain fluoride ions, which can enhance remineralization and strengthen tooth enamel. However, this is also a secondary function compared to providing calcium and phosphate ions.
Question 84:
Answer: a) Stomach and upper duodenum
Explanation: The foregut gives rise to the stomach and the upper part of the duodenum and is innervated by the Celiac trunk.
B, D and E are incorrect as they are derived from the midgut during embryonic development, not the foregut and innervated by the Superior Mesenteric Artery.
C is incorrect as they are derived from the hindgut during embryonic development, not the foregut and innervated by the inferior mesenteric artery.
Question 85:
Answer: c) Cecum, appendix, and ascending colon
Explanation: The midgut develops into the cecum, appendix, ascending colon, and a portion of the transverse colon.
A is incorrect they are derived from the foregut during embryonic development.
B is incorrect as they are derived from the hindgut during embryonic development.
D is incorrect as the spleen is derived from mesodermal cells and the pancreas is derived from the dorsal (gives rise to neck, body, and tail) and ventral pancreatic bud (gives rise to the uncinate process), which originate from endodermal cells of the foregut.
E is incorrect as they are derived from the hindgut during embryonic development.
Question 86:
Answer: d) Descending colon and sigmoid colon
Explanation: The hindgut primarily forms the descending colon and sigmoid colon during embryonic development.
Question 87:
Answer: c) Small intestine and ascending colon
Explanation: The SMA arises from the abdominal aorta at the level of the L1 vertebra and primarily supplies the small intestine (jejunum and ileum) and the proximal part of the colon. Mnemonic: In My Room I’m In A Jail: Inferior Pancreaticoduodenal (anterior and posterior), Middle colic artery, Right colic artery, Ileocolic artery, Ileal arteries, Appendicular artery and Jejunal arteries.
A is incorrect as the stomach is primarily supplied by the left gastric artery (from the celiac trunk), and the spleen is primarily supplied by the splenic artery (also from the celiac trunk).
B is incorrect as the liver is primarily supplied by the hepatic artery (from the celiac trunk) and the gallbladder is primarily supplied by the cystic artery (a branch of the right hepatic artery).
D is incorrect as the kidneys are primarily supplied by the renal arteries (direct branches of the abdominal aorta), and the adrenal glands are primarily supplied by branches of the abdominal aorta (such as inferior phrenic, renal arteries and abdominal aorta to superior, middle, and inferior suprarenal arteries respectively) as well.
E is incorrect as the pancreas and duodenum receive their arterial supply from branches of the celiac trunk (such as the pancreaticoduodenal arteries) and the superior mesenteric artery (for the distal duodenum).
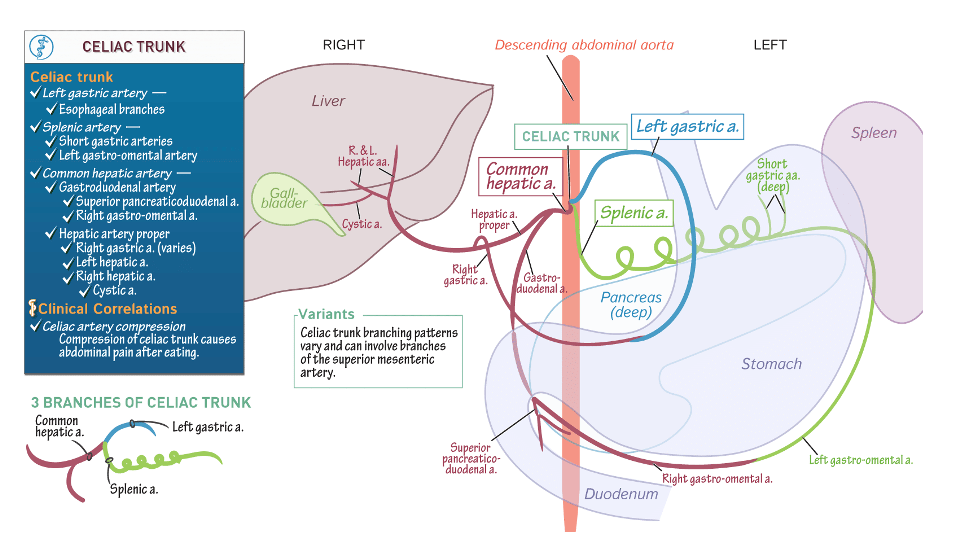
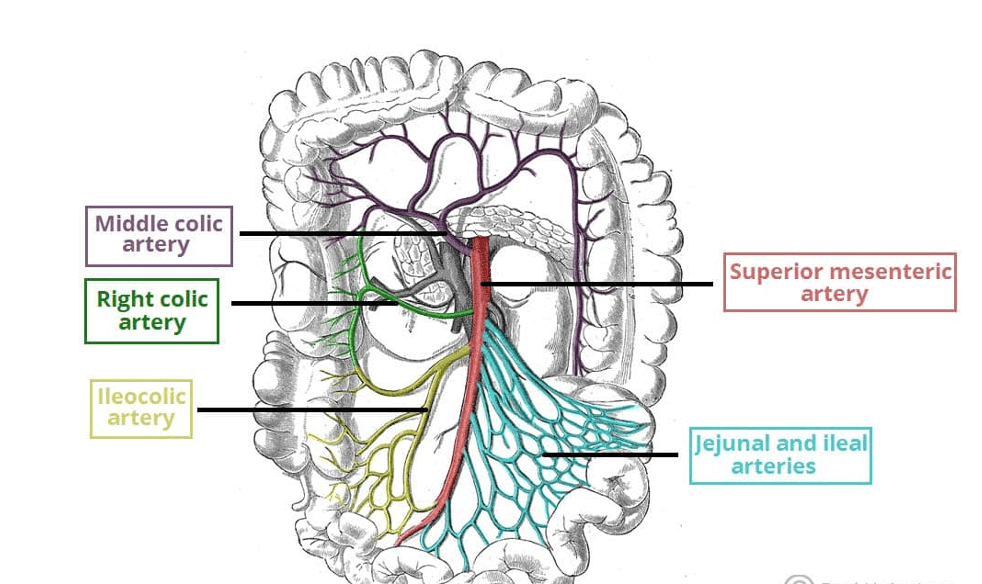
Question 88:
Answer: b) Left gastric artery, common hepatic artery, and splenic artery
Explanation: The Coeliac Trunk usually branches into the left gastric artery, common hepatic artery, and splenic artery, providing blood supply to various abdominal organs, including the stomach, liver, and spleen.
Question 89:
Answer: d) Oesophagus
Explanation: Portosystemic anastomoses can develop in various locations in the body, but one of the significant sites is in the oesophagus. These anastomoses, particularly in the lower part of the oesophagus, can lead to the formation of oesophageal varices, which are dilated blood vessels and can be clinically important in conditions associated with portal hypertension. Other sites for portosystemic anastomoses are rectum and anal canal as well as paraumbilical veins (abdomen).
Question 90:
Answer: e) Cisterna chyli
Explanation: The Cisterna chyli is a lymphatic structure located in the abdomen, serving as a storage reservoir for lymph. It collects lymph from the lower body and intestines before ultimately draining into the thoracic duct. Anything below the diaphragm drains into cisterna chyli whilst about the diaphragm drains into the thoracic duct.
Question 91:
Answer: c) They promote smooth muscle relaxation.
Explanation: Both NO and VIP are neurotransmitters that contribute to the relaxation of smooth muscle in the gastrointestinal tract. This relaxation is crucial for various GI functions, including facilitating the movement of food and contents through the digestive system. A is incorrect as smooth muscle contraction in the GI tract is typically stimulated by neurotransmitters like acetylcholine (ACh) and tachykinin.
Question 92:
Answer: d) Corpus
Explanation: The corpus of the stomach is the main region responsible for the secretion of gastric acid. It contains gastric glands that produce hydrochloric acid and pepsinogen, contributing to the digestive processes in the stomach.
A is incorrect as the pylorus is the narrowest part of the stomach, located near the junction with the small intestine (duodenum). It regulates the passage of chyme from the stomach into the duodenum and prevents backflow of it.
B is incorrect as the fundus is the upper part of the stomach that expands as it fills with food. It primarily serves as a temporary storage area for food and swallowed saliva before digestion begins in the rest of the stomach.
C is incorrect as the antrum is the lower part of the stomach, near the pyloric sphincter. It plays a role in mixing food with gastric juices and helps regulate the release of partially digested food (chyme) into the small intestine, it also contains the G cells which secrete gastrin and the d cells which secrete somatostatin.
E is incorrect as the cardia is the area surrounding the opening of the oesophagus into the stomach next to the lower oesophageal sphincter. Its main function is to prevent reflux of acidic stomach contents into the oesophagus. It contains glands that secrete mucus to protect the oesophagus from stomach acid.
Question 93:
Answer: d) When fats and proteins are detected in the small intestine.
Explanation: Cholecystokinin (CCK) is primarily released in response to the presence of fats and proteins in the small intestine. It stimulates the gallbladder to release bile and the acinar cells of the pancreas to secrete digestive enzymes, facilitating the digestion of these macronutrients.
Question 94:
Answer: d) Stimulator of acid secretion
Explanation: In the gastrointestinal tract, histamine primarily acts as a stimulator of acid secretion in the stomach. It is released from enterochromaffin-like (ECL) cells in response to various stimuli, such as gastrin or acetylcholine (ACh). It binds to H2 receptors on the surface of parietal cells in the stomach lining, triggering the release of gastric acid (hydrochloric acid). This acid secretion is essential for the digestion of food in the stomach.
A is incorrect as histamine can act as a vasodilator in other tissues, but in the context of the GI tract, its primary role is not vasodilation.
B is incorrect as histamine generally acts as a vasodilator rather than a vasoconstrictor.
C is incorrect as histamine H2 receptors on parietal cells stimulate acid secretion; they do not inhibit it.
E is incorrect as histamine can have some smooth muscle relaxing effects in certain contexts, its primary role in the GI tract is not as a muscle relaxant. Therefore, A and D are not the best answers.
Question 95:
Answer: a) CCK-2 receptors on parietal cells to stimulate acid secretion
Explanation: Gastrin primarily interacts with CCK-2 receptors (cholecystokinin type 2 receptors) located on chief cells and parietal cells in the stomach. These receptors mediate the effects of gastrin, including stimulating gastric acid secretion (parietal cells) and promoting the release of pepsinogen (chief cells) to aid in the digestive process which is then converted to pepsin due to the low pH of the stomach.
B is incorrect as H2 receptors are found on parietal cells and are involved in stimulating acid secretion, not on chief cells.
C is incorrect as ECL cells produce histamine in response to gastrin binding to CCK-2 receptors on parietal cells, which then stimulate acid secretion or gastrin binding to H2 receptors on ECL cells.
D is incorrect M3 receptors are cholinergic receptors involved in stimulating acid secretion, not inhibiting it and they are activated by Ach not gastrin either.
E is incorrect as D2 receptors are dopamine receptors and are not involved in regulating pepsinogen secretion by chief cells. D2 receptors are found on parietal cells in the gastric glands of the stomach. These receptors have an inhibitory effect on gastric acid secretion. When dopamine binds to D2 receptors on parietal cells, it decreases the production and release of hydrochloric acid (HCl).
Question 96:
Answer: d) They suppress the activity of the proton pump on parietal cells.
Explanation: Proton pump inhibitors (PPIs) work by suppressing the activity of the proton pump (H+/K+ ATPase) on parietal cells in the stomach lining. By inhibiting this pump, PPIs significantly reduce the secretion of gastric acid, helping to alleviate conditions associated with excess acid production, such as gastroesophageal reflux disease (GERD) and peptic ulcers.
A is incorrect as G cells secrete gastrin, which stimulates the release of histamine from ECL cells. Histamine then binds to H2 receptors on parietal cells, stimulating acid secretion, they have nothing to do with PPIs.
B is incorrect as D cells secrete somatostatin, which inhibits the release of gastrin from G cells and thus indirectly reduces acid secretion, but PPIs do not act directly on D cells.
C is incorrect as ECL cells release histamine in response to gastrin stimulation. Histamine then binds to H2 receptors on parietal cells, stimulating acid secretion. H2 receptor antagonists directly block H2 receptors on parietal cells to reduce acid secretion, but PPIs do not target ECL cells.
E is incorrect as chief cells secrete pepsinogen, which is converted to pepsin in the presence of acid. PPIs do not directly affect chief cells or their secretion of pepsinogen.
Question 97:
Answer: c) Ghrelin directly inhibits the firing of vagal afferent nerves.
Explanation: Ghrelin is produced in the stomach and acts on the hypothalamus to stimulate appetite and increase food intake. Ghrelin has been shown to directly inhibit the firing of vagal afferent nerves which play a crucial role in sensing nutrients and initiating the feeling of satiety. This inhibition can contribute to the sensation of hunger and the initiation of meal consumption. Ghrelin’s actions on the vagal afferent system are part of its complex role in regulating appetite and energy balance.
A is incorrect as Cholecystokinin (CCK) is a hormone involved in appetite regulation, but it is not directly stimulated by ghrelin, instead it stimulated by fats and proteins in the duodenum. Moreover, CCK typically acts to reduce appetite by signalling satiety, rather than inhibiting vagal afferent activity.
B is incorrect as ghrelin does not suppress the release of gastrin. Gastrin is involved in stimulating gastric acid secretion and motility, not vagal afferent nerve activity.
D is incorrect as leptin is an adipose tissue-derived hormone that acts to decrease appetite and regulate energy balance. Ghrelin increases appetite and food intake, but it does not increase leptin release.
Question 98:
Answer: a) Splanchnic nerves carry sensory information from abdominal organs to the central nervous system.
Explanation: Splanchnic nerves carry sensory information (afferent fibres) from abdominal organs to the central nervous system. This sensory information includes pain, distension, and other visceral sensations that are important for regulating autonomic functions and providing feedback to the brain.
B is incorrect as splanchnic nerves primarily consist of sympathetic fibres, not parasympathetic fibres. Parasympathetic innervation to the abdominal viscera is primarily provided by the vagus nerve and pelvic splanchnic nerves. This makes A the most correct and accurate answer.
C is incorrect because splanchnic nerves do not directly innervate skeletal muscles. They are associated with the autonomic nervous system, which controls involuntary functions of abdominal organs.
D is incorrect because splanchnic nerves regulate involuntary (autonomic) functions, not conscious motor functions.
E is incorrect because splanchnic nerves are part of the autonomic nervous system, not the somatic nervous system which innervates skeletal muscles.
Question 99:
Answer: c) GLP-1 triggers insulin secretion from pancreatic beta cells and inhibits food intake.
Explanation: GLP-1 is an incretin that is secreted by L cells in the small intestine that stimulates the release of insulin from pancreatic beta cells, which helps lower blood glucose levels. Additionally, it inhibits food intake by promoting a feeling of fullness (satiety), making it a key regulator of glucose metabolism and appetite.
A is incorrect as GLP-1 inhibits the secretion of glucagon from pancreatic alpha cells. Low blood glucose levels stimulate glucagon secretion from pancreatic alpha cells.
B is incorrect as GLP-1 does not promote glycogen breakdown in the liver; it promotes insulin secretion, which aids in glycogen synthesis. Glucagon and adrenaline stimulate glycogen breakdown in the liver.
D is incorrect as bile acids, micelles and pancreatic lipase are primarily responsible for the digestion and absorption of dietary fats.
E is incorrect as GLP-1 does not directly act on skeletal muscle to promote glucose uptake. Insulin stimulates glucose uptake in skeletal muscle by promoting the translocation of GLUT4 transporters to the cell surface. Therefore, this is not the best answer.
Question 100:
Answer: c) Hepatocyte
Explanation: Hepatocytes are the primary functional cells (parenchymal cells) of the liver. They perform numerous essential functions in the liver, including metabolism, detoxification, and the production of bile. Kupffer cells are liver-resident macrophages, stellate cells are involved in liver fibrosis, endothelial cells line blood vessels.
Question 101:
Answer: c) Stercobilin
Explanation: Stercobilin is a breakdown product of bilirubin which is converted to urobilinogen, formed in the intestines by the action of bacteria. It gives stool its characteristic brown colour. Bilirubin, urobilinogen, and melanin are also involved in coloration processes, but stercobilin is the primary contributor to the brown colour of stool. Cholecystokinin, on the other hand, is a hormone involved in the regulation of pancreatic enzyme secretion and gallbladder contraction, unrelated to stool colour.
Bilirubin is a yellow compound that breaks down haeme in red blood cells. Bilirubin is processed in the liver and then secreted into bile.
Urobilinogen is a colourless byproduct formed in the intestines from bilirubin. Some urobilinogen is reabsorbed, converted to urobilin which is excreted in urine, contributing to its yellow colour.
Melanin is a pigment is responsible for the colour of skin, hair, and eyes, and is not involved in stool coloration.
CCK is a hormone that stimulates the digestion of fat and protein by promoting the secretion of digestive enzymes from acinar cells in the pancreas, but it does not contribute to the colour of stool.
Question 102:
Answer: c) Bile salts
Explanation: Bile salts are amphipathic molecules that form the core of micelles. They have both hydrophilic and hydrophobic regions, allowing them to surround and solubilize lipids, such as fatty acids and fat-soluble vitamins, in the aqueous environment of the small intestine. This formation of micelles enhances the absorption of lipids by increasing their surface area for interaction with the absorptive epithelial cells.
A is incorrect as this enzyme is involved in steroid metabolism, converting testosterone to dihydrotestosterone (DHT). It is not related to the formation of micelles.
B is incorrect as triglycerides are the primary form of stored fat in the body and are broken down into fatty acids and monoglycerides for absorption which is facilitated by micelles. They are not involved in micelle formation; micelles are what facilitates their absorption.
D is incorrect as chylomicrons are lipoprotein that transport absorbed triglycerides from the intestinal cells to other parts of the body. They form after micelles have delivered the lipids into the enterocytes.
E is incorrect as fatty acids are absorbed into enterocytes after micelles deliver them to the intestinal epithelium. While fatty acids can be part of the micelle content, they are not the core-forming molecule. Therefore, the best answer is C.
Question 104:
Answer: c) Enterohepatic circulation
Explanation: Enterohepatic circulation is the process in which bile acids are absorbed in the ileum, transported to the liver via the portal vein, and then secreted into bile. This recycling mechanism is essential for the efficient digestion and absorption of dietary lipids. Options a, b, d, and e do not accurately describe this process.
Question 105:
Answer: c) Bilirubin
Explanation: Jaundice is characterized by the yellowing of the skin and eyes due to the excess accumulation of bilirubin, a pigment derived from the breakdown of haemoglobin. Options a, b, d, and e are not the primary pigments associated with jaundice.
Question 106:
Answer: a) Glucose and galactose
Explanation: Lactose is broken down into glucose and galactose by the enzyme lactase during the process of digestion. Options b, c, d, and e involve different sugars and enzymatic processes.
B is incorrect as fructose and glucose are the monosaccharides that result from the breakdown of sucrose, not lactose.
C is incorrect as sucrose and maltose are disaccharides themselves. Sucrose breaks down into glucose and fructose, and maltose breaks down into two glucose molecules.
D is incorrect as lactase is the enzyme that breaks down lactose into glucose and galactose.
Question 107:
Answer: e) Sodium and glucose
Explanation: Oral rehydration tablets typically contain sodium and glucose, which work together to restore electrolyte balance and facilitate fluid absorption in cases of dehydration, particularly due to diarrhoea. Options a, b, c, and d do not represent the primary components of oral rehydration tablets.
Question 107:
Answer: c) pH 7-9
Explanation: Trypsin exhibits its maximum enzymatic activity in the pH range of 7-8 within the human digestive system. This pH range is typically found in the duodenum, where trypsin plays a significant role in the digestion of proteins. Options a, b, d, and e represent pH ranges that are less optimal for trypsin activity.
A is incorrect as this pH range is optimal for the enzyme pepsin, which is active in the stomach. Trypsin, however, operates in the small intestine where the environment is less acidic.
B is incorrect as this pH range is too acidic for trypsin’s optimal activity. Trypsin requires a more neutral to slightly alkaline environment to function effectively.
D is incorrect as this pH range is slightly higher than the optimal range for trypsin. Although trypsin can still be active at this pH, its maximum activity is typically at a slightly lower pH.
E is incorrect as this pH range is highly alkaline and not conducive to trypsin activity. At such a high pH, trypsin would likely be denatured and inactive.

Question 108:
Answer: b) Vitamin D
Explanation: Vitamin D is not passively transported across the intestinal membrane but, like vitamin C (water-soluble), requires specific transport mechanisms for absorption. This distinction is essential in understanding the absorption of different vitamins in the gastrointestinal tract. The question is asking about a fat-soluble vitamin that isn’t passively transported, Vitamin C is not fat soluble and is therefore immediately the incorrect answer and out of the other options Vitamin D is the only fat soluble vitamin that requires active transport into enterocytes.
Question 109:
Answer: c) Maintenance of healthy skin and vision
Explanation: Vitamin A is essential for maintaining healthy skin and vision. It plays a critical role in the formation of visual pigments in the retina and helps prevent night blindness. Additionally, it supports skin health and integrity. While vitamin A has other functions in the body, such as immune system support, its role in skin and vision is particularly significant.
A is incorrect as this function is primarily associated with Vitamin K. Vitamin K is crucial for synthesizing proteins required for blood clotting (coagulation) and wound healing. It helps in the formation of prothrombin, which is essential for the clotting process.
B is incorrect as this function is primarily associated with Vitamin C and Vitamin E. Vitamin C is a potent antioxidant that helps protect cells from damage by free radicals and boosts the immune system. Vitamin E also acts as an antioxidant, protecting cell membranes from oxidative damage.
D is incorrect as these functions are primarily associated with Calcium and Potassium. Calcium ions are critical for muscle contractions and neurotransmitter release in nerve cells. Potassium is also crucial for proper muscle function and nerve transmission, maintaining the electrical charge in cells.
E is incorrect as this function is primarily associated with Vitamin D. Vitamin D promotes calcium absorption in the gut and maintains adequate serum calcium and phosphate concentrations, which is necessary for bone health.
Question 110:
Answer: b) Duodenum
Explanation: Most of the iron absorption occurs in the duodenum, the first part of the small intestine. This is where dietary iron is actively absorbed into the bloodstream. The stomach also plays a role in iron absorption by converting some of the dietary iron into a form that is more easily absorbed in the duodenum. The jejunum and ileum are also parts of the small intestine but are not the primary sites of iron absorption. Iron absorption does not occur in the colon.
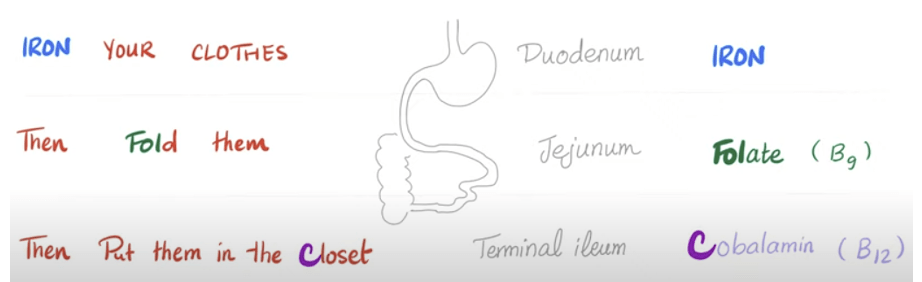
Question 111:
Answer: c) Paracellular transport
Explanation: Paracellular transport refers to the movement of substances through the tight junctions between adjacent epithelial cells in the gastrointestinal tract. This mode of transport allows certain ions and small molecules to pass between cells and enter the bloodstream. It is an essential mechanism for nutrient absorption and maintaining intestinal barrier function.
A is incorrect as it involves the movement of substances through the epithelial cells themselves, passing across the apical and basolateral membranes.
B is incorrect as this describes the movement of substances within a single cell, not between cells.
Question 112:
Answer: c) Reduced mixing of digestive enzymes with food
Explanation: Increased gut motility can lead to reduced mixing of digestive enzymes with food, potentially resulting in incomplete digestion and absorption. This can occur in conditions such as rapid transit through the digestive tract.
A is incorrect as increased gut motility typically results in decreased nutrient absorption because the food moves too quickly through the digestive tract, reducing the time available for absorption.
B is incorrect as increased gut motility leads to faster transit time of food through the digestive tract.
D is incorrect as increased gut motility often increases the risk of diarrhoea because the rapid movement of food through the intestines reduces the absorption of water, leading to watery stools.
E is incorrect as increased gut motility usually decreases water absorption because the food passes through the colon too quickly, not allowing sufficient time for water reabsorption.
Question 113:
Answer: a) To dilute hypertonic solutions in the lumen
Explanation: One of the primary functions of intestinal secretion is to release fluids into the intestinal lumen to dilute hypertonic solutions and maintain appropriate osmotic balance.
Question 114:
Answer: a) G protein-coupled receptors (GPCR)
Explanation: Acetylcholine primarily binds to cholinergic receptors, which belong to the G protein-coupled receptor (GPCR) family, when mediating its effects in the gastrointestinal tract. Options b, c, d, and e represent other receptor families that are not the primary targets of Ach in this context.
B is incorrect as these receptors are typically used by growth factors such as insulin, epidermal growth factor (EGF), and platelet-derived growth factor (PDGF). When these ligands bind to the receptor, the receptors dimerize, leading to phosphorylation of specific tyrosine residues on the receptor itself and downstream signalling proteins.
C is incorrect as these receptors are used by steroid hormones such as cortisol, oestrogen, testosterone, and thyroid hormones. These ligands cross the cell membrane and bind to their receptors in the cytoplasm or nucleus, resulting in changes in gene expression.
E is incorrect as these receptors are part of the innate immune system and are involved in recognizing pathogen-associated molecular patterns (PAMPs). They play a crucial role in activating immune responses to bacterial, viral, and fungal infections.
Question 115:
Answer: a) Activation of adenylate cyclase
Explanation: Cholera toxin activates adenylate cyclase in intestinal cells, leading to an increase in cyclic AMP (cAMP) levels. Elevated cAMP levels subsequently activate protein kinase A (PKA), which phosphorylates and opens chloride channels in the cell membrane, resulting in the uncontrolled secretion of chloride ions (Cl-) into the intestinal lumen. This chloride secretion disrupts electrolyte balance and leads to watery diarrhoea.
Question 116:
Answer: e) Decreased gastric acid secretion
Explanation: Medications that block H2 histamine receptors in the GI system, like ranitidine, are primarily used to decrease gastric acid secretion. This reduction in gastric acid production is beneficial in treating conditions such as gastroesophageal reflux disease (GERD) and peptic ulcers.
Question 117:
Answer: b) They are all involved in the modulation of gastric acid secretion.
Explanation: Prostaglandins specifically, prostaglandin E2 (PGE2), have a regulatory role, balancing the secretion of mucus and bicarbonate to protect the stomach lining while also influencing acid secretion indirectly. Acetylcholine (Ach) acts on muscarinic receptors (M3) on parietal cells to directly stimulate the secretion of gastric acid. Gastrin secreted by G cells in response to food, gastrin acts on parietal cells (CCK-B and CCK-2) and stimulates ECL cells (H2) to release histamine, both of which enhance gastric acid secretion. Histamine released by ECL cells in response to acetylcholine and gastrin, histamine binds to H2 receptors on parietal cells, significantly increasing the production of gastric acid.
A is incorrect as these molecules are not involved in nutrient absorption. Their primary roles are in the regulation of secretion and motility rather than direct absorption.
C is incorrect as none of these molecules inhibit the release of pancreatic enzymes. They are more focused on the stomach’s functions, particularly acid secretion.
D is incorrect as although acetylcholine is involved in stimulating peristalsis, the primary roles of prostaglandins, gastrin, and histamine are not directly related to initiating peristalsis. Their main function is related to gastric acid secretion.
E is incorrect as bile secretion is primarily regulated by other hormones such as cholecystokinin (CCK).
**Question 118:**
**Answer: A) Acetylcholine**
**Explanation:** Acetylcholine is the primary neurotransmitter responsible for initiating peristalsis in the esophagus during the oral phase of swallowing. It acts on the smooth muscle of the esophagus, leading to a coordinated contraction and relaxation sequence, propelling the food bolus downwards. Serotonin, dopamine, norepinephrine, and GABA are not the primary neurotransmitters involved in this process. Serotonin (5-HT) detects distension arounds the bolus in the oesophagus which sends signals to the nodose ganglion in the brain stem stimulating the vagus nerve. Dopamine is not really involved in the GI tract however it can influence the gut-brain axis. Norepinephrine (noradrenaline) acts as a neurotransmitter and is involved in sympathetic nervous system control. In the gastrointestinal tract including the oesophagus, it generally inhibits smooth muscle contraction and slows down motility. GABA is primarily an inhibitory neurotransmitter in the central nervous system. In the gastrointestinal tract, it can modulate enteric nervous system activity, influencing smooth muscle relaxation and gut motility under certain conditions including in the oesophagus.
**Question 119:**
**Answer: A) Epiglottis**
**Explanation:** The epiglottis is a flap-like structure that covers the trachea during the pharyngeal phase of swallowing, preventing food from entering the airway. The thyroid gland, cricoid cartilage, hyoid bone, and vocal cords are involved in other functions but do not play a direct role in preventing aspiration during swallowing.
**Question 120:**
**Answer: D) Motilin**
**Explanation:** Motilin is primarily responsible for initiating the migrating motor complex (MMC) in the fasting state of the intestinal tract. MMC helps to clear undigested material and maintain motility during fasting. Insulin, glucagon, cholecystokinin (CCK), and leptin are hormones that play different roles in metabolism and digestion but do not initiate MMC.
**Question 121:**
**Answer: D) Propelling faecal material**
**Explanation:** Haustrations in the large intestine are responsible for the segmental contraction and relaxation of the colon, aiding in the mixing and propelling of faecal material forward for further processing and absorption. Propelling chyme occurs due to peristalsis. Storage of faeces and formation of faecal pellets occur in the rectum and sigmoid colon.
Peristalsis is the coordinated contraction and relaxation of longitudinal and circular muscles that propels chyme (partially digested food) through the digestive tract, it ensures the forward movement of food along the entire length of the digestive tract, from the oesophagus to the rectum and links to answer C.
Segmentation is the alternating contractions and relaxations of circular muscles in the small intestine. This process divides the intestinal contents into segments and mixes them thoroughly with digestive enzymes and bile for optimal nutrient absorption and is linked to answer B.
Retropulsion is the backward movement of food in the stomach caused by contractions of the stomach muscles. This movement helps to mix food with gastric juices and break it down into smaller particles and links to answer A.
**Question 122:**
**Answer: C) Ano-rectum**
**Explanation:** The ano-rectum is the component of the gastrointestinal tract responsible for voluntary control over defecation. The external anal sphincter, which surrounds the ano-rectal junction, can be voluntarily contracted and relaxed to control the release of feces. The small intestine, large intestine, duodenum, and cecum do not have direct control over defecation.
**Question 123:**
**Answer: B) Nitric oxide**
**Explanation:** Nitric oxide is the neurotransmitter that plays a key role in relaxing the lower esophageal sphincter (LES) to allow food to pass into the stomach during the swallowing process. The relaxation of the LES is crucial to prevent obstruction and facilitate food entry. Serotonin, epinephrine, glutamate, and substance P are not primarily responsible for LES relaxation.
**Question 124:**
**Answer: C) Clearing undigested material**
**Explanation:** In the fasted state, the primary function of the small intestine’s migrating motor complex (MMC) is to clear undigested material and maintain motility. This helps prevent bacterial overgrowth and keeps the intestine clean for subsequent digestion and absorption. The other options are not the primary function of MMC.
**Question 125:**
**Answer: C) Propelling faecal material over long distances**
**Explanation:** Mass movements in the large intestine are characterized by strong, propulsive contractions that move faecal material over long distances, typically from the transverse colon to the rectum. They are responsible for the urge to defecate. The other options are not characteristics of mass movements.
**Question 126:**
**Answer: E) Sigmoid colon**
**Explanation:** The sigmoid colon acts as a reservoir for faeces and allows for the storage of stool until defecation. It is the last part of the large intestine before the rectum and is responsible for the temporary storage of faecal material. The other options do not serve this specific function.
**Question 127:**
**Answer: C) Relaxing to allow the passage of stool**
**Explanation:** The primary function of the external anal sphincter in defecation is to relax, allowing the passage of stool from the rectum through the anus. This sphincter is under voluntary control and must relax for defecation to occur. The other options are not the primary function of the external anal sphincter.
E is incorrect as this describes the function of the internal anal sphincter rather than the external anal sphincter.
**Question 128:**
**Answer: A) Receptive relaxation for efficient food intake**
**Explanation:** The proximal stomach exhibits receptive relaxation, allowing it to relax in response to food entry, facilitating efficient food intake. This relaxation is important for accommodating a meal. Gastric accommodation is correct however it primarily relates to the fundus and body of the stomach which is more distal than proximal. Propulsion, grinding, and retropulsion are more characteristic of the distal stomach’s motility.
**Question 129:**
**Answer: C) Intrinsic factor**
**Explanation:** Intrinsic factor, a component of gastric secretions, is essential for the absorption of vitamin B12 in the ileum. It forms a complex with vitamin B12, allowing its absorption in the ileum. Pepsinogen, gastric acid, protein, and haptocorrin (R-factors) have other functions in the digestive process.
Proteins is incorrect as Vitamin B12 enters the body bound to proteins in our food however it has no influence on the absorption of cobalamin (vitamin B12) in the ileum.
Haptocorrin (R-factor) is incorrect as it is needed to protect vitamin B12 from the acidic pH of the stomach, which does mean that it is in the correct form to be absorbed in the ileum however this is not the best answer.
**Question 130:**
**Answer: B) Parietal cells**
**Explanation:** Parietal cells are primarily responsible for secreting gastric acid in the stomach. They contain proton pumps that actively transport hydrogen ions into the stomach lumen. Chief cells secrete pepsinogen, mucous neck cells produce mucus, G cells secrete gastrin, and D cells release somatostatin.
Chief cells are responsible for secreting pepsinogen (a zymogen) which is activated by the low pH of the stomach into pepsin which is involved in the digestion of proteins.
Mucous neck cell is the incorrect answer as it secretes mucus, which helps protect the lining of the stomach from the corrosive effects of gastric acid and digestive enzymes.
G cells stimulate the release of gastrin which binds to parietal cells to stimulate the secretion of HCl, but it is not the G cell that secretes the acid.
D cells is incorrect as this is responsible for secreting somatostatin a hormone that inhibits the secretion of gastric acid.
**Question 131:**
**Answer: B) Gastric phase**
**Explanation:** The gastric phase of gastric secretion is characterized by the release of gastrin, which stimulates gastric acid production in response to partially digested food entering the stomach. The cephalic phase is triggered by sensory stimuli, the intestinal phase occurs in the duodenum, and the pyloric and enteric phases are not typical phases of gastric secretion.
**Question 132:**
**Answer: A) Gastric ulcers**
**Explanation:** Hyper-acid secretion in the stomach is often associated with gastric ulcers, which can be exacerbated by Helicobacter pylori infection. H. pylori is a bacterium that can infect the stomach lining and contribute to the development of ulcers. Various mechanisms of gastric acid blockade, including proton pump inhibitors and H2-receptor antagonists, are used to manage hyper-acid secretion and ulceration.
**Question 133:**
**Answer: C) Intestinal phase**
**Explanation:** The intestinal phase of gastric secretion primarily involves the release of secretin and cholecystokinin (CCK), which inhibit gastric acid secretion and promote pancreatic enzyme secretion to aid in digestion in the small intestine. The other phases have different functions in gastric secretion.
**Question 134:**
**Answer: E) Gastric lipases**
**Explanation:** Gastric lipases, present in gastric secretions, are responsible for breaking down dietary triglycerides into fatty acids and glycerol in the stomach. Pepsinogen is a precursor of pepsin, gastric acid aids in protein digestion, intrinsic factor is involved in vitamin B12 absorption, and mucus provides protection and lubrication.
**Question 135:**
**Answer: D) Bicarbonate secretion**
**Explanation:** The cellular mechanism of bicarbonate secretion in the gastric parietal cells involves the exchange of bicarbonate ions for chloride ions to keep the charges balanced across the epithelial cells. This process helps maintain the stomach’s pH balance. Proton pump activation, hydrochloric acid production, and acidic protease release are other aspects of gastric acid secretion regulation.
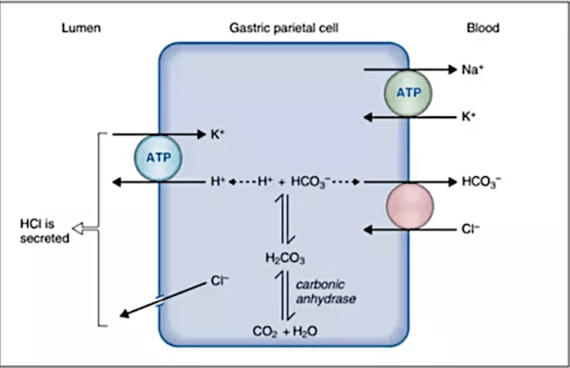
**Question 136:**
**Answer: A) Cephalic phase**
**Explanation:** The cephalic phase of gastric secretion is initiated by sensory stimuli, such as the sight, smell, or taste of food. It involves vagal stimulation leading to the release of gastrin, which prepares the stomach for food entry. The other phases are triggered by different factors and have distinct functions.
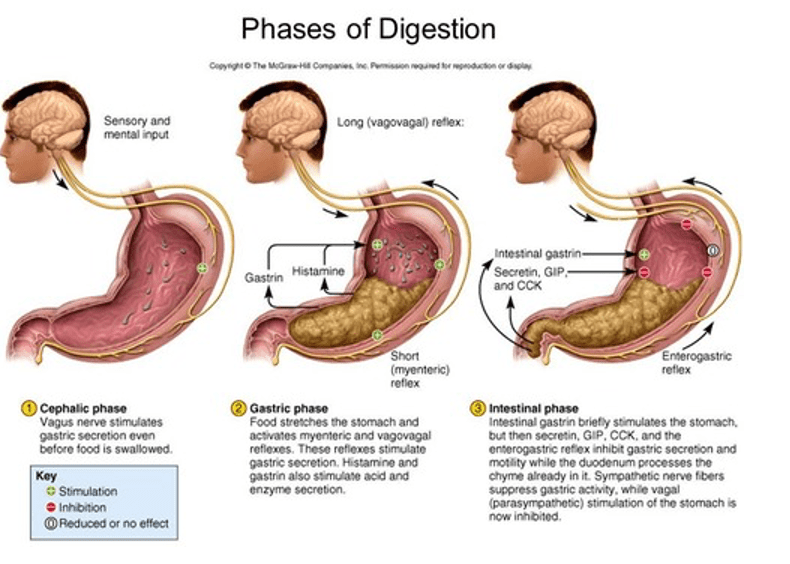
**Question 137:**
**Answer: D) Disrupting the gastric mucosal barrier**
**Explanation:** In the context of hyper-acid secretion, Helicobacter pylori primarily disrupts the gastric mucosal barrier, making the stomach lining more susceptible to damage from gastric acid. This bacterium is a common cause of gastric ulcers and can lead to various gastric diseases. It does not stimulate mucus production, inhibit acid secretion, or directly protect the stomach lining.
**Question 139:**
**Answer: D) Gallbladder**
**Explanation:** Bile is primarily stored in the gallbladder before its release into the duodenum. The gallbladder acts as a reservoir for bile, which is produced in the liver and transported to the gallbladder for storage and concentration.
**Question 140:**
**Answer: D) Cholecystokinin (CCK)**
**Explanation:** Cholecystokinin (CCK) is the hormone that stimulates gallbladder contraction and the relaxation of the sphincter of Oddi in response to the presence of food in the duodenum. It promotes the release of bile into the duodenum for digestion. Secretin stimulates ductal cells of the pancreas to secrete bicarbonate to neutralise the acidic chyme from the stomach that has just entered the duodenum.
**Question 141:**
**Answer: C) Recycling bile salts for reuse**
**Explanation:** The primary function of the enterohepatic circulation of bile salts is to recycle bile salts for reuse. Bile salts are absorbed in the ileum and transported back to the liver to be incorporated into newly synthesized bile, thus conserving these essential components for digestion.
**Question 142:**
**Answer: C) By forming a hydrophilic shell around lipid particles**
**Explanation:** Bile salts aid in solubilizing products of lipid digestion in mixed micelles by forming a hydrophilic (water-attracting) shell around lipid particles. This allows the lipids to remain in suspension in the aqueous environment of the small intestine, facilitating their absorption.
A is incorrect as this function is primarily carried out by pancreatic lipases, not bile salts. Lipases hydrolyse triglycerides into free fatty acids and monoglycerides.
B is incorrect as although bile salts do emulsify large fat droplets into smaller ones, this process occurs before the formation of mixed micelles and helps to increase the surface area for the action of lipases. However, the specific role of bile salts in solubilizing lipid digestion products in mixed micelles is better described by forming a hydrophilic shell.
**Question 143:**
**Answer: C) Altered bilirubin metabolism**
**Explanation:** One of the basic causes of jaundice is altered bilirubin metabolism. Jaundice results from the accumulation of bilirubin, a yellow pigment, in the body due to various factors, including liver dysfunction, haemolysis of red blood cells, or biliary obstruction.
**Question 144:**
**Answer: C) Bacterial overgrowth**
**Explanation:** When the mucosal barrier fails to protect the gut, one of the consequences can be bacterial overgrowth. This can lead to dysbiosis and increased susceptibility to infections and inflammatory conditions in the gastrointestinal tract.
**Question 145:**
**Answer: C) Mucus-bicarbonate layer**
**Explanation:** The mucus-bicarbonate layer is responsible for producing a thick, viscous layer that protects the epithelial cells of the stomach from the corrosive effects of acid and digestive enzymes. Prostaglandins, hydrochloric acid, gastrin, and pepsin have other roles in the gastrointestinal tract. Prostaglandins play a role in maintaining the integrity of the mucosal barrier by stimulating mucus and bicarbonate secretion and enhancing blood flow to the stomach lining. However, they do not form the physical mucus-bicarbonate layer.
**Question 146:**
**Answer: D) Regulating inflammatory responses**
**Explanation:** Prostaglandins play a primary role in regulating inflammatory responses in the gastrointestinal tract. They can have both protective and inflammatory effects, helping to maintain the mucosal barrier and modulate immune responses.
B is incorrect as prostaglandins have an inhibitory effect on gastric acid secretion. They help protect the stomach lining by reducing acid production.
C is incorrect as although prostaglandins can modulate immune responses, their primary role in the GI tract is related to inflammatory regulation and mucosal protection rather than directly stimulating immune cell activity.
E is incorrect as prostaglandins stimulate the production of mucus in the GI tract, which helps protect the mucosal lining from damage.
**Question 147:**
**Answer: B) Proliferation of epithelial cells
**Explanation:** Epithelial cells in the GI tract have a high turnover rate and are capable of rapid proliferation to replace damaged cells. This process helps to maintain the protective barrier function of the GI epithelium and prevents further damage from luminal contents. This is crucial for repairing the damaged epithelium and restoring its integrity.
A is incorrect as the focus initially is on repairing the damage rather than enhancing nutrient absorption.
C is partially correct as apoptosis may occur in severely damaged cells as part of the healing process, but it is not the initial response. The body first attempts to repair and replace damaged cells before resorting to cell death mechanisms. It is like the cell cycle whereby the checkpoints stop the cells and try to repair the damage, if it is not repairable then apoptosis occurs as a last resort. Therefore, this isn’t the best answer.
D is incorrect as decreased cell migration would hinder the repair process rather than facilitate it. Increased cell migration is necessary for covering the injured area and restoring the epithelial barrier.
E is partially correct although increased mucus secretion can be part of the protective response, it is not universally the first response to injury throughout the entire GI tract. It is more specific to the stomach and certain parts of the intestine, shielding the epithelial cells from further harm by gastric acid. Therefore, again this is not the best answer.
**Question 148:**
**Answer: C) Restitution**
**Explanation:** Restitution is the process that involves the replacement of injured or lost gastrointestinal epithelial cells by adjacent healthy cells to restore the integrity of the mucosal barrier. It is an essential part of the healing response to gut injury. It involves vagal efferent nerves release nitric oxide (NO) and calcitonin gene-related peptide (CGRP), which cause local vasodilation (increased blood flow) and hyperaemia (increased blood volume in vessels) to remove the acid and aid in tissue repair. Inflammatory stimuli trigger the production of prostaglandins by the enzyme cyclooxygenase-2 (COX2). Prostaglandins promote various responses including cell migration, motility of cells to the site of injury, and increased blood flow (vasodilation). Gastrin, not only stimulate parietal cells to produce HCl, in the context of restitution is enhances motility of the GI tract and stimulates the production of growth factors such as Epidermal Growth Factor (EGF) and Transforming Growth Factor Beta (TGFB), which are important for tissue repair and regeneration. Trefoil peptides are proteins found in mucus secretions they stimulate cell motility and migration of cells to the areas of damage, aiding in the repair process. Regenerating proteins (REG) are released from enterochromaffin-like (ECL) cells and enteroendocrine cells near the site of injury. They play a role in organizing the epithelial cells, ensuring they are correctly positioned and functional during the repair process.
**Question 149:**
**Answer: A) Hepatocytes**
**Explanation:** Hepatocytes are the primary liver cells responsible for the synthesis of proteins, including albumin and clotting factors. They play a crucial role in maintaining protein homeostasis in the body.
B is incorrect as Kupffer cells are specialized macrophages located in the liver sinusoids and are involved in phagocytosis and immune responses, not protein synthesis.
C is incorrect as stellate cells are involved in storing vitamin A and producing extracellular matrix components during liver injury and fibrosis, not protein synthesis.
D is incorrect as endothelial cells line the blood vessels within the liver and are involved in regulating blood flow and exchange between blood and liver tissue, not protein synthesis.
**Question 150:**
**Answer: B) Kupffer cells**
**Explanation:** Kupffer cells are specialized macrophages located in the liver sinusoids. They are responsible for phagocytosing pathogens and debris, contributing to the liver’s immune function.
**Question 151:**
**Answer: C) Stellate (Ito) cells**
**Explanation:** Stellate (Ito) cells are liver cells responsible for storing vitamin A and can become activated in liver fibrosis and cirrhosis, contributing to the pathogenesis of these conditions.
**Question 152:**
**Answer: D) Synthesis of plasma proteins**
**Explanation:** The main function of the liver related to the synthesis of proteins is the production of plasma proteins, including albumin and clotting factors. These proteins are essential for maintaining normal blood composition and coagulation.
A is incorrect as although the liver is involved in carbohydrate metabolism (glycogen storage, gluconeogenesis), this is not directly related to protein synthesis.
B is incorrect as although the liver does store vitamins A, D, E, and K this function is not directly related to protein synthesis.
C is incorrect as although the liver plays a major role in detoxifying drugs and other xenobiotics, but this is unrelated to its role in protein synthesis.
E is incorrect as the liver does not have a primary role in regulating blood pressure; this function is mainly controlled by the kidneys and cardiovascular system.
**Question 153:**
**Answer: D) Cytochrome P450 2E1 (CYP2E1)**
**Explanation:** Cytochrome P450 2E1 (CYP2E1) is a liver enzyme primarily responsible for the metabolism of alcohol (ethanol), converting it into acetaldehyde. This enzyme plays a key role in the breakdown of alcohol in the liver.
Question 154:
Answer: C. Chenodeoxycholic
Explanation: Chenodeoxycholic acid is a primary bile acid synthesised in the liver from cholesterol, the other primary bile acid is cholic acid.
A. Deoxycholic acid and B. lithocholic acid are incorrect as they secondary bile acids formed by bacterial action in the intestine not primary bile acids.
D. Glycine and E. Taurine are incorrect as they are both amino acids involved in the conjugation of bile acids to form bile salts but they are not bile acids themselves.
Question 155:
Answer: B. Glucuronyl transferase
Explanation: Glucuronyl transferase conjugates bilirubin in the liver, making it water-soluble for excretion.
A. Lipase is incorrect as lipase is an enzyme that breaks down fats
C. amylase is incorrect as it is an enzyme that breaks down carbohydrates
D. pepsin is incorrect as it is an enzyme that breaks down proteins in the stomach
E. lactase is incorrect as it is an enzyme that breaks down lactose.
Question 156:
Answer: A. Cholic acid
Explanation: Cholic acid is a primary bile acid that is converted to the secondary bile acid deoxycholic acid by intestinal bacteria.
B is incorrect as although Chenodeoxycholic acid is a primary bile acid, it is either converted to lithocholic acid or ursodeoxycholic acid which are secondary bile acids making C. and E. incorrect.
E. is incorrect as taurocholic acid is a conjugated form of cholic acid.
Question 157:
Answer: C. Neutralisation of stomach acid
Explanation: Bile acids emulsify dietary fats allowing them to aggregate withing micelles, facilitate the absorption of fat-soluble vitamins (A, D, E, K), aid in the elimination of cholesterol since bile acids are made from cholesterol, and activate pancreatic lipase for fat digestion.
C. is the correct answer as bile acids do not neutralise stomach acid; this function is performed by bicarbonate secreted by ductal cells of the pancreas. Bile acids emulsify dietary fats, facilitate the absorption of fat-soluble vitamins (A, D, E, K), aid in the elimination of cholesterol, and activate pancreatic lipase for fat digestion.
Question 158:
Answer: D. Reabsorption in the colon
Explanation: Bile acids are primarily reabsorbed in the terminal ileum, not the colon. In the liver, cholesterol is converted into primary bile acids: cholic acid and chenodeoxycholic acid, through a series of enzymatic reactions. The rate-limiting step in this process is catalysed by the enzyme cholesterol 7α-hydroxylase (CYP7A1 an enzyme located in the endoplasmic reticulum of the liver). These primary bile acids are then conjugated with amino acids, glycine, or taurine, to form bile salts. This increases the solubility of bile acids, making them more effective in the digestive process. Bile produced by the liver is transported through bile ducts to the gallbladder, where it is stored and concentrated. When food, especially fatty food, enters the duodenum, it stimulates the release of the hormone cholecystokinin (CCK) from the enteroendocrine cells (I cells) of the duodenum. CCK causes the gallbladder to contract and release bile through the common bile duct into the duodenum. In the duodenum, bile salts emulsify dietary fats, breaking them down into smaller droplets. This increases the surface area for pancreatic lipase to act upon, aiding in the digestion of fats. Bile salts also form micelles, which are tiny aggregates that encapsulate fatty acids and monoglycerides, making them soluble in the aqueous environment of the intestine and facilitating their absorption into the intestinal cells. About 95% of bile salts are reabsorbed in the last 80cm of the ileum. These reabsorbed bile salts enter the portal circulation and are transported back to the liver via the portal vein, conserving the body’s resources. The synthesis of new bile acids is tightly regulated by a feedback mechanism involving the farnesoid X receptor (FXR). When bile acids are abundant, FXR inhibits cholesterol 7α-hydroxylase (CYP7A1), reducing the synthesis of new bile acids.
Question 159:
Answer: B. Kidney
Explanation: The kidney converts Vitamin D to its active form, calcitriol.
A. liver is incorrect as it is involved in the initial hydroxylation of Vitamin D to calcidiol (25 hydroxy Vitamin D) by enzyme 25 hydroxylase.
C. the skin is incorrect as it synthesises 7- dehydrocholesterol which is then converted to pre–Vitamin D and then cholecalciferol upon UV exposure which are not the active forms of Vitamin D.
D. is incorrect as the intestine absorbs dietary Vitamin D and isn’t responsible in any of the synthesis.
E. is incorrect as the pancreas is not involved in Vitamin D metabolism either.

Question 160:
Answer: D. Lithocholic acid
Explanation: Lithocholic acid is a secondary bile acid formed from chenodeoxycholic acid.
A. is incorrect as Cholic acid is a primary bile acid not a secondary bile acid
B. is incorrect as deoxycholic acid is a secondary bile acid derived from cholic acid
C. is incorrect as ursodeoxycholic acid is a secondary bile acid but not directly formed from chenodeoxycholic acid
E. is incorrect as taurocholic acid is a conjugated form of cholic acid.
Question 161:
Answer: C. CYP7A1
Explanation: CYP7A1 (cholesterol 7 alpha-hydroxylase) catalyses the rate-limiting step in bile acid synthesis, converting cholesterol to 7-alpha-hydroxycholesterol. CYP1A1, CYP2D6, CYP3A4, and CYP2C19 are involved in different metabolic pathways and are not the primary enzymes in bile acid synthesis.
Question 162:
Answer: C. Enterohepatic circulation
Explanation: Enterohepatic circulation is the process that recycles bile acids from the intestine back to the liver.
A. and B. are incorrect as glucuronidation, and sulfation are processes of conjugation that increase solubility of compounds for excretion such as drugs and hormones.
D. is incorrect as deconjugation occurs in the intestine by bacteria where gut bacteria produce enzymes (like bile salt hydrolases) that remove glycine or taurine from conjugated bile acids. Deconjugated bile acids can then be reabsorbed or further metabolized into secondary bile acids.
E. is incorrect as transamination is crucial in amino acid metabolism and the synthesis of non-essential amino acids.
Question 163:
Answer: E. Acetyl-CoA
Explanation: Acetyl-CoA is involved in fatty acid and cholesterol metabolism but not directly in the conjugation of bile acids. Glycine and taurine are amino acids used to conjugate bile acids. Glucuronic acid and sulphate are used in the conjugation of other molecules, like bilirubin, drugs and hormones.
Question 164:
Answer: D. They are derived from cholesterol
Explanation:
A. is incorrect as bile acids are synthesised in the liver from cholesterol.
B. is incorrect as bile acids do not hydrolyse proteins; they emulsify fats.
C. is incorrect as bile acids are primarily reabsorbed in the terminal ileum, not the jejunum
E. is incorrect as bile acids do not neutralize gastric acid; bicarbonate from the pancreas performs that function.
Question 165:
Answer: B. Conversion of primary bile acids to secondary bile acids
Explanation: The conversion of primary bile acids to secondary bile acids is performed by intestinal bacteria, not cytochrome P450 enzymes. Cytochrome P450 enzymes hydroxylate cholesterol (e.g., CYP7A1), hydroxylate bile acids (e.g., CYP27A1), detoxify xenobiotics, and are involved in regulatory feedback mechanisms.
Question 166:
Answer: B. Conversion of cholesterol to 7-alpha-hydroxycholesterol
Explanation: The conversion of cholesterol to 7-alpha-hydroxycholesterol by CYP7A1 is the rate-limiting step in bile acid synthesis.
A. is incorrect as the conversion to pregnenolone is part of steroidogenesis, not bile acid synthesis.
C. is incorrect as conjugation with glycine or taurine occurs after primary bile acid formation
D. is incorrect as the conversion of 7-alpha-hydroxycholesterol to cholic acid is a subsequent step.
E. is incorrect as the reabsorption in the ileum is part of the enterohepatic circulation, not synthesis.

Question 167:
Answer: C. Phase III
Explanation: Phase III of the MMC is characterised by intense, rhythmic contractions that sweep through the stomach and small intestine and the key hormone responsible for this is motilin.
B. is incorrect as Phase II is a period with intermittent, irregular contractions that gradually increase in frequency and intensity.
D. is incorrect as Phase IV is a period of short transitional phase leading back to the period of quiescence.
E. is incorrect as Phase V is not even a phase of MMC cycle.


Question 168:
Answer: C. Interstitial cells of Cajal
Explanation: Interstitial cells of Cajal act as pacemakers in the gastrointestinal tract, generating slow waves of electrical activity that regulate smooth muscle contractions.
A. is incorrect as parietal cells are cells in the stomach lining that secrete hydrochloric acid and intrinsic factor.
B. is incorrect as chief cells are cells in the stomach lining that secrete pepsinogen, the precursor to the enzyme pepsin.
D. is incorrect as enteroendocrine cells are cells scattered throughout the gastrointestinal tract that secrete various hormones involved in digestion, they include G cells which secrete gastrin, D cells which secrete somatostatin and I cells which secrete CCK etc.
E. is incorrect as goblet cells are cells that secrete mucus to protect the mucous membranes of the gastrointestinal tract.

Question 169:
Answer: C. 5.5
Explanation: The critical pH in saliva below which enamel demineralisation occurs is 5.5. Above this pH, the saliva is supersaturated with calcium and phosphate, protecting teeth from demineralisation.
A. is incorrect pH 3.5 level is highly acidic and would lead to severe demineralisation, but it is not typically relevant to normal oral conditions.
B. is incorrect as pH 4.5 is still highly acidic and more relevant to erosive conditions, but not the critical threshold for enamel.
D. is incorrect as pH 6.5 is slightly acidic but above the threshold where enamel demineralisation begins.
E. is incorrect as pH 7.5 is a neutral to slightly basic pH which is generally protective against enamel demineralisation.
Question 170:
Answer: C. Muscarinic M3 receptor
Explanation: Acetylcholine stimulates gastric acid secretion primarily through the muscarinic M3 receptors on parietal cells.
A. is incorrect as nicotinic receptor are found in the neuromuscular junction and autonomic ganglia but are not directly involved in gastric acid secretion.
B. is incorrect as muscarinic M2 receptors are primarily found in cardiac tissue and involved in reducing heart rate, not stimulating acid secretion.
D. is incorrect as beta-adrenergic receptor are part of the sympathetic nervous system and are not involved in acid secretion.
E. is incorrect as alpha-adrenergic receptor are also part of the sympathetic nervous system and do not play a direct role in gastric acid secretion
Question 171:
Answer: B. Secretin
Explanation: Secretin stimulates ductal cells of the pancreas to release bicarbonate into the duodenum to neutralise stomach acid.
A. is incorrect as gastrin primarily stimulates gastric acid secretion and growth of the gastric mucosa.
C. is incorrect as cholecystokinin (CCK) stimulates gallbladder contraction and pancreatic enzyme secretion but not bicarbonate release.
D. is incorrect as histamine stimulates gastric acid secretion via H2 receptors but has no direct role in bicarbonate secretion.
E. is incorrect as motilin stimulates gastric and intestinal motility but does not influence bicarbonate secretion.
Question 172:
Answer: C. Muscularis externa
Explanation: The myenteric plexus, or Auerbach’s plexus, is located between the circular and longitudinal muscle layers of the muscularis externa and is responsible for controlling gut motility.
A. is incorrect as the mucosa is the innermost layer involved in secretion and absorption.
B. is incorrect as the submucosa contains blood vessels, lymphatics, and the submucosal (meissner’s) plexus but not the myenteric plexus.
D. is incorrect as the serosa is the outermost layer providing structural support and protection but does not contain the myenteric plexus.
E. is incorrect as the adventitia is a connective tissue layer found in retroperitoneal organs, not typically containing the myenteric plexus.

Question 173:
Answer: C. H+/K+ ATPase (Proton pump)
Explanation: The H+/K+ ATPase, also known as the proton pump, is responsible for the final step in gastric acid production, actively exchanging H+ ions into the gastric lumen in exchange for K+ ions.
A. is incorrect as carbonic anhydrase catalyses the formation of carbonic acid from CO2 and water but is not the final step in acid secretion.
B. is incorrect as HCO3-/Cl- exchanger is responsible for maintaining electroneutrality in the blood when Cl- moves into the parietal cells
D. is incorrect as pepsinogen is a precursor to pepsin, involved in protein digestion but not acid secretion.
E. is incorrect as gastric lipase is an enzyme involved in fat digestion, not in acid production
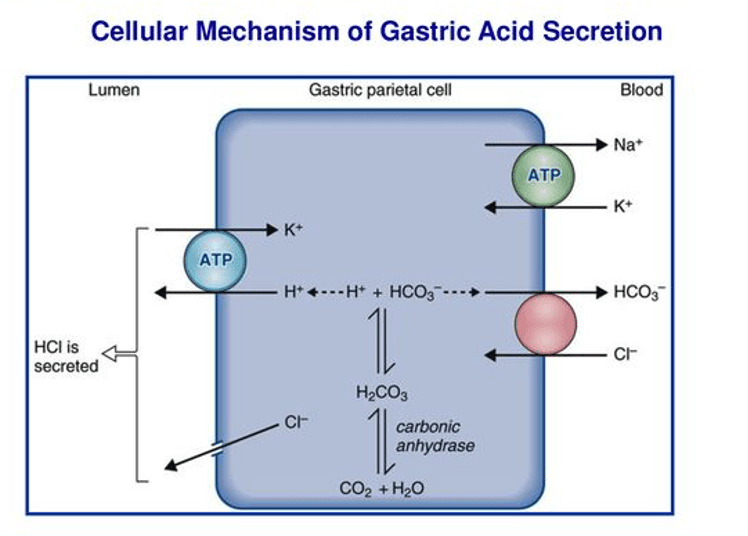
Question 174:
Answer: B. Proton pump inhibitors (PPIs)
Explanation: Proton pump inhibitors (PPIs) block the H+/K+ ATPase enzyme, reducing gastric acid production.
A. is incorrect as H2 receptor antagonists block histamine receptors on parietal cells but do not inhibit the proton pump directly.
C. is incorrect as antacids neutralise existing stomach acid but do not inhibit its production.
D. is incorrect as anticholinergics reduce gastric secretions through various mechanisms but not directly via the proton pump.
E. is incorrect as beta-blockers primarily affect the cardiovascular system and are not used for gastric acid reduction.
Question 175:
Answer: C. Mucosal damage due to bacterial toxins and inflammation
Explanation: Helicobacter pylori causes peptic ulcers primarily through mucosal damage due to bacterial toxins and the resulting inflammatory response. While H. pylori can also increase acid production, the primary mechanism of ulcer formation is mucosal damage.
Question 176:
Answer: B. H2 receptor
Explanation: Histamine stimulates gastric acid secretion through H2 receptors on parietal cells. H1 receptors are involved in allergic reactions, H3 receptors are primarily found in the central nervous system, H4 receptors are involved in immune responses and M3 receptor are muscarinic receptors involved in acetylcholine-mediated responses, not histamine.
Question 177:
Answer: D. PEPT1 (Peptide Transporter 1)
Explanation: PEPT1 is responsible for the active transport of dipeptides and tripeptides from the intestinal lumen into the enterocytes. It is essential for protein digestion and absorption. Other proteins listed are involved in iron metabolism or have different functions unrelated to peptide absorption.
A is incorrect as ferroportin is a protein that exports ferrous iron from enterocytes into the bloodstream but is not involved in peptide transport.
B is incorrect as ferroreductase is an enzyme responsible for reducing ferric iron (Fe³⁺) to ferrous iron (Fe²⁺) but does not handle peptides.
C is incorrect as DMT1 is a transporter that uptakes ferrous iron (Fe²⁺) and other divalent metals but does not transport peptides.
E is incorrect as hephaestin is a protein oxidises ferrous iron (Fe²⁺) to ferric iron (Fe³⁺) but does not facilitate peptide absorption.

Question 178:
Answer: B. Ferrous iron (Fe²⁺)
Explanation: Ferrous iron (Fe²⁺) is more readily absorbed than ferric iron (Fe³⁺). The reduction of ferric iron to ferrous iron is a crucial step for its efficient absorption. In circulation Iron is in the ferric (fe3+) and inside cells iron is in the ferrous (Fe2+) form.
A. is incorrect as ferric iron (Fe3+) is not readily absorbed in the intestine and needs to be reduced to ferrous iron (Fe²⁺) before absorption can occur.
C. is incorrect as ferric iron refers to Fe³⁺, and there is no form of ferric iron as Fe²⁺.
D. is incorrect as because ferrous iron is Fe²⁺, not Fe³⁺.
E. is incorrect as ferrous iron (Fe²⁺) is absorbed more efficiently than ferric iron (Fe³⁺), which requires reduction.
Question 179:
Answer: B. Ferroportin
Explanation: Ferroportin is essential for exporting iron from enterocytes into the bloodstream, playing a key role in systemic iron regulation.
A. is incorrect as PEPT1 is involved in the uptake of peptides, not iron export.
C. is incorrect DMT1 is involved in the uptake of ferrous iron (Fe²⁺) into enterocytes, not in exporting iron.
D. is incorrect DCTYB converts ferric (Fe3+) to ferrous (Fe2+) to facilitate its absorption into the enterocytes.
E. is incorrect as ferrireductase like DCTYB reduces ferric iron (Fe³⁺) to ferrous iron (Fe²⁺) but does not export iron.
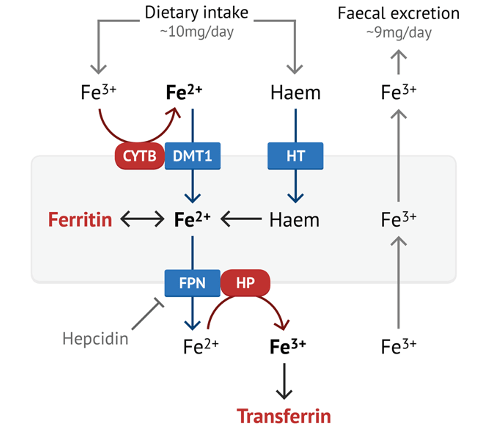
Question 180:
Answer: E. Hephaestin
Explanation: Hephaestin oxidises ferrous iron (Fe²⁺) to ferric iron (Fe³⁺) to facilitate its export from cells into the blood stream as iron needs to be in the ferric (Fe3+) form when not in cells.
A. is incorrect as PEPT1 is involved in tri and dipeptide transport but does not play a role in iron oxidation.
B. is incorrect as ferroportin exports iron out of enterocytes and into the bloodstream but does not oxidize it.
C. is incorrect as DMT1 is responsible for the uptake of ferrous iron and does not oxidise iron.
D. is incorrect as ferrireductase reduces ferric iron to ferrous iron, not the reverse.
Question 181:
Answer: D. Aquaporin 10
Explanation: Aquaporin 10 is present on the luminal side of intestinal epithelial cells and facilitates the absorption of water from the intestinal lumen.
C. is incorrect as aquaporin 3 is located on the basal side of intestinal epithelial cells, facilitating water movement from the cells to the bloodstream.
Question 182:
Answer: D. Filiform papillae
Explanation: Filiform papillae are primarily responsible for the mechanical manipulation of food due to their long, pointed projections and lack of taste buds.
A. is incorrect as fungiform papillae are involved in taste perception and are located on the tip and margins of the tongue.
B. is incorrect as foliate papillae are involved in taste perception and are located on the sides of the tongue.
C. is incorrect as circumvallate papillae are involved in taste perception and are located at the back of the tongue.
E. is incorrect as taste buds are sensory organs located on various papillae and are involved in taste perception rather than mechanical manipulation.
Question 183:
Answer: D. Kidney
Explanation: The kidneys are retroperitoneal organs, located behind the peritoneal cavity. Other organs listed are intraperitoneal or have varying peritoneal relations.
C. is incorrect as the small intestine is generally considered intraperitoneal, although parts of the duodenum are retroperitoneal. Use the mnemonic SAD PUCKER to remember all the retroperitoneal organs.
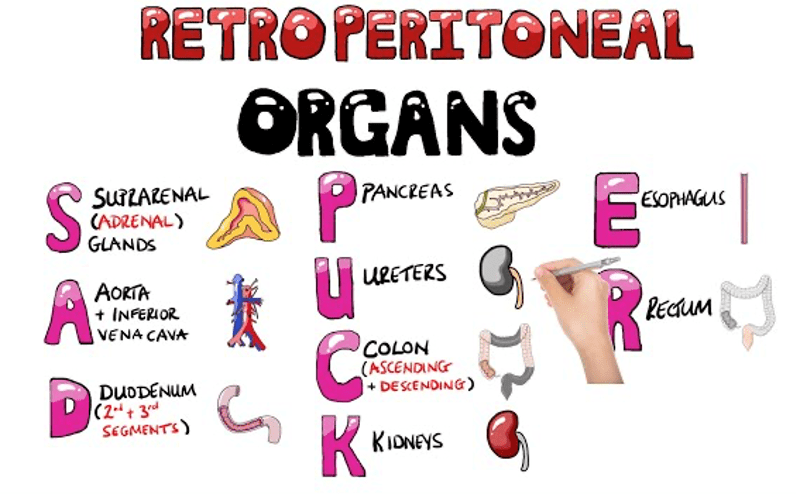
Question 184:
Answer: A. SPINK1 (Serine Peptidase Inhibitor, Kazal Type 1)
Explanation: SPINK1 is crucial in inhibiting the activation of pancreatic proteases and preventing premature digestion of pancreatic tissues. Its deficiency can lead to pancreatitis, and hypercalcemia can aggravate this condition by increasing enzyme activity as it causes Cathepsin B to fuse with zymogens activating them prematurely.
B. is incorrect as trypsinogen is the inactive precursor of trypsin and does not directly inhibit protease activity during hypercalcemia it is activated to trypsin prematurely which ends up digesting the pancreas in pancreatitis.
Question 185:
Answer: A. Butyrate and Propionate
Explanation: Butyrate and propionate are short-chain fatty acids made of 6 carbons or less and produced by the fermentation of dietary fibres in the colon. Butyrate is crucial for colonocyte energy and has anti-inflammatory properties, while propionate is involved in gluconeogenesis and cholesterol reduction.
B. is incorrect as they are ketone bodies produced during fat metabolism and are not primarily involved in fibre fermentation in the colon.
C. is incorrect as they are long-chain fatty acids derived from dietary fats, not short-chain fatty acids produced by fermentation.
D. is incorrect as they are essential fatty acids found in dietary fats, not short-chain fatty acids produced by fibre fermentation.
E. is incorrect as they are lipids involved in fat metabolism and not short-chain fatty acids from fibre fermentation.
Question 186:
Answer: a) Interstitial cells of Cajal
Explanation: These cells act as pacemakers for gastrointestinal motility, generating slow-wave potentials that initiate rhythmic contractions in the smooth muscle of the stomach and the rest of the GI tract.
b) is incorrect as enteric glial cells support neurons but do not act as pacemakers for muscle contraction.
c) is incorrect as enteroendocrine cells secrete hormones such as gastrin and secretin but do not directly initiate smooth muscle contractions.
d) is incorrect as chief cells secrete pepsinogen and do not influence smooth muscle contraction.
e) is incorrect as parietal cells secrete hydrochloric acid and intrinsic factor but do not initiate smooth muscle contraction.
Question 187:
Answer: a) Primary bile acids are synthesised from cholesterol in the liver, while secondary bile acids are formed by bacterial conversion in the intestines.
Explanation: Primary bile acids (e.g., cholic acid and chenodeoxycholic acid) are synthesised in the liver from cholesterol. Secondary bile acids (e.g., deoxycholic acid and lithocholic acid) are formed by bacterial action in the intestines.
b) is incorrect as primary bile acids are synthesised in the liver, not secondary bile acids.
c) is incorrect as primary bile acids are synthesised in the liver, but secondary bile acids are formed in the intestines.
d) is incorrect as bile acids are not formed in the stomach or pancreas; primary bile acids are synthesised in the liver.
e) is incorrect as both primary and secondary bile acids are excreted via the bile into the intestines, not the kidneys.
Question 188:
Answer: a) Gastric emptying
Explanation: The MMC plays a crucial role in clearing the stomach and small intestine of residual chyme between meals. Impaired MMC function can lead to delayed gastric emptying and constipation.
b) is incorrect as while MMC affects gut motility, nutrient absorption is primarily related to the absorptive capacity of the intestinal mucosa.
c) is incorrect as faecal incontinence is primarily related to anal sphincter function and not directly impacted by MMC function.
d) is incorrect as pancreatic enzyme secretion is regulated by hormones like secretin and CCK, not by MMC function.
e) is incorrect as hepatic bile production is regulated by liver function and hormonal signals but not by MMC function.
