
MSK Answers (Y2)
Question 1:
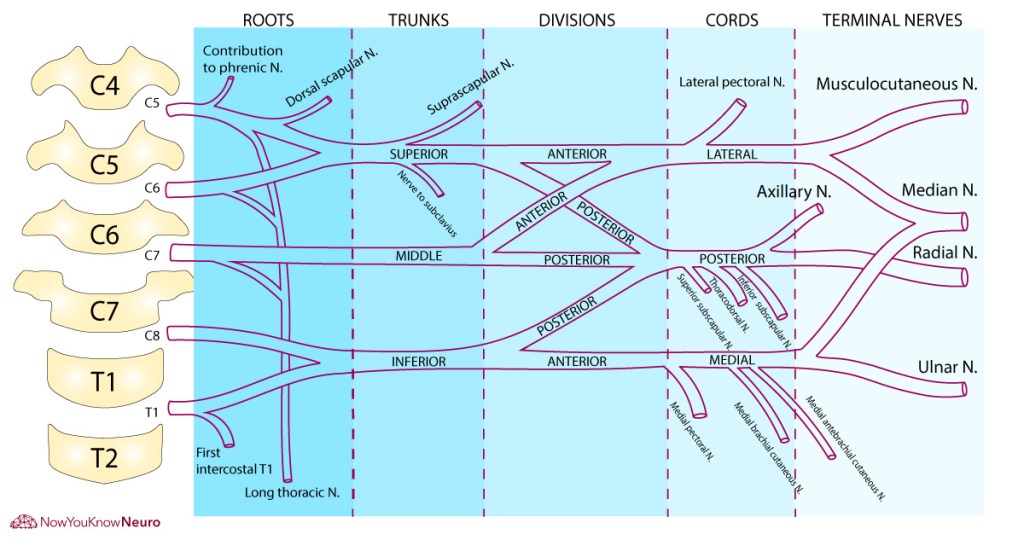
Answer: B) Axillary nerve
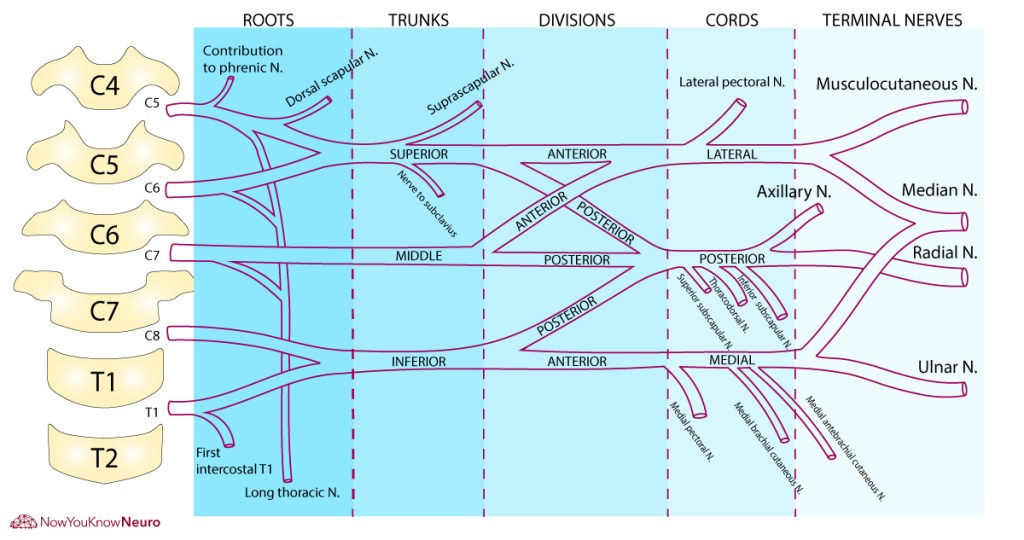
Explanation: The axillary nerve originates from the posterior cord of the brachial plexus (C5–C6) and passes through the quadrangular space. It innervates:
Deltoid which abducts the arm from 15° to 90°
Teres minor which laterally rotates the arm
Damage to the axillary nerve leads to a weakness in abduction beyond 15° (the initial 0–15° is done by supraspinatus), a flattened shoulder contour due to deltoid atrophy and a loss of sensation over the regimental badge area.
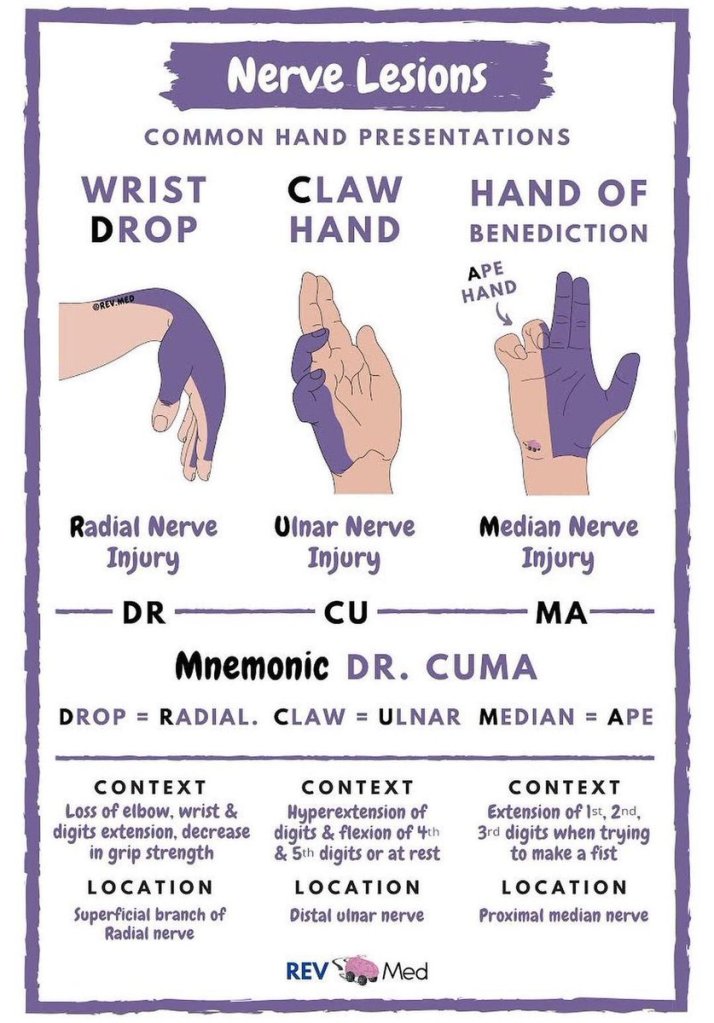
A) is incorrect because the radial nerve innervates the posterior arm/forearm (triceps, extensors) and damage here leads to wrist drop
C) is incorrect because the musculocutaneous nerve supplies the anterior arm (biceps, brachialis) and damage results in an inability to flex the elbow
D) is incorrect because the median nerve supplies the anterior forearm and thenar muscles, it has no role in the shoulder.
E) is incorrect because the long thoracic nerve innervates serratus anterior which protracts the scapula holding it flat against the thoracic wall, damage to this nerve cause a winged scapula.
Question 2:
Answer: A) Upper trunk
Explanation: The upper trunk (C5–C6) gives rise to nerves supplying the deltoid, supraspinatus, infraspinatus, and biceps. Erb’s palsy results from traction on the upper trunk, leading to the characteristic “waiter’s tip” position.
B) is incorrect because the lower trunk (C8–T1) causes Klumpke’s palsy, a claw hand.
C) is incorrect as the lateral cord gives rise to musculocutaneous and part of median nerve.
D) is incorrect as the posterior cord lesion would affect radial and axillary nerves.
E) is incorrect as the medial cord lesion mainly affects ulnar nerve distribution.
Question 3:
Answer: E) Wrist drop
Explanation: The posterior cord gives rise to the axillary and radial nerves. A lesion here affects wrist and finger extension, resulting in wrist drop, and may impair shoulder abduction.
A) is incorrect because winging of the scapula is due to the long thoracic nerve lesion.
B) is incorrect as claw hand results from the ulnar nerve damage.
C) is incorrect because thumb opposition is due to the median nerve and thenar muscles.
D) is incorrect since elbow flexion is controlled by the musculocutaneous nerve.
Question 4:
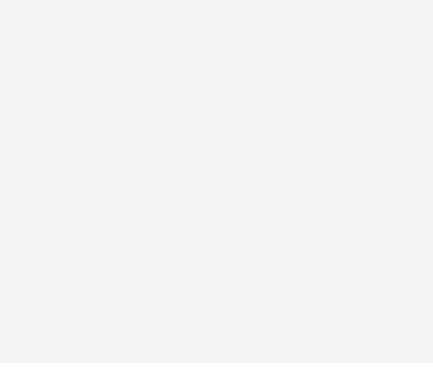
Answer: C) Median nerve
Explanation: The median nerve runs anterior to the elbow joint through the cubital fossa, making it vulnerable in supracondylar humerus fractures. This may lead to loss of forearm flexors and thenar muscle function as well as hand of benediction when trying to make a fist
A) is incorrect because the ulnar nerve runs behind the medial epicondyle.
B) is incorrect because the radial nerve runs posteriorly in the radial groove.
D) is incorrect since the musculocutaneous nerve lies in the arm, not at the elbow.
E) is incorrect because the axillary nerve is at the surgical neck, not the distal humerus.
Question 5:
Answer: C) Suprascapular nerve
Explanation: The suprascapular nerve (C5–C6) innervates supraspinatus which initiates abduction (0–15°) and infraspinatus which is involved in the lateral rotation of the arm. Lesions to this nerve leads to impaired initiation of abduction and reduced external rotation.
A) is incorrect because axillary nerve abducts from 15–90° via innervating the deltoid.
B) is incorrect as the long thoracic nerve controls scapular protraction through its innervation of serratus anterior.
C) is incorrect as the thoracodorsal nerve innervates latissimus dorsi, which is responsible for adduction and extension.
E) is incorrect since the radial nerve does not innervate shoulder muscles.
Question 6:
Answer: D) Brachioradialis – Radial nerve
Explanation: The brachioradialis, although is a flexor of the forearm, is innervated by the radial nerve.
A) is incorrect because pronator teres is innervated by the median nerve, not radial.
B) is incorrect as flexor carpi ulnaris is innervated by the ulnar nerve, not median.
C) is incorrect as infraspinatus is supplied by the suprascapular nerve, not axillary.
E) is incorrect because subscapularis is innervated by the upper and lower subscapular nerves, not suprascapular.
Question 7:
Answer: C) Midshaft
Explanation: The radial nerve runs along the radial (spiral) groove of the humerus. A midshaft humeral fracture puts this nerve at risk, leading to wrist drop due to loss of wrist/finger extensors, and loss of sensation over the posterior forearm and dorsum of the hand.
A) is incorrect as a surgical neck fracture affects the axillary nerve, impairing shoulder abduction.
B) is incorrect because medial epicondyle fractures damage the ulnar nerve, causing claw hand.
D) is incorrect because the lateral epicondyle is the origin of wrist extensors but not where radial nerve injury occurs.
E) is incorrect because supracondylar fractures affect the median nerve, not radial.

Question 8:
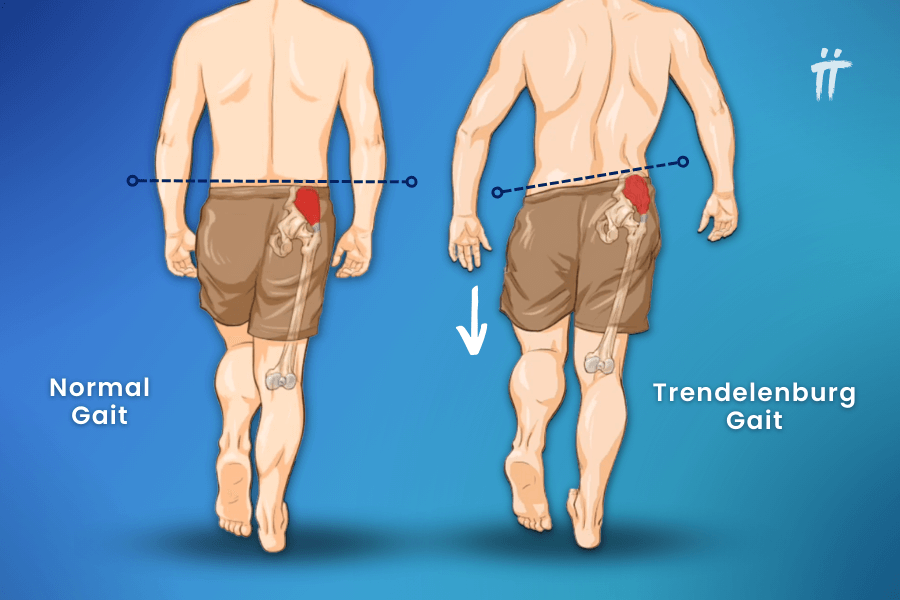
Answer: D) Superior gluteal
Explanation: The superior gluteal nerve (L4–S1) innervates gluteus medius, gluteus minimus, and tensor fasciae latae, which abduct and stabilize the pelvis during gait. Injury causes Trendelenburg sign – pelvic drop on the contralateral swing side.
A) is incorrect because the inferior gluteal nerve innervates gluteus maximus, affects hip extension, not abduction.
B) is incorrect because the obturator nerve innervates the medial thigh causing adduction.
C) is incorrect because the sciatic nerve innervates the posterior thigh and leg, not abductors, causing extension.
E) is incorrect as the femoral innervates the anterior thigh resulting in hip flexion and knee extension.
Question 9:
Answer: D) Claw toe
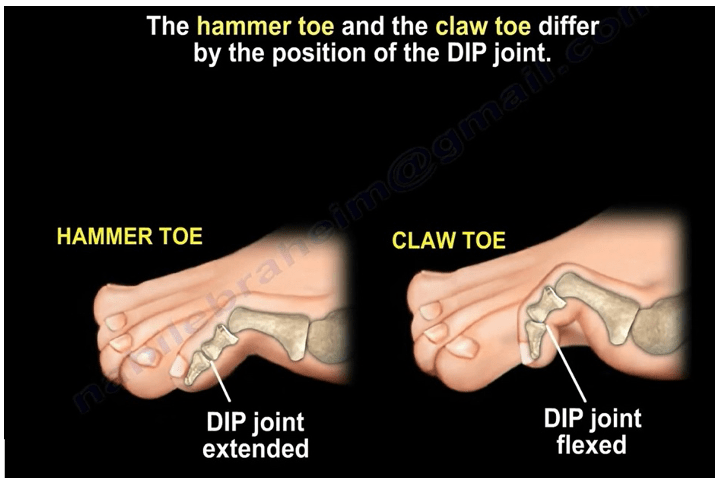
Explanation: Claw toe is a classic deformity associated with neuromuscular disease (e.g., diabetes, Charcot-Marie-Tooth, spinal cord injury) and results from an imbalance between the long toe flexors/extensors and intrinsic foot muscles. The MTP joint becomes hyperextended due to an overpull of extensor digitorum longus. The PIP and DIP joints are flexed due to unopposed flexor digitorum longus and brevis. This often affects lateral toes and may cause corns or pressure ulcers due to shoe rubbing.
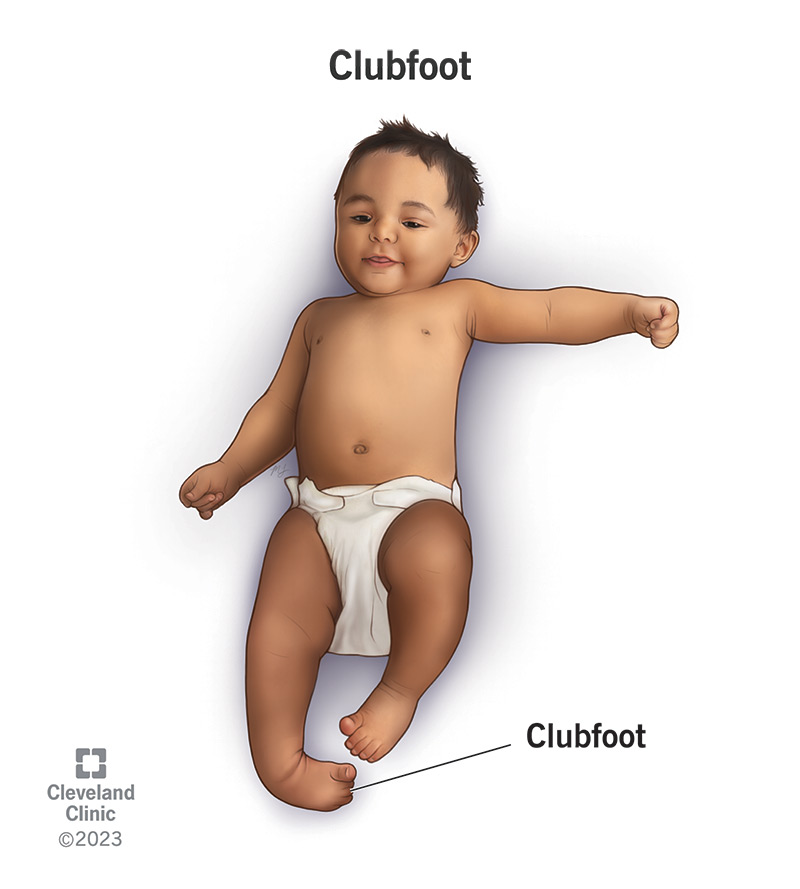
A) is incorrect because hammer toe has flexion at the PIP joint only, with a neutral or extended MTP, often affecting a single toe.
B) is incorrect as club foot is congenital causing inversion, plantarflexion, and forefoot adduction.
C) is incorrect as hallux valgus is a lateral deviation of the big toe with medial deviation of the first metatarsal resulting in a bunion formation.
E) is incorrect as the Trendelenburg gait is a hip abductor dysfunction due to superior gluteal nerve lesion.

Question 10:
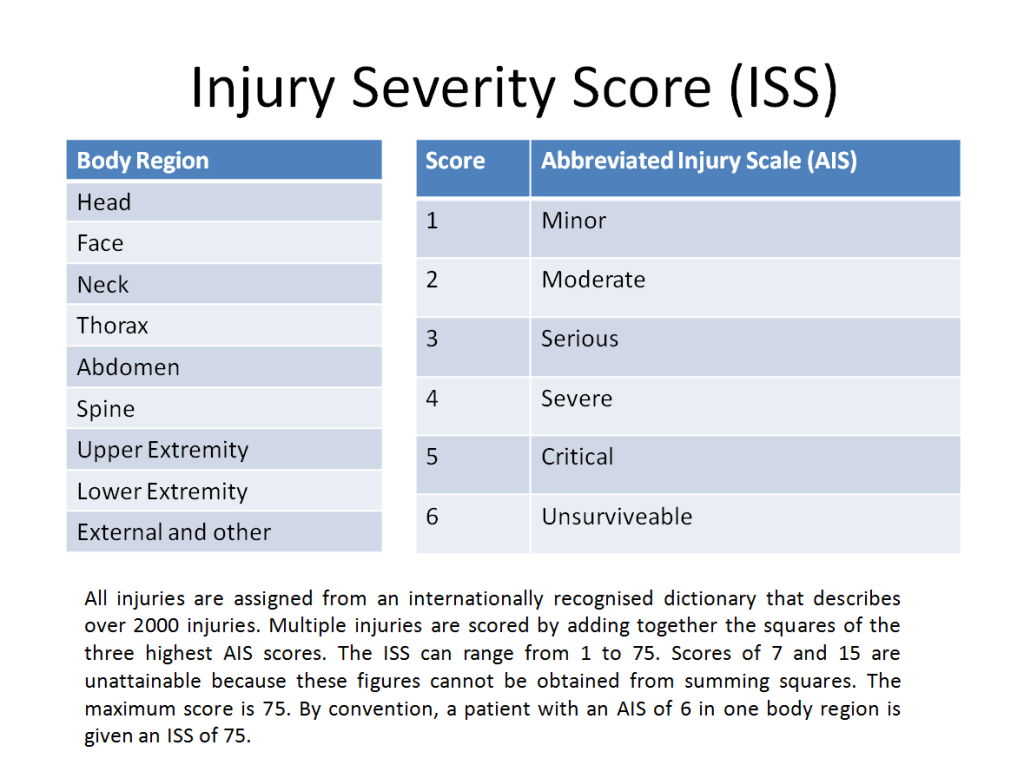
Answer: C) ISS ≥12–15 usually defines major trauma
Explanation: The Injury Severity Score sums the squares of the highest AIS scores in the 3 most severely injured body regions. Each AIS score ranges from 1 (minor) to 6 (unsurvivable). A single AIS of 6 results in an ISS of 75.
A) is incorrect as an AIS of 6 results in automatic 75.
B) Incorrect as the ISS uses the 3 highest, not lowest scores.
D) is incorrect as the ISS range is 0–75, not 50.
E) is incorrect because the ISS is based on injuries, not vital signs.
Question 11:
Answer: A) 2 hours post-injury with active bleeding
Explanation: Tranexamic is an inhibitor of plasminogen with antifibrinolytic action stabilising clots. It is indicated in the treatment of excessive blood loss from major trauma, menorrhagia, postpartum bleeding and epistaxis. TXA reduces mortality if given within 3 hours of trauma.
B and C) are incorrect as this is outside window and not indicated
D) is incorrect because there is no sign of bleeding
E) is incorrect because TXA is used differently in elective surgery
Question 12:
Answer: B) Plantar fasciitis
Explanation: Plantar fasciitis is common degenerative condition of the plantar fascia that is caused by mechanical overuse, usually related to prolonged standing, elevated BMI, and repetitive activities such as running. It typically presents with foot/heel pain that is worse in the morning, improves throughout the day, and worsens again in the evening.
A) is incorrect because achilles tendinopathy manifests with pain and tenderness 2–6 cm above the insertion of the Achilles tendon.
C) is incorrect because tarsal tunnel involves the posterior tibial nerve becoming compressed within the tarsal tunnel. Manifestations include neuropathic pain, paraesthesia, and numbness in the posteromedial ankle, heel, and toes.
D) is incorrect because a fracture would need trauma and would result in swelling.
E) is incorrect because PTT causes medial foot arch pain.
Question 13:
Answer: C) Tennis elbow
Explanation: Tennis elbow aka lateral epicondylitis is an overuse injury typically caused by activities that involve repetitive wrist extension and/or repetitive forearm supination-pronation with the elbow in near complete extension (e.g., racket sports). It results in microtears at the lateral epicondyle.
A) is incorrect because golfer’s elbow affects the medial epicondyle
B) is incorrect because olecranon bursitis is inflammation of the olecranon bursa that is caused by acute trauma to the elbow joint, chronic irritation (e.g., leaning on the elbows for a prolonged period, repetitive elbow flexion-extension, gout crystals), systemic inflammatory process (e.g., rheumatoid arthritis), or abrasions to the skin overlying the olecranon bursa. Patients typically present with a swelling on the posterior surface of the elbow. If infected, the skin over the swollen bursa may become warm and tender.
D) is incorrect because radial tunnel syndrome involves radial nerve compression but more distally and not tender at the epicondyle
E) is incorrect because cubital tunnel syndrome is a condition characterised by compression of the ulnar nerve at the medial epicondyle of the humerus. It can be caused by leaning on the elbow, prolonged elbow flexion, trauma, and repetitive use of the forearm flexors (e.g., baseball players, bodybuilders, wrestlers). Symptoms include numbness/paraesthesia along the ring and little fingers that can be reproduced by tapping on the medial epicondyle (Tinel test) and elbow pain that radiates to the forearm.
Question 14:
Answer: E) Positive PR3-ANCA with nasal crusting
Explanation: GPA is an immune-mediated necrotizing vasculitis that most commonly affects small vessels in the upper and lower respiratory tract, eyes, and kidneys. It classically manifests with ENT involvement saddle-nose deformity, haematuria, and PR3-ANCA positivity.
A) is incorrect as this suggests EGPA (eosinophilic GPA) also known as Churg Strauss syndrome, not GPA.
B) is incorrect as this is a presentation of Behçet’s disease.
C) is incorrect because although it could be seen in lupus nephritis or ANCA vasculitis or glomerulonephritis, but it lacks specificity.
D) is incorrect as this suggests IgA vasculitis aka Henoch-Schonlein Purpura (HSP).

Question 15:
Answer: D) IgA vasculitis – Immune complex-mediated
Explanation: IgA vasculitis (HSP) involves IgA immune complex deposition in small vessels leading to purpura, arthralgia, abdominal pain, and nephritis.
A) is incorrect because EGPA is ANCA-mediated, not T-cell granulomas.
B) is incorrect because GCA is T-cell-mediated, not immune complexes.
C) is incorrect because GPA is ANCA-associated, not immune complex-driven.
E) is incorrect because MPA is also ANCA-associated, not T-cell-mediated.
Question 16:
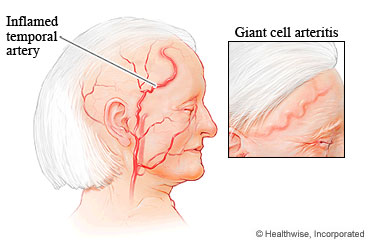
Answer: B) Initiate high-dose oral prednisolone immediately
Explanation: This is a presentation describing Giant Cell Arteritis (GCA) which is a medical emergency due to risk of permanent vision loss. Start high-dose steroids (e.g., prednisolone 40–60 mg daily) immediately — before biopsy.
A) is incorrect as although a biopsy should be done, it should not be performed before treatment, as delay risks blindness.
C) is incorrect as although aspirin may help reduce ischaemic complications, it is not sufficient alone.
D) is incorrect because outpatient referral would delay treatment and GCA is urgent.
E) is incorrect because MRI is not first-line in suspected GCA.
Question 17:
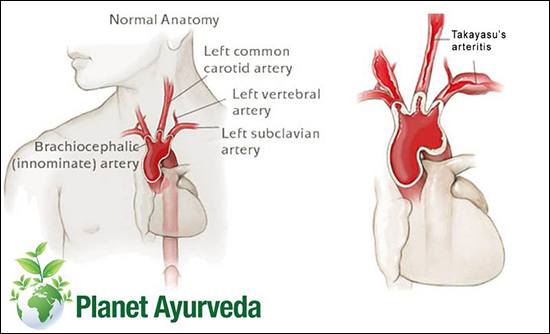
Answer: A) Most often affects the aortic arch and its branches
Explanation: Takayasu arteritis is a large vessel vasculitis that mainly involves the aorta and its major branches. It predominantly affects women < 50 years of age and manifests with fever, malaise, and weight loss. The typical clinical features include absent or decreased peripheral pulses, bruits, and limb claudication.
B) is incorrect as IgA deposition is present in IgA vasculitis.
C) is incorrect because it is not ANCA-associated.
D) is incorrect as it affects younger females, not older males.
E) is incorrect because purpura and arthritis are seen in IgA vasculitis.
Question 18:
Answer: C) Ankylosing spondylitis
Explanation: Ankylosing spondylitis is a chronic inflammatory disease of the axial skeleton that leads to partial or complete vertebral fusion (bamboo spine) and spine rigidity. It mainly affects male individuals and > 90% of patients are positive for HLA-B27. Clinical features include pain, uveitis and stiffness in the neck and lower back that improves with exercise.
A) is incorrect as cause equina would present with urinary retention and saddle anaesthesia.
B) is incorrect because mechanical pain doesn’t improve with exercise.
D) is incorrect because a spinal tumour would involve constant and progressive pain.
E) is incorrect because OA usually occurs in older adults and is not inflammatory.
Question 19:
Answer: B) Duchenne muscular dystrophy
Explanations: This is an X-linked recessive genetic disease in which mutations in the dystrophin gene resulting in a defective protein product. It causes subsequent degeneration of muscle fibres, causing proximal muscle weakness along with cardiomyopathy and bone fragility. Signs include proximal muscle weakness (especially in pelvic girdle), Gower’s sign (using hands to “climb up” from floor), pseudohypertrophy of calf muscles (due to fibrofatty infiltration) and a raised creatine kinase (CK).
A) is incorrect because Becker muscular dystrophy although is due to a dystrophin mutation, it results in partially functional dystrophin, with later onset (teens) and milder progression than DMD.
C) is incorrect because although Spinal muscular atrophy (SMA) causes proximal muscle weakness. Fasciculations and hypotonia in infancy are more typical and it does not cause calf hypertrophy or Gower’s sign.
D) is incorrect because Charcot-Marie-Tooth disease is a peripheral neuropathy that presents with distal muscle weakness, foot drop, and pes cavus. Calf hypertrophy is present but is true hypertrophy from overuse, not pseudohypertrophy.
E) is incorrect because Cerebral palsy is a non-progressive disorder of movement and posture caused by brain injury. This boy has progressive symptoms, making CP unlikely.

Question 20:
Answer: C) Optic neuritis
Explanation: Optic neuritis is an inflammatory demyelination of the optic nerve. The most common identifiable cause is multiple sclerosis. It involves demyelination of the optic nerve, leading to unilateral eye pain (worse on movement), visual loss, decreased colour vision (especially red desaturation) and relative afferent pupillary defect (RAPD).
A) is incorrect as central retinal artery occlusion causes painless, sudden vision loss with a pale retina and cherry-red spot.
B) is incorrect as temporal arteritis typically affects patients over 50 and presents with headache, jaw claudication, and visual loss.
D) is incorrect because retinal detachment causes flashes, floaters, and a curtain-like vision loss, not RAPD.
E) is incorrect because diabetic retinopathy is bilateral and chronic, not associated with acute pain or RAPD.
Question 21:
Answer: D) Myotonic dystrophy
Explanation: Myotonic dystrophy is an autosomal dominant myopathy characterized by myotonia (slow relaxation of muscles after cessation of contraction) and slowly progressive weakness of muscles in the face and/or limbs. It can also cause frontal balding, cataracts, and cardiac conduction defects
A) is incorrect because it causes fatigable weakness but no myotonia.
B) is incorrect because is MS is a CNS demyelinating disease, not muscular.
C) is incorrect because Becker causes proximal muscle weakness without myotonia.
E) is incorrect because GBS causes ascending paralysis with absent reflexes.

Question 22:
Answer: B) Prosthetic joint infection
Explanation: Prosthetic joint infection (PJI) should be considered in any patient with a prosthetic joint who presents with acute joint inflammation and signs of infection. A WBC count >3,000 in a prosthetic joint aspirate is suggestive of infection therefor, a WBC >50,000 is very strongly supportive, especially in the presence of a turbid aspirate.
A) is incorrect because gout presents with monosodium urate crystals; WBC can be elevated but not usually >50,000 in prosthetic joints.
C) is incorrect as pseudogout (calcium pyrophosphate crystals) also can mimic infection but is not associated with high WBC count in prosthetic joints.
D) is incorrect because RA causes chronic inflammation and is typically symmetrical, with lower WBC counts and no purulence.
E) is incorrect because OA is non-inflammatory, with WBC <1,500/µL.
Question 23:
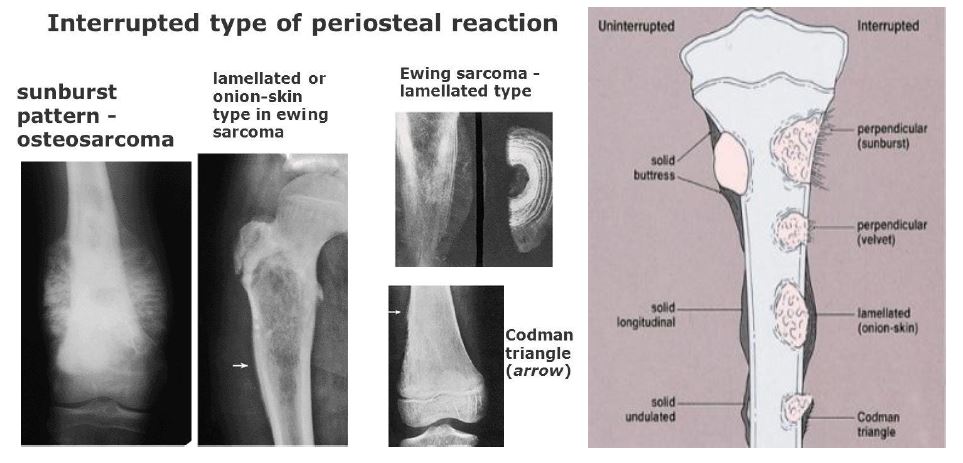
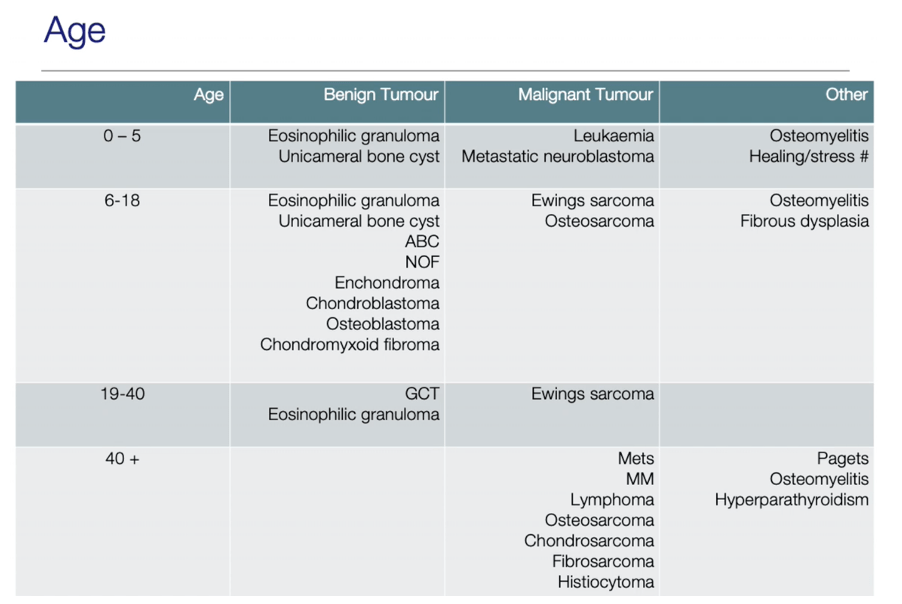
Answer: A) Ewing’s sarcoma
Explanation: Ewing’s sarcoma is a malignant small round blue cell tumour, primarily affecting children and adolescents. It often affects the diaphysis of long bones and presents with an onion-skin periosteal reaction due to layered new bone formation.
B) is incorrect because osteosarcoma typically occurs in metaphysis with sunburst or Codman triangle periosteal reaction.
C) is incorrect because a giant cell tumour typically arises after epiphyseal closure (older teens to adults), affects the epiphysis/metaphysis.
D) is incorrect because fibrous dysplasia usually has a “ground glass” appearance on imaging and is more benign.
E) is incorrect because osteomyelitis although can mimic Ewing’s, it lacks the classic onion-skin appearance.
Question 24:
Answer: E) CRP >50
Explanation: Kocher’s criteria for septic arthritis include:
- Non–weight bearing
- Fever >38.5°C
- ESR >40 mm/hr
- WBC >12,000/μL
However, CRP is useful but not part of the original Kocher’s criteria.
Question 25:
Answer: C) Gout
Explanation: Gout is an inflammatory arthropathy characterised by painful and swollen joints caused by precipitation of uric acid crystals. This is classic presentation is of acute gout, involving the 1st MTP joint (podagra), with negatively birefringent needle-shaped urate crystals. CKD and alcohol increase the risk of gout due to impaired uric acid excretion.
A) is incorrect as although septic arthritis may mimic this, the crystal identification and absence of systemic infection point away.
B) is incorrect because RA is chronic, symmetrical, and not typically monoarticular.
D) is incorrect because pseudogout crystals are positively birefringent and rhomboid shaped.
E) is incorrect because OA presents with chronic, mechanical joint pain, not acute inflammatory flares.
Question 26:
Answer: B) Systemic lupus erythematosus (SLE)
Explanation: SLE is a multisystem autoimmune disease that particularly affects women of childbearing age and leads to chronic inflammatory reactions in a variety of organs, including the skin, kidney, and joints. Typical findings include fever and fatigue, a malar rash (facial “butterfly rash”), myalgia, and arthritis. The “classic triad”: malar rash, photosensitivity, arthralgia/arthritis.
A) is incorrect because RA typically causes symmetric small joint polyarthritis, not rash.
C) is incorrect because dermatomyositis has heliotrope rash, not malar.
D) is incorrect because scleroderma features skin thickening and Raynaud’s.
E) is incorrect because Sjogren’s causes dry eyes and mouth (sicca syndrome).
Question 27:
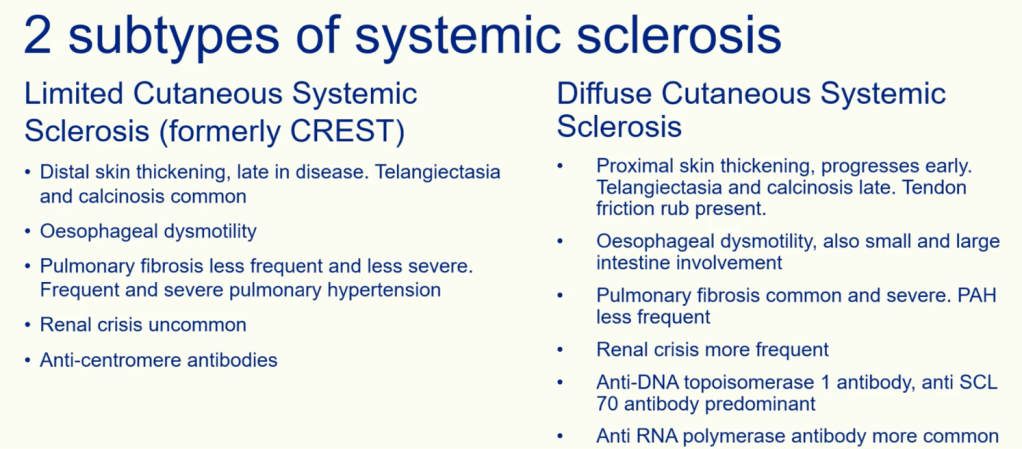
Answer: D) Anti-Scl-70 (anti-topoisomerase I)
Explanation: Anti-Scl-70 is associated with diffuse systemic sclerosis, involving internal organ fibrosis (GI, lungs, kidneys).
A) is incorrect as Anti-centromere is found in limited cutaneous/systemic sclerosis (CREST) not diffuse.
B) is incorrect as this is associated with SLE.
C) is incorrect as this is associated with mixed connective tissue disease.
E) is incorrect as this is seen in RA.
Question 28:
Answer: A) Anti-Ro (SSA)
Explanation: Anti-Ro is found in Sjogren’s syndrome and associated with dry eyes and mouth (sicca symptoms) and congenital heart block in neonatal lupus.
B) is incorrect because anti-centromere is linked to limited systemic sclerosis.
C) is incorrect because anti-scl-70 is linked to diffuse systemic sclerosis/
D) is incorrect because anti-dsDNA is linked to SLE
E) is incorrect because anti-jo-1 is linked to dermatomyositis and polymyositis.
Question 29:
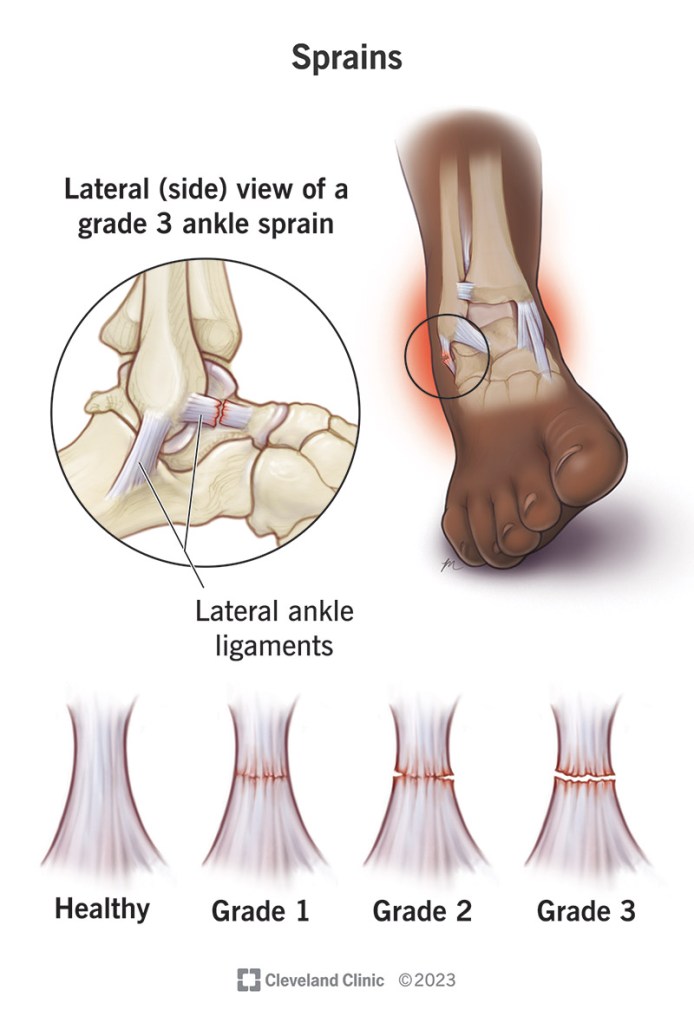
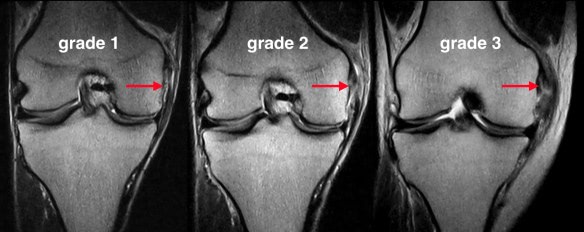
Answer: C) Grade 2
Explanation: Grade 2 sprain is a partial tear. On MRI a high signal with partial ligament disruption is seen
A) is incorrect as this is not a valid grade.
B) is incorrect because grade 1 is mild stretch with intact fibres.
D) is incorrect because grade 3 is a complete rupture with no continuity.
E) is incorrect because grade 4 is not part of standard classification.
Question 30:
Answer: E) Notochord
Explanation: The notochord is a dorsal midline structure derived from mesoderm that arises during the 3rd week of gestation (trilaminar disc). It secretes sonic hedgehog (SHH), a signalling protein that activates cellular differentiation and neurulation. It forms the nucleus pulposus of intervertebral discs.
A) is incorrect as neural crest cells give rise to the PNS and enterochromaffin cells of the adrenal medulla.
B) is incorrect because somites give rise to the annulus fibrosis of the vertebral disc.
C) is incorrect because the mesonephros is the embryological kidney.
D) is incorrect because the neural tube becomes the CNS.
Question 31:
Answer: C) Type III
Explanation: During inflammation and early proliferation, Type III collagen is laid down, later replaced by Type I in remodelling.
A) is incorrect because type I replaces Type III later becoming either bone, ligament or tendon.
B) is incorrect as type II is cartilage collagen.
D) is incorrect because type IV collagen is seen in basement membranes.
E) is incorrect because this is a minor collagen in interstitial matrices.
Question 32:
Answer: B) FGFR3
Explanation: Achondroplasia is a common cause of short stature caused by mutation of the fibroblast growth factor receptor 3 (FGFR3) gene which encodes for the FGFR3 receptor responsible for normal chondrocyte function and cartilage growth. Mutations in the gene that encodes this receptor cause growth abnormalities of connective tissue. It gives rise to the trident hand which is a deformity of the hand that is typically associated with achondroplasia and characterized by short stubby fingers of equal size and an increased separation between the middle finger and ring finger.
A) is incorrect as COL2A1 is seen in spondyloepiphyseal dysplasia and EDS, affecting type II collagen.
C) is incorrect as EXT1 is associated with hereditary multiple exostoses, causing cartilage-capped bone tumours.
D) is incorrect because PHEX is mutated in X-linked hypophosphataemic rickets, leading to phosphate wasting.
E) is incorrect because SLC26A2 is involved in diastrophic dysplasia, a rare skeletal dysplasia causing short-limbed dwarfism and joint deformities.
Question 33:
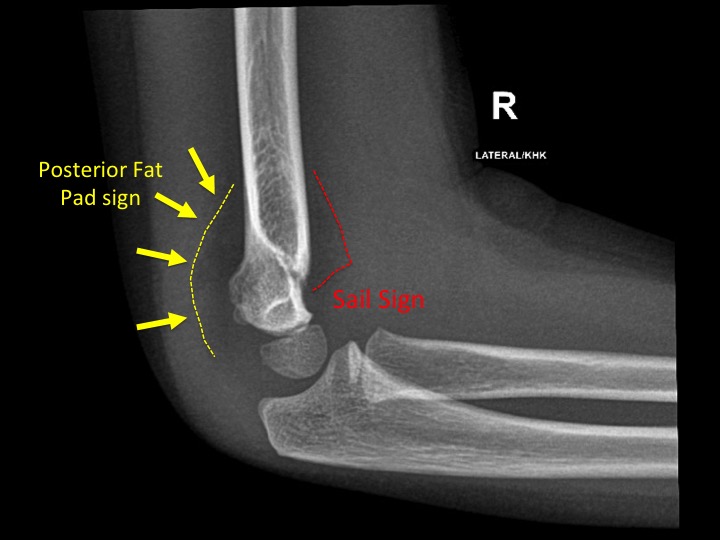
Answer: B) Joint effusion — radial head fracture
Explanation: The “sail sign” (anterior fat pad elevation) and posterior fat pad visibility on an elbow X-ray suggest intra-articular effusion, often due to an occult radial head fracture in adults (or supracondylar fracture in children).
A) is incorrect as a visible posterior fat pad is never normal, it indicates effusion.
C) is incorrect because olecranon dislocations are uncommon and usually show obvious bone displacement.
D) is incorrect because tendon rupture doesn’t typically cause joint effusion with fat pad signs.
E) is incorrect because radial head dislocation is more often seen in children (nursemaid’s elbow) and would be visible as joint malalignment.
Question 34:
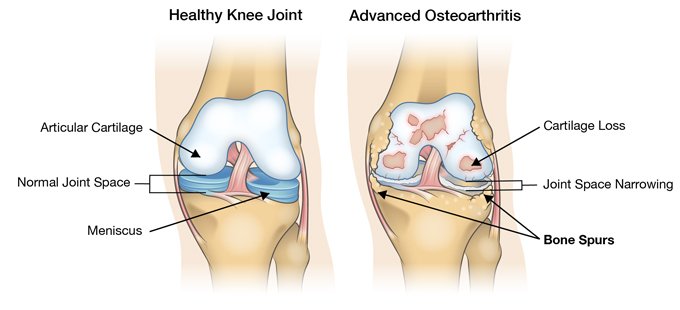
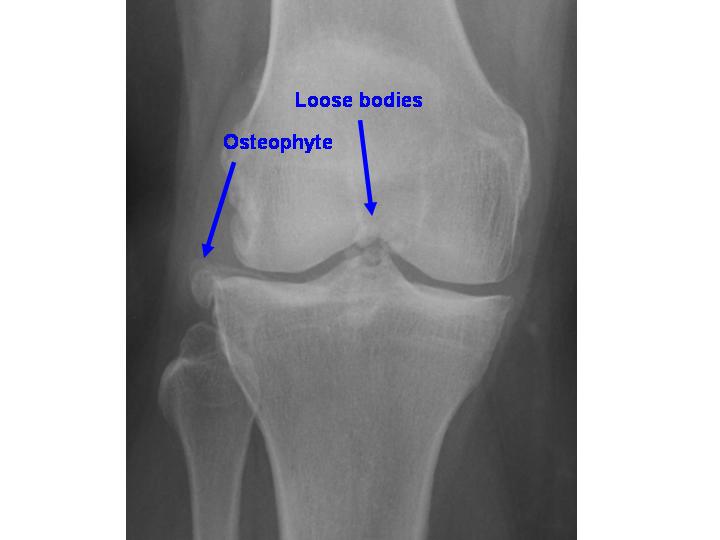
Answer: C) Osteophyte formation
Explanation: These are bony outgrowths that can occur in inflamed or degenerating joints (e.g., from osteoarthritis, joint ligament injury, ankylosing spondylitis). They can be asymptomatic or cause pain, joint deformity, tendinitis, restriction of joint movement, or compression of adjacent nerves. Visible on imaging as bony projections or spurs along the joint line.
A) is incorrect because periarticular osteopenia is typical of RA, not OA.
B) is incorrect because OA causes joint space narrowing, not widening.
D) is incorrect because erosions are characteristic of inflammatory arthritis (e.g., RA).
E) is incorrect because subchondral cysts may be present, but not in isolation, they accompany osteophytes and sclerosis and can also be present in RO.
Question 35:
Answer: D) Anti-CCP
Explanation: Anti-cyclic citrullinated peptide (anti-CCP) antibodies are highly specific for RA and often appear before clinical symptoms, especially in patients who are negative for rheumatoid factor.
A) is incorrect as ANA is non-specific and common in many autoimmune diseases.
B) is incorrect as Anti-dsDNA is specific for SLE.
C) is incorrect as RF is sensitive but not specific (seen in infections, other autoimmune conditions).
E) is incorrect because Anti-Ro is associated with Sjögren’s and neonatal lupus.
Question 36:
Answer: B) Marginal erosions
Explanation: Marginal (bare area) erosions are a hallmark of RA, caused by pannus eroding cartilage and bone. Joint space narrowing and periarticular osteopenia may also be seen.
A) is incorrect because subchondral sclerosis is typical in OA.
C) is incorrect because osteophytes are seen in OA.
D) is incorrect because joint space narrowing, not widening, occurs in RA.
E) is incorrect because bamboo spine is present in ankylosing spondylitis.
.
Question 37:
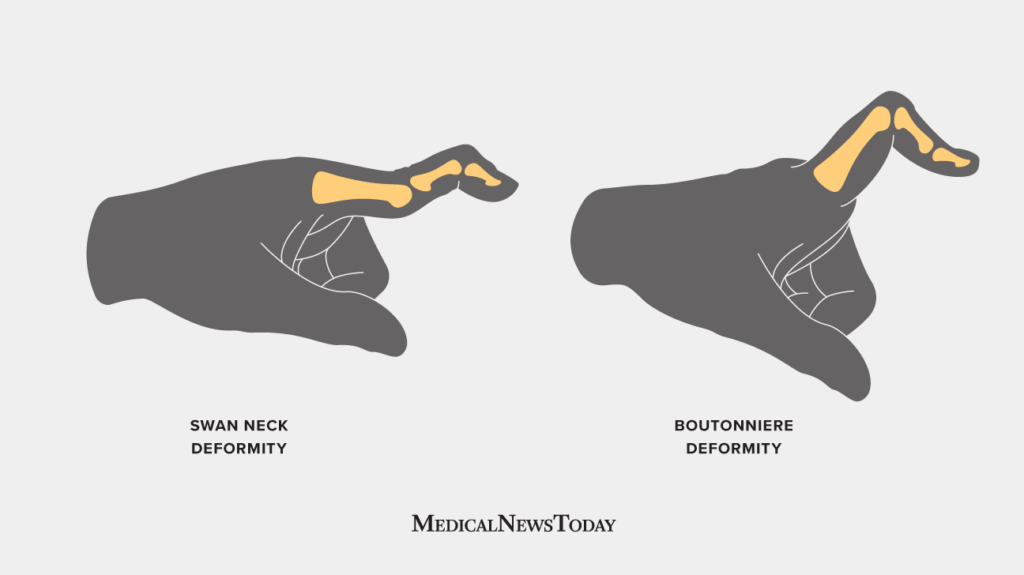
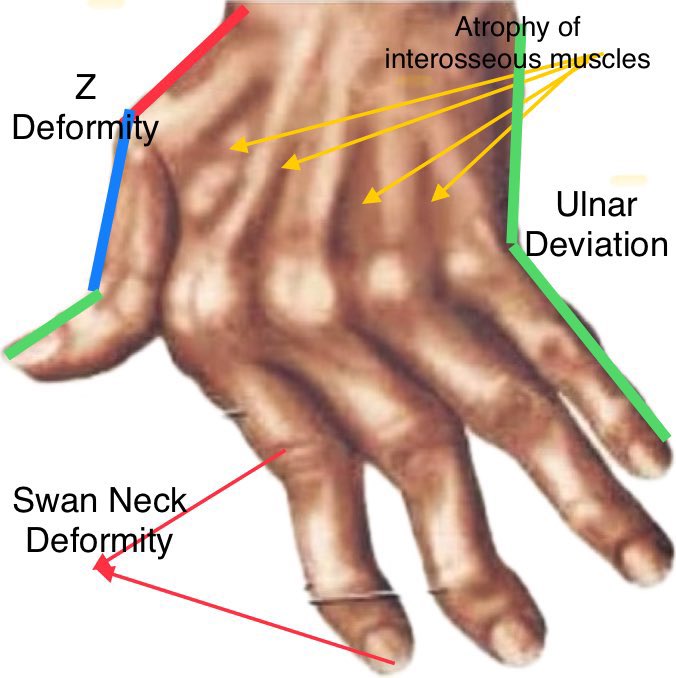
Answer: A) Boutonnière
Explanation: Boutonnière deformity results from rupture of the central slip of the extensor tendon causing PIP flexion and DIP hyperextension.
B) is incorrect as swan neck causes PIP hyperextension and DIP flexion.
C) is incorrect because Z-deformity is a thumb deformity in RA causing hyperextension of IP and MCP flexion.
D) is incorrect as claw hand is seen in ulnar nerve palsy causing MCP hyperextension and IP flexion.
E) is incorrect because ulnar drift is a RA deformity with MCP deviation toward the ulna.
Question 38:
Answer: B) Enteropathic arthritis
Explanation: A seronegative spondyloarthropathy that mimics Ankylosing spondylitis and develops in association with inflammatory bowel disease. Typically affects joints of the lower extremities but can involve the spine.
A) is incorrect because psoriatic arthritis involves skin and nail changes, not IBD.
C) is incorrect because reactive arthritis follows GI/GU infections, not IBD.
D) is incorrect because OA is not inflammatory and uncommon in young adults.
E) is incorrect because RA usually affects small joints symmetrically, not axial spine.
Question 39:
Answer: C) Apert syndrome
Explanation: This is an autosomal dominant condition caused by mutations in the FGFR2 gene on chromosome 10. It is a type of craniosynostosis syndrome involving craniosynostosis (premature skull suture fusion) and syndactyly (often complex, fused digits).
A) is incorrect because Holt-Oram causes upper limb abnormalities and cardiac defects (especially ASDs), not craniosynostosis.
B) is incorrect as VACTERL causes Vertebral, Anal, Cardiac, TE fistula, Renal, Limb deformities not specifically syndactyly or cranial issues.
D) is incorrect because DiGeorge involves 22q11 deletion and results in cardiac anomalies, thymic/aplasia, hypocalcaemia.
E) is incorrect because Ellis-van Creveld causes short stature, polydactyly, dental anomalies, not syndactyly or craniosynostosis.
Question 40:
Answer: C) Arises directly from the C5–C7 nerve roots
Explanation:
The long thoracic nerve, which innervates the serratus anterior, arises directly from the C5–C7 roots of the brachial plexus and runs superficially along the lateral thoracic wall. Injury to this nerve, often from trauma or surgery (e.g., axillary procedures), leads to medial scapular winging and impaired scapular protraction. Importantly, because the nerve arises from the roots, injuries to the cords or terminal branches would not affect the serratus anterior.
- A) Incorrect: The upper trunk gives rise to the suprascapular nerve and nerve to subclavius, not the long thoracic nerve.
- B) Incorrect: The posterior cord gives rise to thoracodorsal, axillary, and subscapular nerves, none of which affect the serratus anterior.
- D) Incorrect: The lateral cord gives rise to the lateral pectoral nerve and musculocutaneous nerve, not the long thoracic nerve.
- E) Incorrect: The musculocutaneous nerve is a terminal branch from the lateral cord and innervates the anterior arm (e.g., biceps); it does not innervate the serratus anterior.
Question 41:
Answer: D) Upper trunk
Explanation:
This classic presentation—“waiter’s tip” posture—is characteristic of Erb’s Palsy, which results from injury to the upper trunk of the brachial plexus (C5 and C6). It commonly occurs from trauma that increases the angle between the neck and shoulder. The upper trunk gives rise to nerves that innervate the deltoid, biceps, brachialis, supraspinatus, and infraspinatus, leading to loss of shoulder abduction, external rotation, and elbow flexion. Finger movements remain intact because T1 is not involved.
- A) Incorrect: The lateral cord is derived from the anterior divisions of the upper and middle trunks but is more distal; injury here would affect musculocutaneous and lateral pectoral nerves—not produce the “waiter’s tip” sign.
- B) Incorrect: The posterior cord gives rise to axillary and radial nerves, and its injury would produce wrist drop and deltoid weakness, not this pattern.
- C) Incorrect: Lower trunk injury causes Klumpke’s paralysis with intrinsic hand muscle loss and sensory deficits in the medial forearm and hand, not the upper limb posture described.
- E) Incorrect: C8 and T1 roots form the lower trunk. This is involved in Klumpke’s, not Erb’s palsy.

Question 42:
Answer: D) Dislocation of the acromioclavicular joint
Explanation:
This is a classic presentation of a shoulder separation, which refers to dislocation of the acromioclavicular (AC) joint. It occurs when the clavicle separates from the scapula due to tearing of the ligaments, often from a direct blow to the top of the shoulder (such as falling on the shoulder). A “step-off” deformity and inferior drooping of the arm when pressing downward on the shoulder are characteristic findings.
- A) Incorrect: Anterior glenohumeral dislocation presents with arm held in abduction and external rotation, often with axillary nerve involvement.
- B) Incorrect: Posterior glenohumeral dislocations are rare, typically result from seizures or electric shock, and do not produce a clavicular step-off.
- C) Incorrect: Inferior glenohumeral dislocations (luxatio erecta) present with the arm held above the head—this is not consistent with the scenario.
- E) Incorrect: Subluxation is a partial dislocation where some joint contact remains, and it typically does not produce a visible deformity or a complete step-off.
Question 43:
Answer: B) Radial nerve compression at the spiral groove of the humerus
Explanation:
The patient presents with wrist drop and sensory loss over the dorsal hand, which points to radial nerve involvement. Preservation of elbow extension suggests the injury occurred distal to the innervation of the triceps, which happens after the nerve wraps around the humerus in the spiral groove. This is consistent with radial nerve compression at the mid-humerus, commonly seen in “Saturday night palsy” from prolonged compression.
- A) Incorrect: Injury in the axilla would affect all radial nerve functions, including triceps (elbow extension), which is preserved in this case.
- C) Incorrect: Posterior interosseous nerve syndrome affects motor function only—there is no sensory loss, which this patient has.
- D) Incorrect: Median nerve injuries at the cubital fossa cause thenar atrophy and median claw / hand of benediction, not wrist drop or dorsal hand sensory loss.
- E) Incorrect: Ulnar tunnel compression causes ulnar claw and hypothenar atrophy, not wrist drop or dorsal hand numbness.
Question 44:
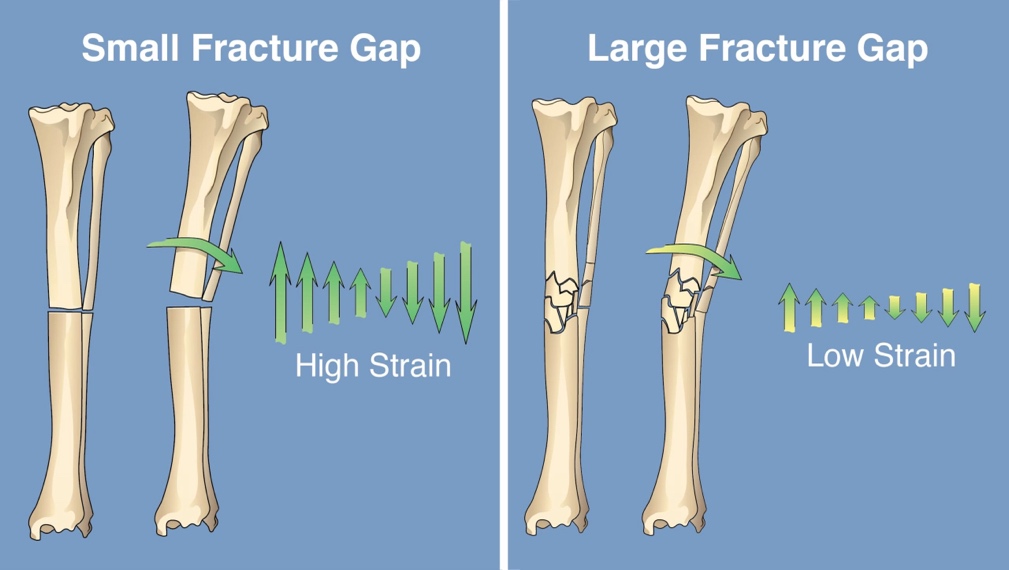
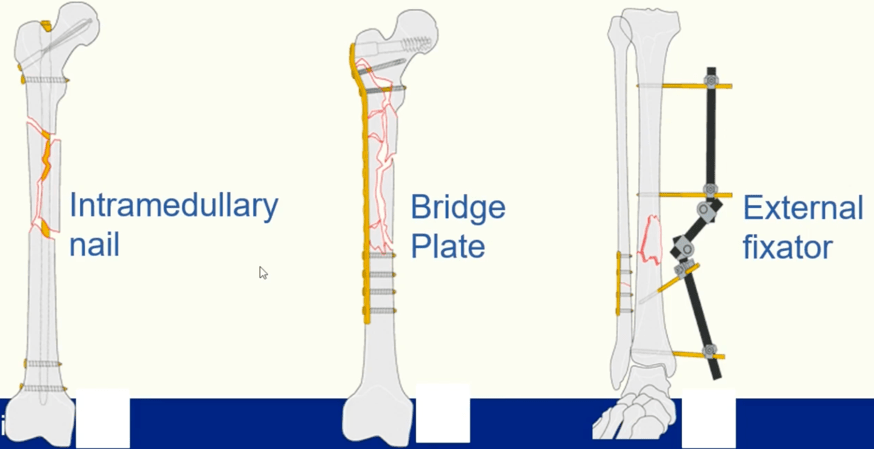
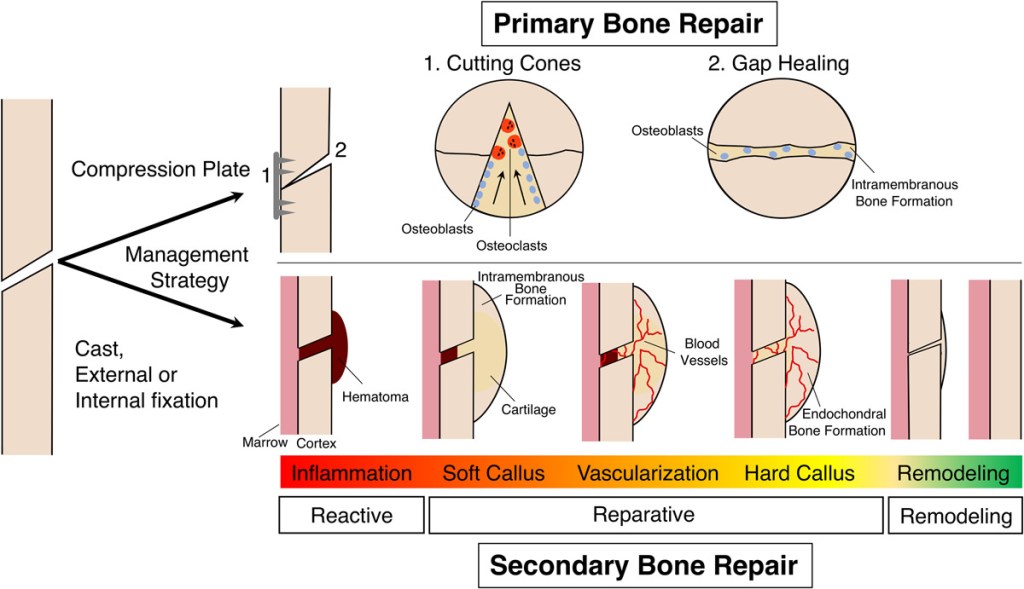
Answer: C) To prevent callus formationin a high-strain region near a joint and promote primary bone healing
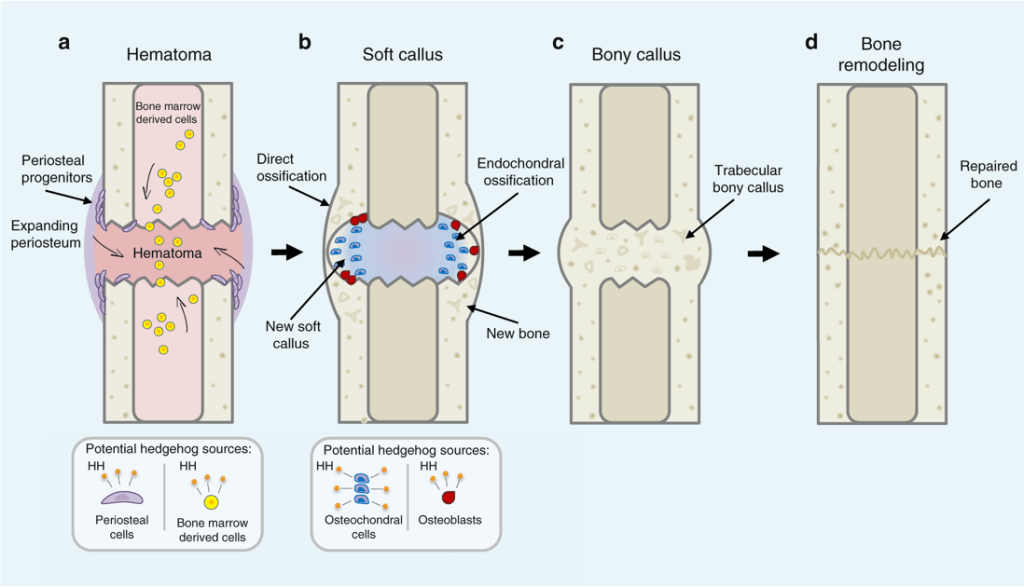
Explanation:
This is a classic example of a high-strain fracture, typically seen in 2-part intra-articular fractures where movement across the fracture can disrupt joint mobility. To preserve function (i.e. prevent reduced movement), callus formation (as seen in secondary bone healing) must be avoided. Instead, absolute stability is achieved surgically, allowing for primary bone healing via cutting cones and direct osteonal remodelling, with no callus visible on imaging.
- A) Incorrect: Periosteal callus would impede joint motion if formed in intra-articular areas.
- B) Incorrect: High-strain fractures need to be stabilised to reduce strain, not converted passively.
- D) Incorrect: Soft callus and bridging are features of secondary healing, inappropriate near joints.
- E) Incorrect: While cytokines play a role in early secondary healing, they are not central to primary healing, which avoids inflammation-mediated repair.

Question 45:
Answer: C) Bone healing through cutting cone remodelling led by osteoclasts and osteoblasts
Explanation:
This patient is undergoing primary bone healing, which occurs when absolute stability is achieved (as in ORIF with compression plating). In this scenario:
- There is no callus formation.
- Healing occurs through the cutting cone mechanism, where osteoclasts tunnel across the fracture site, followed by osteoblasts laying down new lamellar bone.
- It closely mimics normal bone remodelling.
Secondary bone healing involves several distinct stages & occurs with relative stability:
- Inflammatory phase: marked by cytokine release (IL-6, IL-1β, TNF-α) and formation of granulation tissue.
- Callus formation:
- Soft callus is formed via fibroblasts (which lay down collagen III fibres) and chondroid tissue (endochondral ossification)
- Hard callus forms deep to the soft callus via intramembranous ossification
- Remodelling: woven bone is eventually replaced with lamellar bone over months to years.
- A) Incorrect: Endochondral ossification and soft callus formation are features of secondary bone healing
- B) Incorrect: Fibrocartilaginous matrix and cytokine activity dominate early secondary healing
- D) Incorrect: Granulation tissue and soft callus are part of secondary, not primary, healing
- E) Incorrect: Woven bone formation and fibrocartilage are more relevant to secondary healing pathways
Question 46:
Answer: B) The scaphoid blood supply from the radial artery is superficial and easily compromised, risking avascular necrosis
Explanation:
The scaphoid bone has a poor blood supply, primarily from the radial artery, which travels superficially across the wrist. This vascular anatomy makes the scaphoid prone to avascular necrosis after fractures, particularly if the blood flow is disrupted. Healing is often complicated by this poor vascularisation, requiring careful management.
- A) Incorrect: The scaphoid does not have a rich periosteal blood supply; adults have centrifugal blood flow which is poorer.
- C) Incorrect: The retinacular arteries supply the femoral head, not the scaphoid.
- D) Incorrect: Adults have centrifugal blood flow in long bones, but the scaphoid’s supply is limited and superficial, increasing risk.
- E) Incorrect: The scaphoid’s vascular supply is mainly periosteal and superficial, not medullary.
Question 47:
Answer: B) ISS = 34; major trauma
Explanation:
To calculate the Injury Severity Score (ISS):
- List all AIS scores and identify the three highest from different body regions:
- Femur fracture (lower extremity) = AIS 4
- Head injury = AIS 3
- Rib fractures (thorax) = AIS 3
- Radius fracture (upper extremity) = AIS 2
- Facial laceration = AIS 1
- Select the highest three AIS values from different regions:
42 = 16 (femur)
32= 9 (head)
32= 9 (thorax) - Add the squared values:
16+9+9 = 34
Thus, ISS = 34, which is >15, classifying the patient as having major trauma.
A patient who receives a score of 6 on any body part automatically received an ISS of 75 which is dead.
Question 48:
Answer: B) Administer warming blankets and IV fluids to maintain normothermia
Explanation:
This patient is exhibiting signs of the trauma “triangle of death” — hypothermia, coagulopathy, and metabolic acidosis — which exacerbate each other in a dangerous cycle.
- The correct approach involves preventing further harm, maintaining normothermia, avoiding excessive crystalloids, transfusing blood, and providing adequate oxygenation.
- A) Incorrect: High-volume isotonic saline can dilute clotting factors, worsen coagulopathy, and lower core temperature further.
- B) Correct: Warming measures and balanced resuscitation are key to interrupting the cycle of hypothermia and coagulopathy.
- C) Incorrect: Oxygen should be administered immediately in hypoxic trauma patients to prevent worsening lactic acidosis.
- D) Incorrect: Cooling the patient worsens hypothermia and impairs coagulation.
- E) Incorrect: Crystalloids alone do not replace clotting factors or red cells, which are essential in haemorrhagic shock.
Question 49:
Answer: C) Pulmonary artery hypertension with signs of right heart failure
Explanation:
This patient’s presentation is consistent with limited cutaneous systemic sclerosis (lcSSc), especially the CREST variant:
- Calcinosis
- Raynaud’s phenomenon
- Esophageal dysmotility
- Sclerodactyly
- Telangiectasia
She displays Raynaud’s, oesophageal dysmotility, sclerodactyly, and nailfold capillary abnormalities, all suggestive of CREST syndrome.
- C) Correct: Pulmonary artery hypertension (PAH) is a late but life-threatening complication of lcSSc and often leads to right heart failure, which carries poor prognosis.
- A) Incorrect: Renal crisis is more typical of diffuse cutaneous systemic sclerosis, not limited cutaneous.
- B) Incorrect: Early lung fibrosis is more typical in diffuse scleroderma; limited cutaneous often has late pulmonary complications.
- D, E) Incorrect: These findings are more characteristic of systemic lupus erythematosus (SLE), not systemic sclerosis.
Question 50:
Answer: D) Pseudogout
Explanation:
This patient presents with an acute monoarthritis in a hospitalised patient with predisposing factors like elderly age, CKD, and being post-infection—all of which point to pseudogout.
Pseudogout is caused by deposition of calcium pyrophosphate crystals, which are rhomboid-shaped and positively birefringent on microscopy. It commonly affects larger joints like the knee, especially in elderly patients with comorbidities.
- A) Incorrect: Septic arthritis is a differential for acute monoarthritis but would typically require positive cultures, and microscopy wouldn’t show crystals.
- B) Incorrect: Gout crystals are needle-shaped and negatively birefringent, not rhomboid, or positively birefringent.
- C) Incorrect: Osteoarthritis may coexist with pseudogout but does not cause acute inflammatory flares or crystal deposition itself.
- E) Incorrect: Rheumatoid arthritis usually presents as a chronic, symmetric polyarthritis, not an isolated monoarthritis, especially acutely.


Question 51:
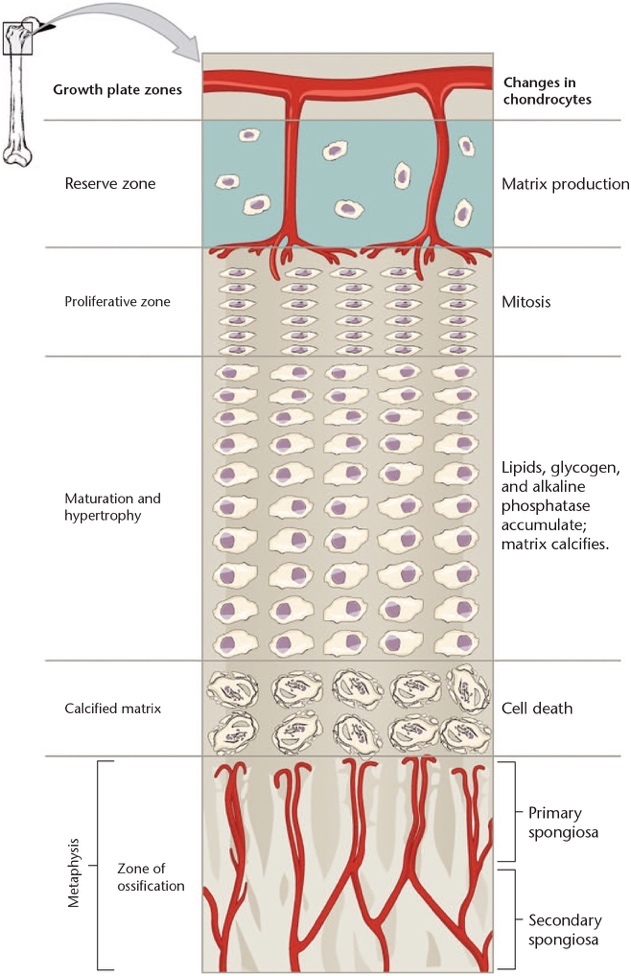
Answer: C) Hypertrophic zone
Explanation:
The hypertrophic zone of the growth plate is the most mechanically vulnerable and commonly injured in growth plate fractures, such as Salter-Harris fractures. It is responsible for the terminal differentiation of chondrocytes and matrix mineralisation, making it crucial for longitudinal bone growth.
- A) Incorrect: The resting zone contains reserve chondrocytes and is relatively quiescent. It is not the main site of growth nor the most injury-prone.
- B) Incorrect: The proliferative zone contains rapidly dividing chondrocytes but is less vulnerable than the hypertrophic zone.
- C) Correct: The hypertrophic zone is critical for matrix expansion and mineralisation and is the weakest and most commonly injured zone in growth plate trauma.
- D) Incorrect: The Grooves of Ranvier provide cellular input to the physis but are not directly involved in longitudinal growth.
- E) Incorrect: The Perichondral ring of Lacroix supports appositional growth and stability, not longitudinal elongation.
Question 52:
Answer: C) Zone of polarizing activity
Explanation:
The Zone of Polarizing Activity (ZPA) plays a crucial role in patterning the anteroposterior axis (radial to ulnar or tibial to fibular) of limb development. It secretes Sonic Hedgehog (SHH), which is essential for proper formation of structures like the radius and thumb. Disruption of this signalling can lead to radial agenesis or other anteroposterior axis defects.
- A) Incorrect: The apical ectodermal ridge (AER) regulates proximal-distal outgrowth (e.g., transverse deficiencies), not radial/ulnar specification.
- B) Incorrect: The surface ectoderm contributes to the dorsal-ventral axis (e.g., nail-patella syndrome), not radial agenesis.
- C) Correct: The ZPA controls anteroposterior limb patterning. Defects here lead to radial or ulnar agenesis.
- D) Incorrect: The perichondral ring of Lacroix supports appositional growth in the physis, not involved in early limb axis development.
- E) Incorrect: Wnt signalling is involved in dorsal-ventral axis formation, not anteroposterior.

Question 53:
Answer: C) Failure of formation (longitudinal axis)
Explanation:
This patient presents with features typical of congenital short femur with associated fibular hemimelia, hypoplastic femoral condyle, and limb shortening — all consistent with a longitudinal axis formation defect.
- A) Incorrect: Failure of segmentation involves fusion or coalition of developing parts, e.g., Apert’s syndrome with syndactyly or tarsal coalitions.
- B) Incorrect: Radial-ulnar axis defects involve radial or ulnar aplasia (e.g., VACTERL, TAR syndrome, Holt-Oram), not femoral or fibular issues.
- C) Correct: This is a longitudinal formation defect affecting the proximal-distal development of the limb, including congenital femoral deficiency and fibular absence.
- D) Incorrect: Overgrowth (e.g., hemihypertrophy) would involve asymmetric enlargement, not absence or hypoplasia.
- E) Incorrect: Amniotic band syndrome causes constriction-related deformities or autoamputation, not intrinsic bone development defects.
Question 54:
Answer: D) The lytic lesion’s location and pattern increase the risk of pathological fracture requiring surgical stabilisation
Explanation:
The proximal femur is a very common site for metastatic lesions (both lytic and sclerotic) and is mechanically important; lesions here carry a high risk of fracture, requiring prophylactic stabilisation.
- A) Incorrect: Patient age >30 and lesion appearance strongly support metastatic disease rather than primary bone tumour.
- B) Incorrect: Hypercalcemia typically accompanies osteolytic metastases due to bone resorption, not osteoblastic lesions.
- C) Incorrect: Prostate cancer metastases are mostly sclerotic, but the lesion here is clearly described as lytic and from lung cancer.
- E) Incorrect: Secondary bone tumours are unlikely under 30 years old, and the primaries vary in lesion type.
Question 55:
Answer: D) Osteoid Osteoma
Explanation:
Osteoid osteoma typically presents in adolescents with severe localised pain that worsens at night and is characteristically relieved by aspirin. Radiographically, it appears as a small, well-demarcated radiolucent lesion with a central nidus surrounded by reactive sclerosis. Increased uptake on bone scintigraphy reflects active osteoblastic activity at the lesion site.
- A) Incorrect: Simple bone cysts commonly occur in adolescents but are usually asymptomatic or present after a fracture. They appear as cold spots on bone scintigraphy and lack the classic night pain relieved by aspirin.
- B) Incorrect: Aneurysmal bone cysts are expansile and erosive lesions with multiple septations (walls), mostly seen in the metaphysis; they do not present with night pain relieved by aspirin and have different imaging features.
- C) Incorrect: Giant cell tumours occur after growth plate closure (20–40 years) and are locally aggressive, but they do not cause night pain or respond to aspirin.
- E) Incorrect: Osteosarcoma is a malignant tumour with poorly defined margins and systemic symptoms, lacking the characteristic pain pattern of osteoid osteoma.
Question 56:
Answer: C) Chondroblastoma
Explanation:
Chondroblastoma is a benign cartilage-producing tumour that characteristically arises in the epiphysis of long bones, mostly affecting adolescents aged 10–20 years. Although benign, it can expand into the metaphysis and cause local symptoms.
- A) Incorrect: Osteochondroma typically arises near joints in the metaphyseal region during childhood/adolescence but is not epiphyseal.
- B) Incorrect: Enchondroma is benign and typically located in the metaphysis within the medullary cavity, not epiphyseal.
- C) Correct: Chondroblastoma is the only tumour described as epiphyseal and common in adolescents (10–20 years).
- D) Incorrect: Chondrosarcoma is malignant, typically occurs later in life (30–60 years), and affects pelvis or femur, not predominantly epiphyseal.
- E) Incorrect: Fibrous dysplasia is a benign fibro-osseous lesion, not a cartilage-producing tumour and is usually asymptomatic.
Question 57:
Answer: B) Osteochondroma
Explanation:
Osteochondroma is a benign cartilage-capped bony tumour that typically arises near joints during childhood or adolescence, especially in bones formed through endochondral ossification. It can cause pain and limit mobility due to its location. Though mostly benign, it has a small risk of malignant transformation.
- A) Incorrect: Enchondroma is benign and usually metaphyseal, arising within the medullary cavityand rarely causes symptoms unless large enough to cause fracture.
- C) Incorrect: Chondroblastoma is epiphyseal and occurs mainly in younger patients (10-20 years old).
- D) Incorrect: Chondrosarcoma is malignant, typically occurs later in life (30-60 years), and often involves the pelvis and femur with surrounding soft tissue calcification.
- E) Incorrect: Giant Cell Tumour is benign but locally aggressive and usually occurs after growth plate closure (>20 years), mostly epiphyseal and may expand into metaphysis.
Question 58:
Answer: B) Ewing’s Sarcoma
Explanation:
Ewing’s Sarcoma is a malignant small round cell tumour of neuroectodermal origin, typically affecting children and adolescents. It often presents in the diaphysis of long bones with systemic symptoms (fever, weight loss), mimicking infection. The classic radiographic appearance is an “onion-skin” periosteal reaction due to layered periosteal bone formation.
- A) Incorrect: Osteosarcoma usually affects the metaphysis and produces osteoid; it has a “sunburst” or Codman triangle appearance.
- B) Correct: Ewing’s Sarcoma affects the diaphysis, presents with systemic signs, and has onion-skin radiography.
- C) Incorrect: Chondrosarcoma typically affects adults aged 30–60 and arises in the pelvis or femur.
- D) Incorrect: Osteomyelitis may mimic Ewing’s but usually lacks onion-skinning and histologic findings.
- E) Incorrect: Giant Cell Tumour affects the epiphysis of long bones, usually in adults >20.
Question 59:
Answer: C) Ligament
Explanation:
Ligaments connect bone to bone and stabilise joints. They are composed of non-parallel collagen bundles with elastin and proteoglycans, giving both strength and flexibility. Injuries here typically cause joint instability without affecting muscle contraction.
- A) Incorrect: Energy-storing tendons transmit muscle force e.g. Achilles tendon; injury would impact strength or recoil.
- B) Incorrect: Positional tendons provide static positioning, not joint stabilisation.
- C) Correct: Ligaments stabilise joints; tearing one (like the ACL) leads to instability.
- D) Incorrect: Aponeuroses are flattened tendons, not involved in joint stability.
- E) Incorrect: Muscle belly injury would impair strength, not cause joint instability.
Question 60:
Answer: C) It promotes intrinsic healing and improves collagen alignment
Explanation:
Early controlled mobilisation enhances intrinsic healing from the epitenon, promoting fibroblast proliferation, collagen synthesis, increased fibril diameter, and alignment along lines of tension, improving tendon function and gliding.
- A) Incorrect: Healing by granulation tissue from the endotenon leads to adhesions and poor sliding.
- B) Incorrect: Mobilisation increases collagen synthesis and alignment, not reduces it.
- C) Correct: Mobilisation supports intrinsic healing and proper collagen organisation.
- D) Incorrect: This describes immobilisation, not mobilisation.
- E) Incorrect: Mobilisation is not superior for tendon-to-bone healing; immobilisation is preferred in that context.
Question 61:
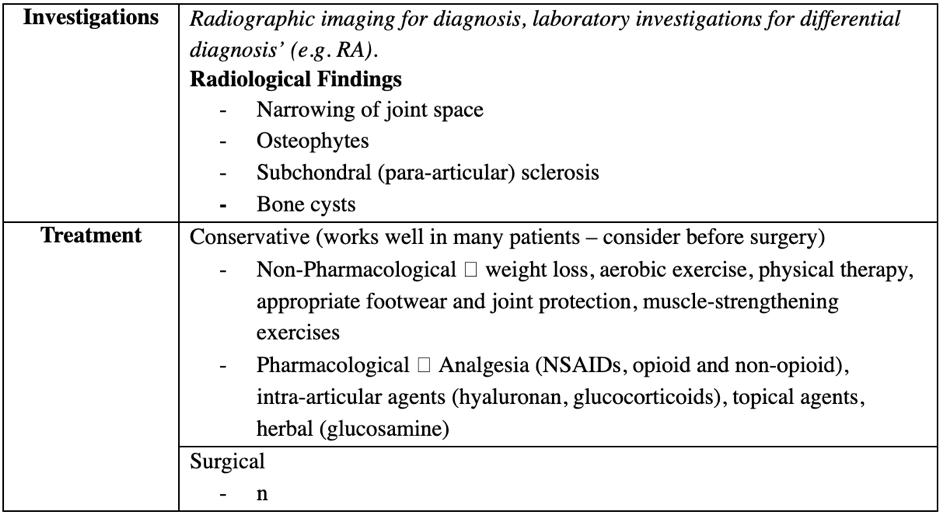
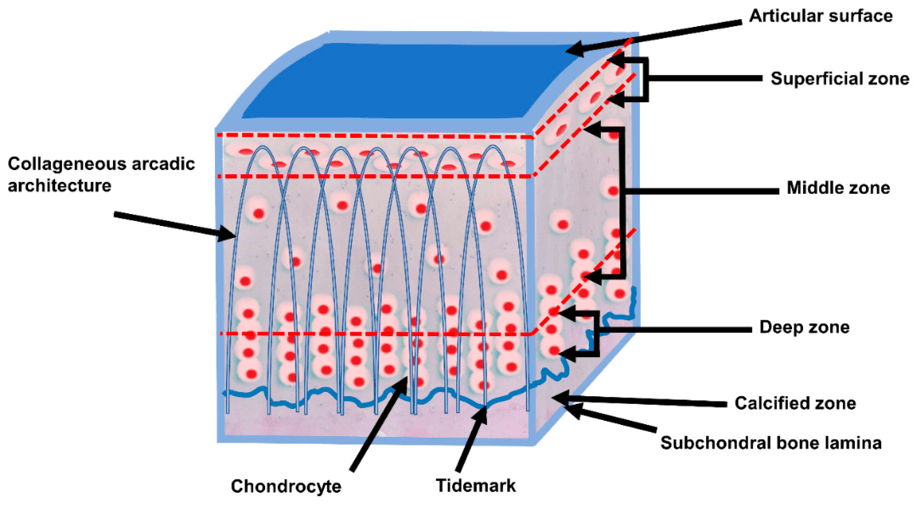
Answer: C) Degeneration of articular cartilage and subchondral bone
Explanation:
Osteoarthritis is characterised by the degeneration of articular cartilage, subchondral bone changes, and the formation of osteophytes. It results in joint space narrowing, loss of ECM components, cartilage fibrillation, and reduced resistance to compression.
- A) Incorrect: This describes rheumatoid arthritis, an autoimmune disease targeting the synovium.
- B) Incorrect: This is a feature of gout.
- C) Correct: OA primarily affects cartilage and bone, not synovium.
- D) Incorrect: Describes septic arthritis, which is infective.
- E) Incorrect: Fibrosis is not the primary issue in OA.
Question 62:
Answer: C) Bone ingrowth into porous coating for biological fixation
Explanation:
Uncemented implants coated with hydroxyapatite rely on biological fixation, where bone grows into the porous surface of the implant, securing it in place over time – allows the body to naturally incorporate the implant by growing bone into its surface. Hydroxyapatite enhances osteointegration by mimicking the mineral component of bone.
- A) Incorrect: Cemented fixation uses polymethylmethacrylate (PMMA), which is not used in this uncemented case.
- B) Incorrect: Mechanical interlock refers to cement anchoring, not applicable here.
- C) Correct: Bone ingrowth into the hydroxyapatite-coated implant surface allows stable biological fixation.
- D) Incorrect: Direct chemical bonding is not a primary fixation mechanism in orthopaedics.
- E) Incorrect: Polyethylene is used as a bearing surface, not a fixation interface.
Question 63:
Answer: D) Giant Cell Arteritis
Explanation:
Giant Cell Arteritis (GCA) is the most common vasculitis in the UK, primarily affecting patients over 50 years old, with a peak incidence around 75 years. It is more common in Northern European populationsand presents with cranial symptoms such as temporal headache, jaw claudication, and visual disturbances (e.g., amaurosis fugax, which can progress to permanent vision loss). GCA involves granulomatous inflammation of large and medium-sized arteries, especially the cranial branches of the carotid artery, and is associated with high ESR/CRP levels.
Biopsy shows granulomatous inflammation with multinucleated giant cells, and pathology includes vessel wall thickening, inflammatory infiltration, and endothelial damage, leading to thrombus formation and downstream ischaemia. Untreated, GCA can result in stroke, TIA, or irreversible blindness.
Treatment involves high-dose corticosteroids, often followed by immunosuppressive therapy to induce remission. Education and early intervention are crucial due to the risk of serious complications.
- A) Incorrect: Granulomatosis with Polyangiitis (GPA) is an ANCA-associated small vessel vasculitis more likely to affect the upper and lower respiratory tract and kidneys.
- B) Incorrect: Takayasu Arteritis presents in younger patients (<40) and is more common in Asian populations, primarily involving the aorta and its branches.
- C) Incorrect: Behçet’s Disease is more common along the Silk Road (e.g., Turkey, Saudi Arabia), and typically presents with oral/genital ulcers, uveitis, and acneiform rashes, not cranial ischaemic symptoms.
- E) Incorrect: Polyarteritis Nodosa affects medium-sized arteries, often with multisystem involvement, but it does not characteristically involve cranial arteries or present with jaw claudication or vision loss.
Question 64:
Answer: B) Increased Q-angle causing lateral patellar pull
Explanation:
The Q-angle, named after the quadriceps femoris muscle, measures the angle between the long axis of the femur (ASIS to patella) and the straight axis of the femur (tibial tuberosity through the centre of the patella). It reflects the lateral pull of the quadriceps on the patella, which is a sesamoid bone within the quadriceps tendon.
A greater Q-angle, commonly seen in females (15-18°) due to wider hips, increases the lateral force on the patella, making it prone to lateral displacement or dislocation. This is usually resisted by the lateral epicondyle and the vastus medialis muscle.
Strengthening the vastus medialis helps prevent lateral dislocation.
Valgus deformity (genu valgum) increases the Q-angle, while varus deformity (genu varum) decreases it.
- A) Incorrect: Decreased Q-angle results in less lateral pull, not medial pull, and is not associated with lateral dislocation.
- C) Incorrect: The patella sits within the quadriceps tendon and is normally aligned centrally unless displaced laterally.
- D) Incorrect: Strengthening vastus lateralis would increase lateral pull; strengthening vastus medialis helps prevent dislocation.
- E) Incorrect: Varus deformity decreases the Q-angle and is associated with decreased lateral displacement.
Question 65:
Answer: C) Hallux Valgus
Explanation:
Hallux Valgus, commonly known as a ‘bunion,’ is characterised by lateral deviation and subluxation of the first metatarsophalangeal joint. The sesamoid bones may also be laterally displaced. It is often caused by abnormal weight distribution onto the distal foot, frequently exacerbated by wearing high-heeled shoes, which force weight onto the forefoot unevenly.
- A) Incorrect: Hammer Toe is a contracture deformity affecting the 2nd to 5th toes (due to flexion of proximal interphalangeal joint), caused by muscle-tendon imbalance and often due to poorly fitting shoes; it results in corns on the proximal and middle phalanx, not at the big toe.
- B) Incorrect: Claw Toe affects multiple toes (2nd to 5th) with a characteristic bending up at the base and downward at the middle and tip, often related to nerve damage or systemic conditions like diabetes.
- D) Incorrect: Congenital Clubfoot is an inversion (varus) deformity present at birth, caused by short tendons and often associated with bone deformities, not acquired lateral deviation.
- E) Incorrect: Metatarsalgia refers to pain in the metatarsal region but does not involve joint subluxation or deformity.
Question 66:
Answer: C) Tricyclic antidepressants (e.g., amitriptyline)
Explanation:
Fibromyalgia is a chronic disorder characterised by widespread pain, fatigue, and neurological symptoms related to central sensitisation and disordered pain processing. The main pharmacological treatments include simple analgesics and medications that modulate the nervous system, such as tricyclic antidepressants (e.g., amitriptyline) and anticonvulsants (e.g., gabapentin). These drugs help manage pain and improve sleep quality. Opioids and anti-inflammatory agents are generally not recommended due to lack of efficacy and risk of harm.
- A) Incorrect: Long-term opioids are discouraged in fibromyalgia due to poor efficacy and risk of dependence.
- B) Incorrect: NSAIDs are not effective in fibromyalgia as there is no primary inflammatory pathology.
- C) Correct: Tricyclic antidepressants like amitriptyline are the main pharmacological option, targeting central pain modulation and improving symptoms.
- D) Incorrect: Systemic corticosteroids are not indicated as fibromyalgia is not an inflammatory disease.
- E) Incorrect: DMARDs are used for inflammatory arthritides and have no role in fibromyalgia.
Question 67:
Answer: B) Bisphosphonates
Explanation:
Osteoporosis is a metabolic bone disease characterised by low bone mass and microarchitectural deterioration, leading to increased fracture risk. It is common in postmenopausal females due to rapid decline in bone mass after menopause. Diagnosis is confirmed by a T-score below -2.5 on DXA scan.
Bisphosphonates are the first-line anti-resorptive agents that inhibit osteoclast-mediated bone resorption, thereby increasing bone density and reducing fracture risk. They are widely used and effective in postmenopausal osteoporosis.
- A) Incorrect: Teriparatide is a humanised parathyroid hormone reserved for severe cases or patients intolerant to bisphosphonates & with a high change of fractures.
- C) Incorrect: Romosozumab is a newer anabolic agent (anti-sclerostin antibody) used in specific cases but not first-line.
- D) Incorrect: Denosumab (anti-RANKL antibody) is also an anti-resorptive agent, often used if bisphosphonates are contraindicated or not tolerated, but not generally initial therapy.
- E) Incorrect: Calcium and vitamin D supplementation are important adjuncts but alone are insufficient as primary pharmacological treatment for established osteoporosis.
Additional points:
- Osteoporosis involves decreased bone formation and increased bone resorption, with a switch from osteogenesis to adipogenesis in bone marrow.
- Peak bone mass is a key predictor, with females achieving lower peak bone mass than males and experiencing rapid postmenopausal decline.
- Hip fractures have high morbidity and mortality, emphasizing the importance of effective treatment.
Question 68:
Answer: B) Paget’s Disease of Bone
Explanation:
Paget’s Disease is a disorder of bone remodelling characterised by focally increased and disorganised bone turnover, driven by abnormal osteoclast activity followed by haphasard osteoblast activity producing poor quality woven bone. It commonly affects older adults (>55 years) and often presents with bone pain, deformity, and pathological fractures.
The “blade of grass / cotton wool” appearance on X-ray is a classic early radiological sign representing osteolytic lesions (osteoporosis circumscripta), followed by osteosclerosis and bone expansion in later stages.
Elevated alkaline phosphatase (ALP) with normal calcium and phosphate is typical, reflecting increased bone turnover without systemic calcium/phosphate disturbance.
Clinical features often include bone pain, deformities, deafness, and rarely secondary osteosarcoma.
The tibia is a common site and involvement may be focal with adjacent bones spared.
- A) Incorrect: Osteoporosis shows decreased bone density diffusely without characteristic X-ray features or elevated ALP.
- C) Incorrect: Osteomalacia involves defective mineralisation with low vitamin D, bone softening, and Looser’s zones on imaging.
- D) Incorrect: Metastatic bone disease usually presents with multiple lesions, often destructive, and abnormal serum calcium.
- E) Incorrect: Multiple myeloma features lytic “punched-out” lesions, anaemia, hypercalcemia, and paraproteinemia.
Question 69:
Answer: C) Osteomalacia
Explanation:
Osteomalacia is a disorder of defective mineralisation of newly formed bone matrix (osteoid), leading to soft bones. It is commonly caused by vitamin D deficiency or phosphate depletion.
Typical biochemical findings include low or low-normal serum calcium and phosphate, elevated alkaline phosphatase due to increased bone turnover, and secondary hyperparathyroidism (raised PTH).
Radiological signs include Looser’s zones (pseudofractures), typically found in ribs, femur, and pubic rami.
Patients often complain of bone pain, tenderness (especially anterior tibia and sternum), muscle weakness, and fractures.
Causes include vitamin D deficiency (due to malabsorption, liver/kidney disease, drugs), phosphate depletion, and mineralisation inhibitors like aluminium.
- A) Incorrect: Osteoporosis is decreased bone density without defective mineralization or pseudofractures.
- B) Incorrect: Paget’s Disease shows focal bone remodelling with elevated ALP but normal calcium/phosphate and characteristic X-ray changes.
- D) Incorrect: Rheumatoid arthritis causes joint inflammation but not metabolic bone disease.
- E) Incorrect: Fibromyalgia causes chronic pain but no bone or biochemical abnormalities.
Question 70:
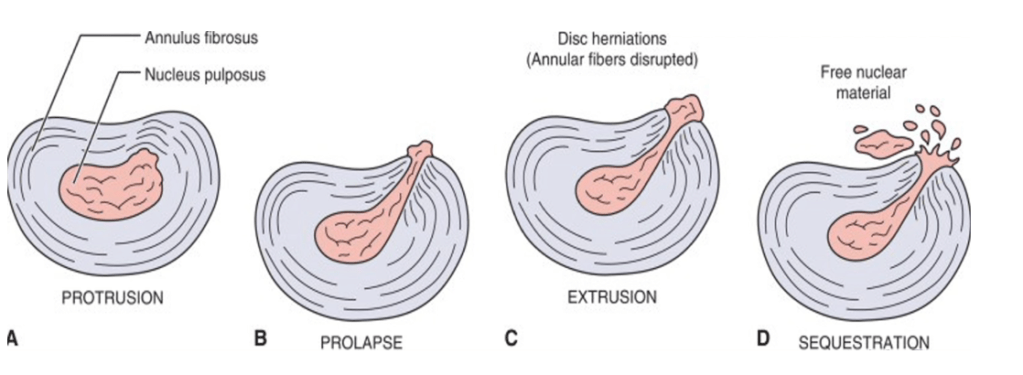
Answer: B) Nuclear extrusion
Explanation:
Nuclear extrusion refers to a complete split of the annulus fibrosus with nuclear material leaking out beyond the annulus but still remaining attached to the disc. This can cause nerve root irritation or compression.
- A) Incorrect: Disc protrusion (bulging) involves rupture of the nucleus causing distortion of only the outermost annular fibres without full annular rupture.
- B) Correct: Nuclear extrusion is when nuclear material leaks out but remains attached.
- C) Incorrect: Sequestered nucleus occurs when the extruded nucleus is no longer attached and may float freely in the spinal canal, potentially causing chemical irritation even without direct nerve compression.
- D) Incorrect: Annular tear without herniation involves a tear in the annulus without nuclear material herniating out.
- E) Incorrect: Spinal stenosis is narrowing of the spinal canal, which may or may not be caused by disc herniation.
Question 71:
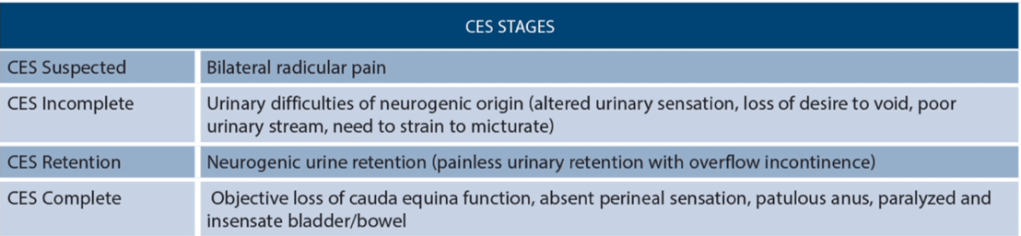
Answer: B) Incomplete CES (CESI); emergency decompression within 48 hours
Explanation:
Incomplete CES (CESI) presents with bilateral leg symptoms, altered perianal sensation, and difficulty voiding or unawareness of bladder dysfunction. It requires emergency surgical decompression within 48 hours to maximise chances of recovery; approximately 75% of patients can return to normal function if treated promptly.
- A) Incorrect: Early CES (CESE) shows unilateral leg symptoms and altered perianal sensation but no bladder dysfunction yet; it requires prompt diagnosis and monitoring, not immediate surgery.
- C) Incorrect: Retention CES (CESR) involves complete urinary retention and bilateral symptoms; urgent decompression is needed immediately, but this patient still can initiate urination.
- D) Incorrect: Spinal cord infarction is a different pathology with different management.
- E) Incorrect: Peripheral neuropathy does not cause acute bilateral leg pain with perianal numbness and bladder dysfunction
Question 72:
Answer: C) Septic arthritis; synovial fluid aspiration
Explanation:
This child presents with the classic features of septic arthritis: inability to weight bear, high fever (>39°C), elevated ESR and WBC count, and acute hip pain. The gold standard investigation is synovial fluid aspiration. Synovial WCC >50,000 indicates infection.
- A) Incorrect: JIA usually has a more chronic presentation without high fever or acute refusal to weight bear.
- B) Incorrect: Osteomyelitis is possible but usually presents with more bone tenderness; MRI would help more.
- D) Incorrect: Transient synovitis is common in this age group but lacks systemic features like fever >39°C, history of viral infection and high inflammatory markers.
- E) Incorrect: Crystal arthropathy is more common in adults, not children.
Question 73:
Answer: C) Staphylococcus; biofilm formation
Explanation:
Peri-Prosthetic Joint Infection (PPJI) is a rare but serious complication of joint replacement surgery, occurring in <1% of cases. Staphylococci are the most common pathogens, responsible for 56% of infections. Risk factors include revision surgery, high BMI, poorly controlled diabetes, immunosuppression, male sex, smoking, and malnutrition.
What makes PPJI particularly difficult to treat is that the bacteria adopt a sessile phenotype (as opposed to planktonic), adhering to the prosthesis and producing a biofilm. This biofilm protects the bacteria from both immune surveillance and antibiotic penetration, necessitating aggressive intervention.
Early infections typically occur within 3 weeks post-op, while late infections may appear years later, often via haematogenous spread (e.g., following a dental or GI procedure).
Management includes:
- Early identification via clinical assessment + aspiration before antibiotics.
- Massive debridement, possibly requiring radical surgery or re-implantation.
- Long-term antibiotics may be used in non-surgical candidates, but they control symptoms without eradicating infection.
- Beware of C. difficile as a complication from prolonged antibiotic therapy.
- A) Incorrect: DVT is a possible complication but unrelated to infection cause.
- B) Incorrect: Pseudomonas is less common and haematogenous spread is more typical of late infections.
- D) Incorrect: Immune complex deposition is more typical of glomerulonephritis, not PPJI.
- E) Incorrect: E. coli is not a common pathogen in PPJI.
Question 74:
Answer: C) Enthesitis with subsequent bone marrow oedema, fat metaplasia, and aberrant osteogenesis
Explanation:
Ankylosing spondylitis (AS) is a seronegative, HLA-B27-associated spondyloarthropathy characterised by inflammation not driven by autoantibodies, but by auto-inflammatory mechanisms centred around the entheses (the sites of ligament/tendon insertion to bone).
The disease process begins with enthesitis, leading to:
- Bone marrow oedema adjacent to the enthesis
- Fat deposition following oedema
- Bone erosion (via Cathepsin K and MMP1)
- New bone formation through BMP and Wnt signalling, forming syndesmophytes, contributing to fusion (e.g., bamboo spine)
Osteopenia and osteoporosis are common in long-standing AS, due to chronic inflammation and decreased physical activity, increasing risk for vertebral fractures with minor trauma.
This patient’s dyspnoea may relate to costovertebral/costosternal enthesitis, limiting chest expansion — a classic feature of advanced AS.
- A) Incorrect: AS is sero-negative; there is no prominent autoantibody involvement.
- B) Incorrect: While TNF-alpha is important, this answer neglects the sequence from enthesitis to ossification.
- D) Incorrect: Immune complex deposition is seen in lupus or post-infectious glomerulonephritis.
- E) Incorrect: Granulomatous inflammation is seen in TB or sarcoidosis, not AS.
Question 75:
Answer: D) Bilateral sacroiliitis on imaging
Explanation:
According to the Modified New York Criteria, the diagnosis of ankylosing spondylitis requires radiologic evidence plus at least one clinical criterion. In this case, the bilateral sacroiliitis (grade ≥2) on MRI is the definitive diagnostic feature when combined with this patient’s symptoms of inflammatory back pain and reduced spinal mobility.
Although HLA-B27 is supportive, it is not diagnostic on its own. Similarly, anterior uveitis and AV block are recognised extra-articular manifestations, but they are non-specific. Clinical features such as decreased chest expansion and spine motion are supportive, but the radiologic confirmation is what fulfils the diagnostic threshold.
- A) Incorrect: HLA-B27 is present in many healthy individuals; not diagnostic.
- B) Incorrect: While typical, these features alone are insufficient for diagnosis.
- C) Incorrect: Part of clinical criteria, but not sufficient without imaging.
- E) Incorrect: Suggestive of spondyloarthropathy, but not diagnostic of AS.
Question 76:
Answer: E) Microfracture technique to induce bleeding
Explanation:
Articular cartilage is avascular, aneural, and alymphatic, making spontaneous healing unlikely, especially for superficial injuries that remain above the tidemark. These defects do not access the subchondral bone’s vasculature and hence lack the ability to mount a repair response.
To address this, the microfracture technique is used, which artificially breaches the tidemark, inducing a controlled deep injury that allows marrow-derived mesenchymal stem cells to infiltrate the lesion and form fibrocartilage.
- A) Incorrect: High tibial osteotomy is used for joint malalignment or advanced cartilage loss to reduce mechanical load on the joint.
- B) Incorrect: Total joint replacement is for end-stage osteoarthritis, not focal superficial injuries.
- C) Incorrect: ACI requires healthy cartilage harvest and lab expansion, and is usually reserved for larger or deeper lesions.
- D) Incorrect: Conservative management is insufficient for persistent, symptomatic full-thickness lesions.
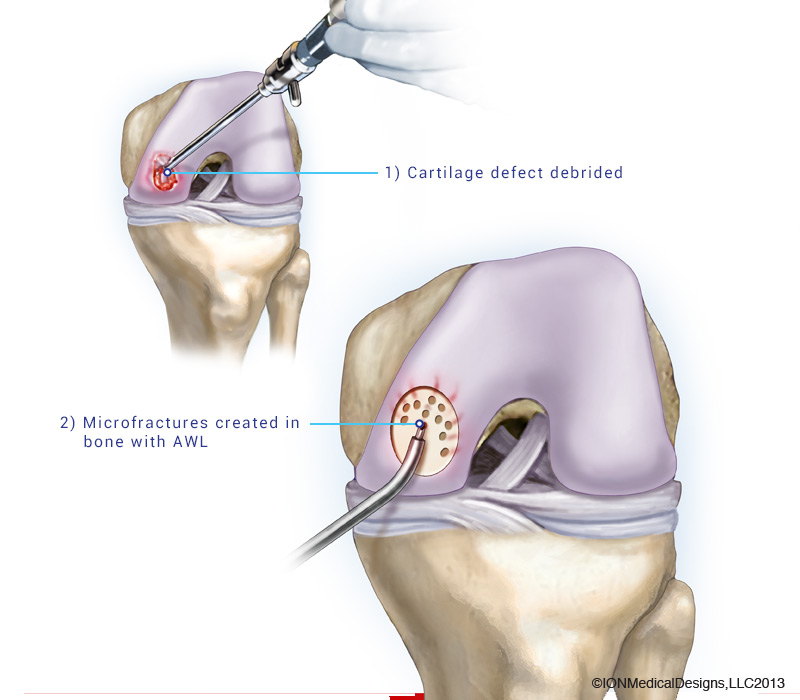
Question 77:
Answer: C) Stage 3; core decompression or osteotomy
Explanation:
This patient shows classical findings of subchondral collapse on imaging (crescent sign) without joint space narrowing or secondary degenerative changes — consistent with Ficat Stage 3.
- Ficat Stage 3: Defined by structural failure of subchondral bone, often visible as the crescent sign. Cartilage is still largely intact but at high risk of collapse.
- Management aims at joint preservation in younger patients — options include:
- Core decompression (relieve intraosseous pressure)
- Osteotomy (redistribute load)
Imaging-to-stage mapping:
- Stage 1: MRI changes only, normal X-ray
- Stage 2: Sclerosis/cystic changes on X-ray, no collapse
- Stage 3: Subchondral collapse
- Stage 4: Joint space narrowing and secondary osteoarthritis
- A) Incorrect: Bisphosphonates may slow progression but are not definitive at Stage 3.
- B) Incorrect: Physiotherapy alone is insufficient in the presence of collapse.
- D) Incorrect: Arthroplasty is reserved for Stage 4 with secondary OA.
- E) Incorrect: Hip resurfacing is not suitable in structurally unstable heads.
