
Neurology Answers (Y2)
Question 1)
Answer: A
Explanation: Spina bifida occulta is the mildest form of spina bifida. It involves a small defect in the vertebrae, usually without visible signs like a cyst or bump. The skin may appear normal, or there may be a small dimple or patch of hair.
B is incorrect as Spina bifida cystica is a more severe form with a visible cyst or sac protruding through the spine.
C is incorrect as Encephalocele is a defect in the skull, not the spine, where brain tissue can protrude.
D is incorrect as Meningocele involves a protrusion of the meninges through the spinal defect, usually visible as a cyst.
E is incorrect as Duane’s syndrome is a congenital eye movement disorder that affects the abducens nerve and its ability to abduct the eye, it is not related to the spine.
Question 2)
Answer: B
Explanation: Duane’s syndrome is a congenital disorder where there is abnormal development of the sixth cranial nerve (abducens nerve), leading to limited ability to move the eye outward (abduction).
A is incorrect as Amblyopia (lazy eye) is a developmental issue where vision in one eye is reduced but doesn’t affect eye movement.
C is incorrect as Strabismus (also known as having a squint) is a general term for misalignment of the eyes, but it doesn’t specifically involve cranial nerve abnormalities.
D is incorrect as Cortical heterotopia is a neuronal migration disorder affecting the brain whereby neurons are in the wrong place in the cortex with the most common symptom being epilepsy, it is unrelated to eye movement.
E is incorrect as Syringomyelia is a cyst formation in the spinal cord, affecting sensory and motor functions, not eye movement.
Question 3)
Answer: D
Explanation: The ventricular zone is the primary site of neurogenesis during brain development. Neural progenitor cells divide and give rise to neurons and glial cells here. The ventricular zone is like a neuron factory, making new brain cells during early development. That’s why it’s the primary area responsible for neuron generation. Once neurons are made, they start to move away from the ventricular zone. The subventricular zone is a layer where some additional cell division happens. It’s like a second, smaller factory for brain cells. Neurons continue to move up into this layer, called the intermediate zone, as they are preparing to reach their destination. As neurons keep moving, they eventually reach the marginal zone (the outermost part). This is where neurons connect and start forming the outer layer of the brain (the cortex). Neurons that have travelled through the other layers eventually settle in the cortical plate, where they will become part of the cerebral cortex (the thinking part of the brain).This is where neurons will start to organize themselves and connect with other neurons to form the brain’s circuits.
A is incorrect as the marginal zone is a thin layer that contributes to the formation of the outermost layer of the brain, not neurogenesis.
B is incorrect as the intermediate zone is where newly formed neurons migrate through, but it’s not where they are generated.
C is incorrect as the subventricular zone does generate neurons, but this primarily happens postnatally and in some adult neurogenic regions.
D is incorrect as the cortical plate is where neurons settle after migrating, but it doesn’t produce neurons.

Question 4)
Answer: A
Explanation: Focal epilepsy refers to seizures that originate from a specific part of the brain. These seizures can be secondary (the result of an abnormality) or cryptogenic (without a known cause).
B is incorrect as Generalized epilepsy involves seizures affecting both hemispheres of the brain simultaneously, not from a specific area.
C is incorrect as Cryptogenic epilepsy is a term used when the cause of epilepsy is unknown but suspected to be present.
D is incorrect as secondary epilepsy refers to seizures caused by an identifiable lesion (e.g., tumour or stroke), but this question specifies no abnormality.
E is incorrect as idiopathic epilepsy is typically genetic and generalized, not focal.
Question 5)
Answer: B
Explanation: Botulinum toxin blocks the release of acetylcholine at the neuromuscular junction, leading to flaccid paralysis. It is used clinically in small doses for muscle spasticity and cosmetic purposes.
A is incorrect as Tetanus toxin prevents the release of inhibitory neurotransmitters, leading to spastic paralysis.
C is incorrect as Saxitoxin is a neurotoxin from algae that blocks sodium channels, leading to paralysis, but it doesn’t affect acetylcholine directly.
D is incorrect as Dendrotoxin blocks potassium channels, affecting action potentials but not acetylcholine release.
E is incorrect as Curare blocks acetylcholine receptors on the muscle, preventing acetylcholine from acting but not stopping its release.
Question 6)
Answer: C
Explanation: The trigeminal nerve (cranial nerve V), specifically the ophthalmic branch (V1), is responsible for sensory innervation of the cornea. Damage to this nerve can result in loss of corneal sensation, increasing the risk of corneal injury.
A is incorrect as the optic nerve (cranial nerve II) is responsible for vision, not corneal sensation.
B is incorrect as the facial nerve (cranial nerve VII) controls facial muscles and lacrimation, but not corneal sensation.
D is incorrect as the oculomotor nerve (cranial nerve III) controls eye movement, not sensation.
E is incorrect as the abducens nerve (cranial nerve VI) controls the lateral rectus muscle, allowing the eye to move outward, but not sensation.
Question 7)
Answer: E) Vitreous humour
Explanation: Vitreous humour is the gel-like substance inside the eyeball, responsible for maintaining the eye’s shape. It has no role in tear production or drainage.
A is incorrect as the lacrimal gland produces tears.
B is incorrect as the trigeminal nerve (V1 branch) provides sensory input that stimulates tear production.
C is incorrect as the lacrimal puncta are small openings that drain tears from the surface of the eye into the nasolacrimal duct.
D is incorrect as the nasolacrimal duct drains tears into the nasal cavity.
Question 8)
Answer: (C) Lewis-Sumner Syndrome: This is a common variant of CIDP characterized by asymmetric involvement of the arms, which differentiates it from typical CIDP.
Explanation:
A is incorrect as Multifocal Motor Neuropathy (MMN) is a distinct disorder from CIDP. While both are immune-mediated neuropathies, MMN affects only motor nerves, whereas CIDP typically affects both motor and sensory nerves.
B is incorrect as Diabetic neuropathy is a common complication of diabetes and is not considered a variant of CIDP. It is a metabolic neuropathy, not an inflammatory one.
D is incorrect as Guillain-Barré Syndrome (GBS) is an acute demyelinating disorder that occurs following an infection, whereas CIDP is chronic. They are related but not variants of each other.
E is incorrect as Myasthenia Gravis is a neuromuscular junction disorder whereby the immune system attacks Acetylcholine channels preventing Ach from binding, it is not a peripheral nerve disease.
Question 9)
Answer: E) Apathy
Explanation: Apathy is a negative symptom characterized by a lack of motivation or interest. Negative symptoms are a lack or reduction of normal habits whereas positive symptoms are symptoms not found in people without a psychosis.
A is incorrect as hallucinations are positive symptoms, not negative.
B is incorrect as delusions are also positive symptoms associated with distorted perceptions of reality.
D is incorrect as euphoria is not a symptom of schizophrenia but may be associated with bipolar disorder or bipolar depression whereby a person alternates between low mood and mania.
E is incorrect as insomnia is a sleep disorder and not specifically a symptom of schizophrenia.
Question 10)
Answer: B) Pons
Explanation: Locked-in syndrome occurs due to damage to the pons, affecting motor control while leaving cognitive function intact.
A is incorrect as damage to the medulla can lead to other types of neurological deficits but is not specifically related to locked-in syndrome.
C is incorrect as the cerebellum is involved in coordination and balance, not primarily motor control.
D is incorrect as the thalamus relays sensory and motor signals but does not control voluntary movement like the pons does.
E is incorrect as the hippocampus is primarily involved in memory and not motor control.
Question 11)
Answer: C) A condition characterized by a combination of ptosis, miosis, and anhidrosis
Explanation: Horner’s Syndrome results from damage to the sympathetic nerve pathway supplying the eye. This leads to three classic signs:
- Ptosis: drooping of the upper eyelid
- Miosis: constriction of the pupil
- Anhidrosis: lack of sweating on the affected side of the face
A is incorrect as it describes movement disorders that could be due to facial nerve damage, not Horner’s.
B is incorrect as it describes Bell’s palsy or similar conditions affecting facial muscles.
D is incorrect Horner’s syndrome is a neurological problem and does not impact the respiratory system.
E is incorrect as although strokes can cause various syndromes, Horner’s specifically relates to sympathetic nerve damage.
Question 12)
Answer: B) Upper motor neuron lesion
Explanation: Upper motor neuron lesions result in increased muscle tone and spasticity due to loss of inhibition from higher brain centres. This often leads to characteristic patterns of muscle tightness.
A is incorrect as lower motor neuron lesions cause weakness and decreased tone.
C is incorrect as neuromuscular junction disorders lead to muscle weakness, not increased tone.
D is incorrect as peripheral neuropathy typically presents with sensory loss or weakness, not spasticity.
E is incorrect as myopathy results in muscle weakness but does not usually cause spasticity.
Question 13)
Answer: A) Maintenance of consciousness and arousal
Explanation: The reticular formation is a network of neurons located in the brainstem that plays a crucial role in regulating arousal and consciousness. It helps determine alertness and the sleep-wake cycle. Damage to the reticular formation can cause a coma
B is incorrect as heart rate regulation is mainly managed by the autonomic nervous system and specific brain areas like the medulla oblongata, not exclusively by the reticular formation.
C is incorrect as muscle movement is primarily controlled by the motor cortex and spinal cord.
D is incorrect as sensory information processing occurs in the thalamus and parietal lobe.
E is incorrect as coordination of voluntary movements is primarily a function of the cerebellum and motor pathways.
Question 14)
Answer: B) Hallucinations
Explanation: Hallucinations, especially auditory (hearing voices), are considered a positive symptom because they reflect an “addition” to normal function, where the person experiences sensations that are not real. Negative symptoms are normal are experiences (don’t include a loss of reality) but they are reduced in Schizophrenia
A is incorrect as Apathy is a negative symptom, indicating a lack of motivation or emotional response, reflecting a “loss” of normal function.
C is incorrect as Withdrawal into self is a negative symptom, representing social withdrawal and lack of engagement.
D is incorrect as reduced motivation is also a negative symptom, where the person shows a decreased drive to do daily activities.
E is incorrect as Anhedonia is the inability to feel pleasure, also a negative symptom of schizophrenia, not a positive one like hallucinations.
Question 15)
Answer: E) Benzodiazepines
Explanation: Benzodiazepines (e.g., diazepam, lorazepam) are highly effective and works almost immediately by increasing levels of GABA (an inhibitory neurotransmitter) that counteracts the effects of adrenaline in treating anxiety but carries a significant risk of dependence and addiction. This is why they are only used for short-term or acute anxiety treatment.
A is incorrect as SSRIs although they are commonly used to treat anxiety, they take weeks to show their effects and are not addictive, they are also more effective in depression where serotonin is reduced.
B is incorrect as SNRIs like SSRIs, SNRIs are used for anxiety but are not associated with a risk of addiction.
D is incorrect as Beta-blockers such as propranolol, are used for physical symptoms of anxiety (e.g., tremors, rapid heartbeat) but are not addictive.
E is incorrect as Antipsychotics are used in certain psychiatric conditions, including in schizophrenia and severe anxiety, but they are not first-line treatment and are not known for causing addiction.
Question 16)
Answer: B) Dysphagia and loss of pain/temperature sensation on the ipsilateral side of the face
Explanation: Wallenberg syndrome is caused by a stroke in the lateral medulla, affecting structures like the nucleus ambiguous (causing dysphagia) and the spinal trigeminal nucleus (leading to ipsilateral facial sensory loss).
A is incorrect as Hemiparesis on the contralateral side would result from damage to the motor tracts, typically seen in medial, not lateral medullary syndromes.
C is incorrect as Complete loss of consciousness would suggest a diffuse or bilateral brain injury for example to the reticular formation, which is involved in consciousness, not localized medullary damage.
D is incorrect as Quadriplegia involves paralysis of all four limbs and is not typically caused by damage to the lateral medulla but maybe by a peripheral neuropathy such as Guillain Bare Syndrome.
E is incorrect as Inability to speak issues may occur in strokes, but the hallmark of Wallenberg syndrome is dysphagia and sensory loss.
Question 17)
Answer: C) Bone breakdown exceeding formation
Explanation: In prolonged immobility, there is an imbalance where bone resorption occurs more than bone formation, leading to the release of calcium into the bloodstream. The other causes listed are possible but not the primary mechanism in the context of immobility.
Question 18)
Answer: B) Lateral Medullary Syndrome (Wallenberg syndrome)
Explanation: Wallenberg syndrome is caused by a stroke in the lateral medulla and is characterized by symptoms such as dizziness (vertigo), dysphagia (difficulty swallowing), and sensory deficits on the face (right-sided numbness in this case).
A is incorrect as Locked-in syndrome occurs with lesions in the pons, leading to complete paralysis except for vertical eye movements, not dizziness or swallowing difficulties.
C is incorrect as Internuclear ophthalmoplegia primarily affects eye movements and does not typically cause dysphagia or facial numbness.
D is incorrect as Spinal shock results in a loss of reflexes and motor function but is not specific to brainstem lesions.
E is incorrect Multiple sclerosis can present with diverse neurological symptoms but typically involves lesions in various areas of the CNS rather than being localized like in Wallenberg syndrome.
Question 19)
Answer: A) Horner’s Syndrome
Explanation: Horner’s Syndrome results from disruption of the sympathetic nerves supplying the eye, leading to the classic triad of ptosis, miosis, and anhidrosis. It can occur due to various causes, including trauma, tumours, or vascular issues.
B is incorrect as Oculomotor nerve palsy involves a different set of symptoms, typically including ptosis and an eye that is down and out, but it does not cause miosis (the pupil may be dilated).
C is incorrect as Myasthenia gravis can cause ptosis but typically does not produce the specific combination of miosis and anhidrosis.
D is incorrect as Guillain-Barré syndrome affects peripheral nerves and is associated with muscle weakness but does not cause the symptoms specific to Horner’s syndrome.
E is incorrect as Brown-Séquard syndrome is characterized by hemi section of the spinal cord leading to weakness and sensory loss on one side of the body and loss of pain and temperature sensation on the opposite side, not affecting pupillary responses.
Question 20)
Answer: C) Beta-amyloid is crucial in triggering the Alzheimer’s process, while tau is important for its progression.
Explanation: Beta-amyloid is a protein that can form clumps, called plaques, outside neurons. These plaques may trigger abnormal processes that lead to the loss of synapses (connections between neurons) through a process called “pruning.” Beta-amyloid plaques may be involved in the early stages of Alzheimer’s but do not directly predict severity of symptoms. Tau is a protein that helps stabilize microtubules (structural components that transport materials within neurons). In AD, tau can become abnormal and form tangles inside neurons. These tangles can disrupt the transport system in axons, leading to cell dysfunction and death. Tau tangles are closely linked to the severity and progression of cognitive decline.
E is incorrect as research indicates that although beta- amyloid is important the amount of these plaques does not always correlate with the level of cognitive impairment across all patients.
Question 21)
Answer: B) Tau-containing Pick bodies inside neurons.
Explanation: Pick’s disease is a form of frontotemporal dementia (FTD), and it is characterized by tau-containing Pick bodies in neurons, causing progressive dementia, particularly affecting behaviour and language since the frontal lobe controls personality/behaviour and language due to the presence of Broca’s area for speech production. Whilst the temporal lobe is responsible for memory due to the presence of the limbic system and Wernicke’s area for speech comprehension.
A is incorrect as Beta-amyloid plaques are typical of Alzheimer’s disease, not Pick’s disease.
C is incorrect as cognitive decline in Pick’s disease correlates more with tau rather than beta-amyloid, which is not a major feature here.
D is incorrect as Lewy bodies are seen in Parkinson’s disease, not in Pick’s disease.
E is incorrect as brain atrophy, particularly in the frontal and temporal lobes, is a hallmark of Pick’s disease, so a normal MRI is unlikely.
Question 22)
Answer: E) Exner’s area, near the motor cortex for hand movement.
Explanation: Exner’s area is crucial for written language, as it is located near the lateral motor homunculus representing the hands, which are needed for writing.
A is incorrect as Broca’s area affects speech, not writing.
B is incorrect as Wernicke’s area is involved in comprehension, not writing.
C is incorrect as the occipital cortex processes visual information, not motor functions for writing.
D is incorrect as the angular gyrus is more related to reading than writing.

Question 23)
Answer: C) The reticular formation and ascending monoamine pathways
Explanation: The reticular formation in the brainstem and its ascending monoamine projections (involving serotonin, noradrenaline, dopamine, etc.) and upper brainstem are crucial for maintaining consciousness, arousal, and alertness. Damage here can lead to coma.
A is incorrect as the occipital cortex is involved in vision, not arousal.
B is incorrect as the lower brainstem is essential for vital functions like breathing but not directly involved in consciousness.
D is incorrect as the cerebellum controls coordination, not consciousness.
E is incorrect as the basal ganglia are involved in movement control and amplification such as in Parkinson’s and Huntington’s disease, not arousal or consciousness.
Question 24)
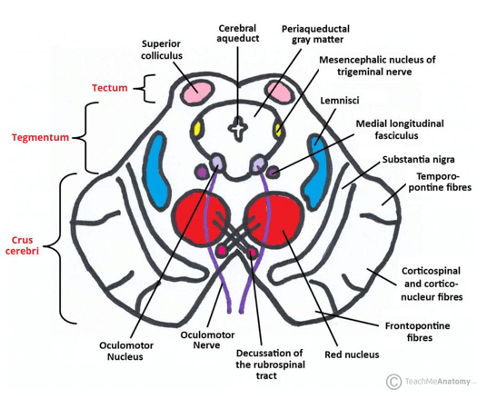
Answer: D) Midbrain
Explanation: The periaqueductal grey matter (PAG) is a region of grey matter located in the midbrain around the cerebral aqueduct, which connects the third and fourth ventricles. The PAG plays a crucial role in pain modulation and coordinating defensive behaviours (like the fight-or-flight response) and is part of pathways involved in emotional and pain responses.
A is incorrect as the pons (located below the midbrain) contributes to autonomic functions and connects the cerebellum to the brainstem but is not the location of the PAG.
B is incorrect as the medulla oblongata is the lower part of the brainstem responsible for vital autonomic functions, such as heart rate, blood pressure, and breathing. It does not contain the periaqueductal grey.
C is incorrect as the limbic system includes structures like the amygdala, hippocampus, and cingulate gyrus, which are involved in emotion, memory, and motivation. Although the PAG is connected to emotional processing (as it interfaces with the limbic system), it is not part of the limbic system itself.
E is incorrect as the basal ganglia are a group of nuclei involved in motor control, habit formation, and reward processing. They include structures such as the caudate, putamen, and globus pallidus but are not involved in pain modulation or defensive behaviours.
Question 25)
Answer: C) Brain herniation
Explanation: In non-communicating hydrocephalus, the ventricles are blocked, causing an uneven distribution of cerebrospinal fluid (CSF) pressure. A lumbar puncture in such cases can result in brain herniation, a life-threatening complication, because lowering CSF pressure in the spine may cause the brain to shift downward toward the foramen magnum.
A is incorrect because an infection of the central nervous system is a general risk with any lumbar puncture, but the specific risk in non-communicating hydrocephalus is brain herniation, therefore, this is not the best answer.
B is incorrect as although bleeding from the puncture site is possible, it’s not the primary concern in hydrocephalus.
D is incorrect as a lumbar puncture in hydrocephalus may decrease, not increase, intracranial pressure.
E is incorrect as permanent spinal cord damage is not a common complication from lumbar puncture, and in non-communicating hydrocephalus, the primary concern is brain herniation.
Question 26)
Answer: A) Disruption of peripheral nerve endings, leading to abnormal brain signal
Explanation: Phantom limb pain is believed to arise because the brain interprets the disruption of peripheral nerve endings as ongoing signals, causing pain to be perceived in the missing limb.
B is incorrect as increased blood flow to the remaining limb does not cause phantom limb pain.
C is incorrect as although inflammation at the amputation site can cause pain, but phantom limb pain is more related to the nervous system and brain misinterpretation
D is incorrect as although bacterial infection in the amputation area could cause local pain, but it is not the cause of phantom limb pain.
E is incorrect as muscle atrophy in the remaining limb is related to nerve signalling, not muscle atrophy.
Question 27)
Answer: E) Horner’s syndrome
Explanation: Horner’s syndrome presents with the classic triad of ptosis (drooping eyelid), miosis (pupil constriction), and anhidrosis (lack of sweating). It results from disruption of the sympathetic nervous system.
A is incorrect as Bell’s palsy causes facial paralysis on one side but does not involve ptosis, miosis, or anhidrosis.
B is incorrect as trigeminal neuralgia presents with severe, shock-like facial pain, but no ptosis, miosis, or anhidrosis.
C is incorrect as although Myasthenia gravis causes ptosis it is due to muscle weakness, not autonomic disruption, and lacks miosis and anhidrosis.
D is incorrect as cluster headache causes severe unilateral headaches, often with autonomic symptoms like tearing or nasal congestion, but it doesn’t present with Horner’s triad.
Question 28)
Answer: A) Complex regional pain syndrome (Type I)
Explanation: Complex regional pain syndrome (Type I), also known as Reflex Sympathetic Dystrophy (RSD), often follows a minor injury and involves burning pain, trophic changes, and vasomotor disturbances like swelling and colour changes.
B is incorrect as Carpal tunnel syndrome causes numbness and tingling in the thumb and first three fingers due to median nerve compression but doesn’t involve skin changes or vasomotor symptoms.
C is incorrect as Phantom limb pain occurs after amputation, not trauma to an intact limb.
D is incorrect Radial nerve injury affects the dorsum of the hand and wrist extensors, causing wrist drop, but not the complex set of symptoms seen in CRPS.
E is incorrect as tendonitis causes localized pain and swelling in tendons, but not the severe burning pain and vasomotor symptoms seen in CRPS.
Question 29)
Answer: C) Alpha-synuclein Lewy bodies in the substantia nigra
Explanation: The patient’s symptoms are consistent with Parkinson’s disease, which is characterized by alpha-synuclein Lewy bodies in the substantia nigra leading to the loss of dopaminergic neurons.
A is incorrect as Beta-amyloid plaques are associated with Alzheimer’s disease, which causes memory loss, not Parkinsonian symptoms.
B is incorrect as Tau protein tangles are also associated with Alzheimer’s disease and frontotemporal dementia/(Picks), causing cognitive decline rather than movement disorders.
D is incorrect as loss of Purkinje cells occurs in cerebellar disorders, which result in ataxia, not the bradykinesia and tremors seen in Parkinson’s disease.
E is incorrect as demyelination of motor neurons is characteristic of multiple sclerosis or ALS, which leads to weakness, not the rigidity and tremor seen in Parkinson’s.
Question 30)
Answer: B) Charcot-Bouchard aneurysm
Explanation: Charcot-Bouchard aneurysms are small aneurysms found in the deep penetrating arteries, such as the lenticulostriate arteries, which supply the basal ganglia, thalamus, and internal capsule. They are strongly associated with chronic hypertension, which causes these small vessels to weaken and rupture, leading to deep intracerebral haemorrhages.
A is incorrect as Arteriovenous malformations (AVMs) are congenital vascular malformations involving abnormal connections between arteries and veins, typically found in larger vessels. AVMs often cause subarachnoid haemorrhage, especially in younger patients, rather than deep intracerebral bleeds.
C is incorrect as Cerebral amyloid angiopathy (CAA) is associated with the deposition of amyloid in the blood vessels of the cerebral cortex and the peripheries of the brain, leading to lobar haemorrhages. It primarily affects elderly individuals but not the deep structures of the brain.
D is incorrect as Venous sinus thrombosis refers to a blood clot in the venous sinuses of the brain, which can cause venous congestion and haemorrhage, but it is not directly related to hypertension or deep brain structure haemorrhages.
E is incorrect as Subarachnoid haemorrhages usually occur due to berry aneurysm rupture in the circle of Willis or from AVMs, and typically result in bleeding into the space between the brain and its protective membranes (pia and arachnoid mater), rather than the deep brain structures.
Question 31:
Answer: C) Procedural
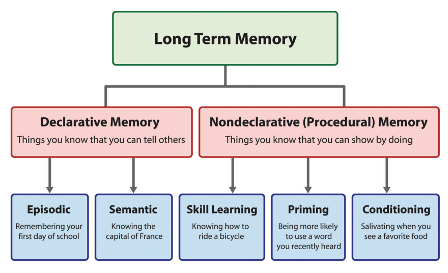
Explanation: Declarative Memory refers to memories that can be consciously recalled, such as facts and events. It is divided into:
- Semantic memory: Knowledge about facts, concepts, and general information (e.g., “Paris is the capital of France”).
- Episodic memory: Memory of personal experiences and specific events (e.g., “I went to Paris last summer”).
- Working memory: Short-term memory used to temporarily store and manipulate information for cognitive tasks (e.g., remembering a phone number while dialling it).
- Short-term memory: The ability to hold a small amount of information in an active, readily accessible state for a short period (e.g., remembering a sequence of numbers). Short term memory is essentially working memory.
Procedural Memory is not a part of declarative memory. It refers to non-declarative memory, which includes motor skills, habits, and tasks that can be performed without conscious awareness (e.g., riding a bike or playing an instrument).
Question 32:
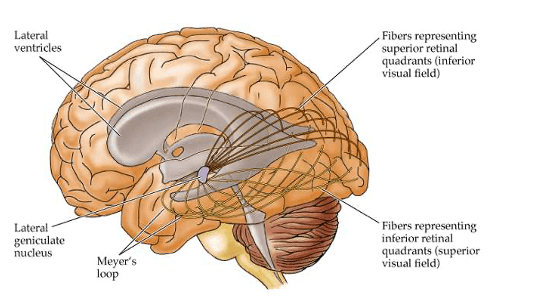
Answer: A) Carries information from the superior retinal field, corresponding to the inferior visual field in the visual cortex, and passes through the parietal lobe.
Explanation: There are two groups of optic radiation fibres that pass through each cerebral hemisphere: Baum’s loop and Meyer’s loop. Baum’s loop passes through the parietal lobe, whereas Meyer’s loop passes through the temporal lobe. Baum’s loop carries information from the superior retina, and due to the inversion of images in the occipital lobe, this corresponds to the inferior visual field. In contrast, Meyer’s loop carries information from the inferior retina, which is also flipped in the occipital lobe, corresponding to the superior visual field.
Option B is incorrect because it states that Baum’s loop carries information from the superior retinal field, which is correct, but it incorrectly claims that this information passes through the temporal lobe instead of the parietal lobe.
Option D is incorrect because it refers to Meyer’s loop, which processes information from the inferior retinal field that corresponds to the superior visual field. Meyer’s loop passes through the temporal lobe, not Baum’s loop.
Question 33
Answer: D) Congestion/hyperaemia.
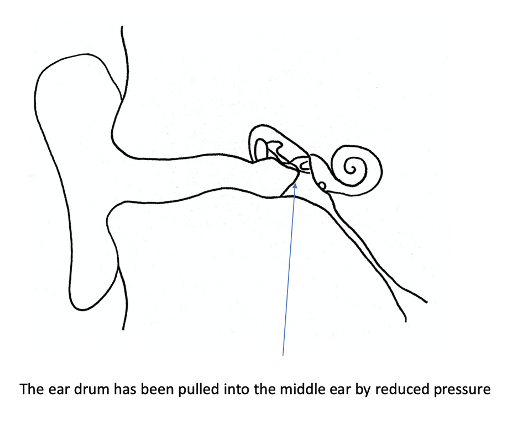
Explanation: Following the obstruction of the pharyngotympanic/Eustachian tube (stage 1), this causes increased pressure in the middle ear since mastoid air cells can allow air into the middle ear however no air can be released (due to closure of pharyngotympanic tube). Due to increased pressure, this causes mucous cells in the inner ear to release a serous fluid. The release of this fluid increases blood flow to the middle ear (hyperaemia) causing the tympanic membrane to appear red & swollen.
Option A is incorrect because perforation of the tympanic membrane is generally considered the last stage (stage 4), occurring after significant accumulation of pus (suppuration) in the middle ear.
Option B is incorrect because obstruction of the pharyngotympanic tube usually occurs first, leading to fluid build-up which triggers the second stage.
Option C is incorrect because suppuration occurs after congestion/hyperaemia, as it is characterised by the accumulation of pus due to the ongoing infection. The ‘battle’ between white blood cells & the virus (e.g. rhinovirus/adenovirus) or bacteria (staphylococcus aureus/streptococcus pneumonia/haemophilus influenzae) causing the infection leads to the release of pus. This pus accumulation exacerbates conductive hearing loss and fever.
Option E is incorrect because the appearance of bubbles on the tympanic membrane indicates fluid presence and typically occurs early in the infection process. It is often associated with non-suppurative otitis media and can be triggered by adenoids obstructing the pharyngotympanic tube.

Question 34
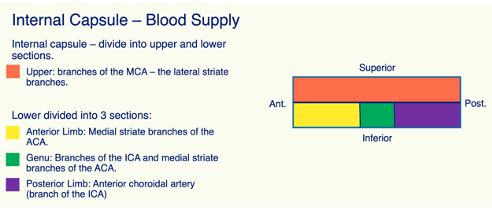
Answer: B) Middle striate branches of the anterior cerebral artery & branches of the internal carotid artery.
Explanation: The genu of the internal capsule, located between the anterior and posterior limbs, receives blood supply from the middle striate branches of the anterior cerebral artery and branches from the internal carotid artery.
Option A is incorrect because the lateral striate branches of the middle cerebral artery primarily supply the upper portion of the internal capsule.
Option C is incorrect as it incorrectly states the source of the striate branches. The medial striate arteries are branches of the anterior cerebral artery not middle cerebral artery. The genu is not primarily supplied by branches from the middle cerebral artery.
Option D is incorrect because while the anterior cerebral artery contributes to the supply of the genu, it does not do so exclusively. It is the combination with the internal carotid artery branches that is crucial.
Option E is incorrect because the anterior choroidal artery primarily supplies the posterior internal capsule, choroid plexus of the lateral ventricles and parts of the thalamus and hippocampus, not the genu of the internal capsule.
Question 35
Answer: D) Gait abnormalities.
Explanation: Gait abnormalities are generally not considered a classic symptom of an acute rise in intracranial pressure (ICP). They are symptoms of chronic rise in intracranial pressure e.g. due to gradual increase of CSF or a slow growing tumour which may be found in the precentral gyrus. Typical symptoms of chronic rise of intracranial pressure also include urinary incontinence and cognitive/memory problems e.g. dementia.
Option A is incorrect because papillodeama is a well-known sign of increased ICP, characterised by swelling of the optic disc due to elevated pressure. The optic nerve is surrounded by meninges (which contain CSF). The increase in pressure of the CSF compresses the blood vessels. Since veins have much thinner walls than arteries, they are significantly more compressed than arteries. This allows blood to supply the optic nerve but not to leave which causes swelling of the optic disc.
Option B is incorrect as Cushing’s triad (hypertension, bradycardia, and irregular respirations) is a classic response to increased ICP, indicating potential brain herniation due to a rapid rise of intracranial pressure.
Option C is incorrect because headaches that worsen with coughing or sneezing (the Valsalva manoeuvre) are typical symptoms of increased ICP due to the sudden rise in pressure in the cranial cavity.
Option E is incorrect as pulsatile tinnitus can occur with increased ICP due to changes in the vascular dynamics and pressure around the auditory structures.
Question 36
Answer: A) Syringomyelia
Explanation: Syringomyelia is characterised by the formation of a fluid-filled cavity (syrinx) within the spinal cord, typically affecting the cervical region. This condition leads to a bilateral loss of pain and temperature sensations due to damage to the crossing fibres of the spinothalamic tract, resulting in a “cape-like” distribution of sensory loss over the upper back and shoulders. The corticospinal tract is typically the first to be affected, leading to limb weakness, and as the syrinx expands, it can damage the spinothalamic tract.
Option B is incorrect because sensory polyneuropathy involves diffuse peripheral nerve damage, which typically results in symmetrical loss of sensation in a “stocking-glove” distribution rather than the “cape-like” pattern seen in syringomyelia.
Option C is incorrect because sensory neuronopathy involves the degeneration of sensory neurons specifically in the DRG, leading to a different pattern of sensory loss such as sensory ataxia, including loss of proprioception & fine touch which are spared in syringomyelia.
Option D is incorrect as radiculopathy is due to nerve root compression or damage of the ventral root/lower motor neuron, which causes symptoms in a dermatomal pattern depending on the affected nerve root, rather than the bilateral loss of pain and temperature sensation seen in syringomyelia.
Option E is incorrect because Brown-Sequard syndrome results from a hemisection of the spinal cord, causing ipsilateral loss of proprioception and vibration sense and contralateral loss of pain and temperature sensation, which does not create the “cape-like” distribution characteristic of syringomyelia.
Question 37
Answer: C) Arcuate fasciculus
Explanation: The arcuate fasciculus is a bundle of axons that connects Broca’s area (in the frontal lobe) to Wernicke’s area (in the temporal lobe), facilitating communication between these two critical regions involved in language processing. Damage to the arcuate fasciculus can result in conduction aphasia, where a person may have difficulty repeating spoken language despite having intact comprehension and fluent speech.
Option A is incorrect because the medial longitudinal fasciculus is primarily involved in coordinating eye movements connecting the oculomotor nucleus to the abducens nucleus. Damage to the medial longitudinal fasciculus results in intranuclear ophthalmoplegia whereby the ipsilateral eye fails to adduct & the contralateral exhibits nastygmas.
Option B is incorrect as the medial lemniscus is a pathway that carries sensory information regarding touch and proprioception via the dorsal column medial lemniscus pathway towards the somatosensory cortex, not language processing, and does not connect these two areas.
Option D is incorrect because Meyer’s fibres are part of the optic radiation, relaying information from the retina towards the occipital lobe (primary visual area specifically), although it passes through the temporal lobe similar to the arcuate fasciculus fibres.
Option E is incorrect because there are indeed physical fibres, specifically the arcuate fasciculus, that connect Broca’s area and Wernicke’s area, allowing for integrated language function.

Question 38
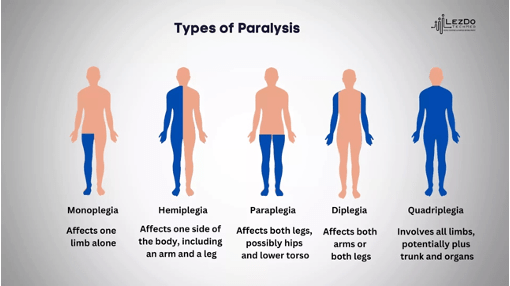
Answer: C) Paraplegia below the level of T2
Explanation: Paraplegia is characterised by paralysis or severe weakness of the lower limbs and occurs when there is damage to the spinal cord at or below the T2 level. This results in loss of motor function in the legs while typically sparing arm function, as the injury does not affect the cervical segments of the spinal cord that innervate the upper limbs.
Option A is incorrect because quadriplegia (or tetraplegia) refers to paralysis affecting all four limbs and typically occurs with injuries at or above the level of C6.
Option B is incorrect because hemiplegia refers to paralysis of one side of the body, and it typically results from a brain lesion rather than a specific level of spinal cord injury.
Option D is incorrect because monoplegia refers to paralysis affecting a single limb.
Option E is incorrect because hemiplegia below the level of C6 is not applicable; hemiplegia involves unilateral paralysis often resulting from brain injury or stroke, not from spinal cord damage below C6.
Question 39
Answer: A) Internal capsule
Explanation: Hemiplegia is primarily caused by damage to the internal capsule, which contains important motor pathways that convey signals from the primary motor cortex to the brainstem and spinal cord. Damage to this area leads to contralateral paralysis and weakness of the body on the opposite side.
Option B is incorrect because damage at the synapse between upper motor neurons (UMN) and lower motor neurons (LMN) does not typically cause hemiplegia; it can lead to different types of motor deficits such as motor neuron disease, but not the classic presentation of hemiplegia.
Option C is incorrect because while damage to the pyramids of the medulla oblongata can affect motor function, it is less common for causing hemiplegia directly compared to lesions in the internal capsule.
Option D is incorrect because, although damage to the primary motor cortex can result in hemiplegia, it is more often the case that the internal capsule, which carries fibres from the motor cortex, is affected in clinical presentations of hemiplegia.
Option E is incorrect because while damage to the corona radiata can affect motor function, the internal capsule is more directly implicated in causing hemiplegia due to its role in transmitting motor signals from the cortex to the rest of the nervous system.
Question 40
Answer: C) Rubella
Explanation: Rubella is not commonly associated with labyrinthitis. While measles, mumps, and meningitis can lead to inflammation of the inner ear structures, labyrinthitis is more directly linked to viral infections like measles and mumps, as well as bacterial infections from complications of otitis media. Rubella, primarily a respiratory virus, does not typically lead to labyrinthitis.
Option A is incorrect because measles can cause viral labyrinthitis due to its effects on the inner ear.
Option B is incorrect as mumps is well-known for causing viral labyrinthitis, especially in children.
Option D is incorrect because meningitis, particularly viral or bacterial meningitis, can lead to labyrinthitis as a secondary complication due to inflammation.
Option E is incorrect because complications from otitis media, such as the spread of infection, can directly result in labyrinthitis, affecting the inner ear structures.

Question 41
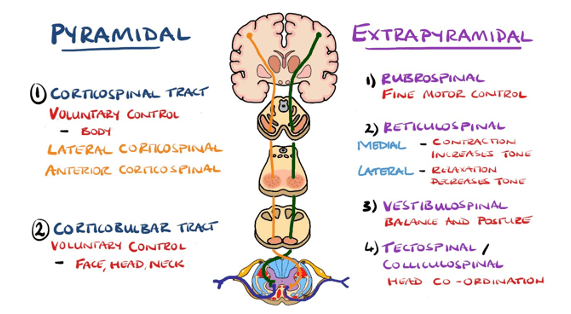
Answer: E) Corticobulbar tract
Explanation: The corticobulbar tract is a voluntary motor pathway that controls the movements of the head and neck, particularly those involving the facial muscles and muscles of mastication. It originates in the motor cortex and terminates in the cranial nerve nuclei in the brainstem, directly influencing voluntary movement in the head and neck region.
Option A is incorrect because the rubrospinal tract primarily facilitates flexor muscle activity and influences motor control of the upper limbs, but it does not specifically target head and neck movements.
Option B is incorrect as the corticospinal tract is mainly responsible for voluntary movements of the limbs and trunk, particularly skilled movements.
Option C is incorrect because the tectospinal tract is involved in reflexive head movements in response to visual and auditory stimuli & is considered an involuntary tract.
Option D is incorrect because the reticulospinal tract plays a role in the regulation of posture and locomotion & is considered an involuntary tract.
Question 42
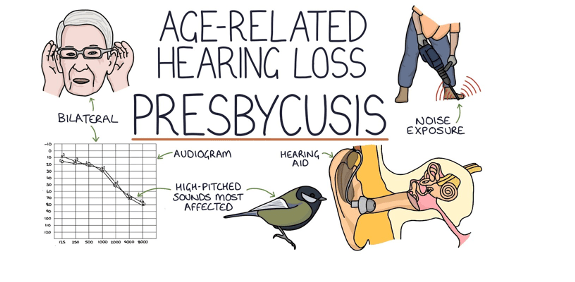
Answer: A) Presbyacusis
Explanation: Presbyacusis is the age-related degeneration of the cochlear end organs, primarily affecting the hair cells in the cochlea. This condition typically results in a gradual loss of hearing, particularly for high-frequency sounds, and is a common consequence of aging.
Option B is incorrect because labyrinthitis refers to inflammation of the inner ear structures, including both the cochlea and the vestibular system, rather than specific degeneration of the cochlear end organs.
Option C is incorrect as vestibular schwannoma (also known as acoustic neuroma) is a benign tumour that affects the vestibulocochlear nerve (CN VIII), leading to hearing loss and balance issues, but it does not primarily involve degeneration of the cochlear end organs themselves.
Option D is incorrect because aplasia refers to the absence or incomplete development of an organ or tissue, rather than degeneration of existing structures. In the case of cochlear aplasia, the cochlea may not develop properly, but it is not a degenerative condition rather a congenital problem.
Option E is incorrect as atresia refers to the absence or closure of a normal opening, such as in the case of congenital aural atresia, where the ear canal does not form properly. This condition does not involve degeneration of the cochlear end organs rather the absence of the external auditory canal & auricle.
Question 43
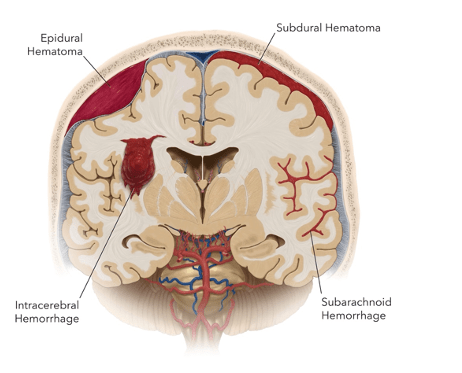
Answer: C) Subarachnoid haemorrhage
Explanation: Subarachnoid haemorrhage is characterised by a sudden, severe headache often described as a “thunderclap headache” or “the worst headache of my life.” This type of headache typically occurs when there is arterial bleeding into the subarachnoid space, often due to a ruptured berry aneurysm, amyloid plaque formation or arteriovenous malformation.
Option A is incorrect because epidural haemorrhage usually presents with a “lucid interval” followed by a progressive decline in consciousness. The headache associated with epidural haemorrhage is typically not as severe or sudden as that of a subarachnoid haemorrhage.
Option B is incorrect since subdural haemorrhage often results in more gradual symptoms, including headache and confusion, rather than the immediate and intense headache, a characteristic of subarachnoid haemorrhage.
Option D is incorrect because intracerebral haemorrhage can also cause headaches, but the headache is usually not as sudden or severe as in subarachnoid haemorrhage. Symptoms typically relate more to the area of the brain affected and can include focal neurological deficits.
Option E is incorrect as Charcot-Bouchard haemorrhage refers to small vessel disease associated with chronic hypertension, leading to small intracerebral bleeds. This condition does not typically present with a thunderclap headache.
Question 44
Answer: A) Herpes simplex virus type 1
Explanation: Herpes simplex virus is one of the main viruses that causes encephalitis not meningitis. Furthermore, meningitis is more associated with bacterial infections unlike encephalitis which is associated with viruses.
Option A is incorrect because Herpes simplex virus type 1 is a known cause of viral meningitis, particularly in adults.
Option B is incorrect as Herpes simplex virus type 2 is one of the leading causes of viral meningitis, particularly in sexually active individuals.
Option C is incorrect because HIV can cause viral meningitis & encephalitis, especially during the acute phase of infection.
Option D is incorrect since enteroviruses are a common viral cause of meningitis, especially in children.
Option E is incorrect since Toxoplasma is not a virus; it is a protozoan parasite that can cause various infections, including encephalitis in immunocompromised individuals, but it does not cause viral meningitis.

Question 45
Answer: C) Macular degeneration.
Explanation: Macular degeneration is a chronic condition that leads to gradual vision loss, primarily affecting central vision. There are two types of age-related macular degeneration: dry and wet. Dry macular degeneration is characterised by the normal wear and tear of the macula of the retina, leading to gradual vision loss. In contrast, wet macular degeneration involves the abnormal growth of blood vessels in the retina; if these vessels bleed, they can cause severe vision loss if not treated promptly.
Option A is incorrect because vitreous haemorrhage can lead to sudden vision loss and requires urgent medical evaluation. Vitreous haemorrhage involves the leaking of blood vessels into the vitreous fluid of the eye. This leads to scattered light rays entering the eye making it very difficult for light to be focused onto the retina.
Option B is incorrect as retinal vein occlusion can cause sudden vision loss and is considered a medical emergency that may lead to permanent damage if not addressed quickly.
Option D is incorrect because retinal detachment is a medical emergency characterised by sudden vision loss and requires immediate intervention to prevent permanent vision loss. This occurs due to the accumulation of vitreous fluid between the choroid & the retina causing the retina to detach.
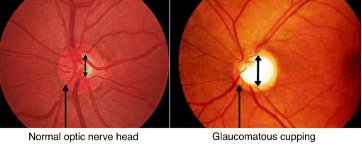
Option E is incorrect since closed-angle glaucoma can cause a rapid increase in intraocular pressure due to sudden blockage of the drainage of aqueous humor, leading to rapid vision loss and severe eye pain, constituting a medical emergency.
Question 46
Answer: B) Middle cerebral artery.
Explanation: The middle cerebral artery (MCA) is the main vessel affected by subarachnoid haemorrhages (SAH), particularly in cases of rupture of a berry aneurysm. When an aneurysm associated with the MCA ruptures, it leads to bleeding into the subarachnoid space, resulting in increased intracranial pressure and potentially severe neurological deficits.
Option A is incorrect because the middle meningeal artery is primarily associated with epidural haemorrhage rather than subarachnoid haemorrhage. Injury to this artery, often due to skull fractures (pterion), can lead to bleeding between the dura mater and the skull.
Option C is incorrect as the middle cerebellar artery is not typically associated with subarachnoid haemorrhage. It supplies the cerebellum, and bleeding here would not usually fall under SAH.
Option D is incorrect since the maxillary artery is a branch of the external carotid artery and is not involved in subarachnoid haemorrhage.
Option E is incorrect because while the anterior cerebral artery (ACA) can also be affected by aneurysms, it is not the main vessel typically associated with SAH; the middle cerebral artery is more commonly implicated in these events.

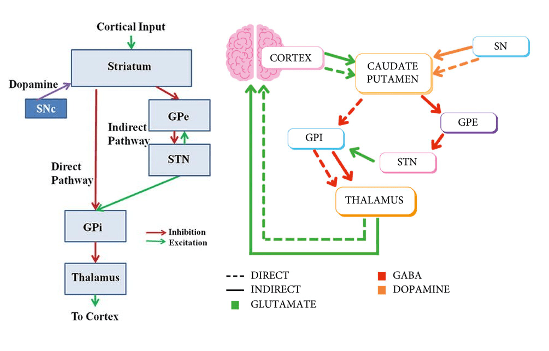
Question 47
Answer: B) Glutamate
Explanation: The subthalamic nucleus (STN) primarily releases glutamate, which is an excitatory neurotransmitter. It plays a crucial role in the regulation of motor control by providing excitatory input to the globus pallidus internus and substantia nigra pars reticulata, both of which are involved in the inhibition of thalamic activity and motor function. When globus pallidus internus is excited, it releases GABA which inhibits the thalamus, which in turn inhibits the cerebral cortex preventing movement.
Option A is incorrect because GABA (gamma-aminobutyric acid) is the primary inhibitory neurotransmitter in the brain, but the subthalamic nucleus is not a GABAergic structure; it predominantly releases glutamate. The striatum (caudate nucleus & putamen), globus pallidus externus & internus all release GABA.
Option C is incorrect as dopamine is primarily released by the substantia nigra, and while it plays a significant role in the basal ganglia circuitry, it is not released by the subthalamic nucleus.
Option D is incorrect because acetylcholine is released by cholinergic neurons in the striatum, not the subthalamic nucleus.
Option E is incorrect because substance P is a neuropeptide associated with pain perception and is primarily found in the striatum, but it is not the main neurotransmitter released by the subthalamic nucleus.
Question 48
Answer: C) Tentorium cerebelli
Explanation: The tentorium cerebelli is a dural fold that separates the cerebellum from the cerebrum.
Option A is incorrect because the falx cerebri separates the two cerebral hemispheres.
Option B is incorrect because the falx cerebelli separates the two hemispheres of the cerebellum.
Option D is incorrect because the calcarine sulcus is part of the occipital lobe, not a dural fold.
Option E is incorrect because the diaphragm sellae covers the pituitary gland.

Question 49
Answer: D) Fine touch
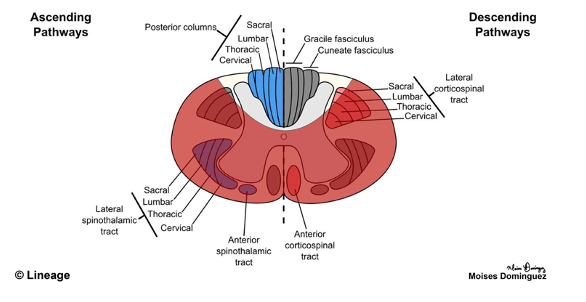
Explanation: The anterior spinal artery supplies the anterior 2/3 of the spinal cord meaning that the both the spinothalamic tract & corticospinal tract will be affected. The Dorsal Column Medial Lemniscus tract is supplied by the posterior spinal artery, thus is spared. Fine touch is unaffected by spinal artery syndrome because it is carried by the dorsal columns, which are supplied by the posterior spinal arteries and are typically spared in spinal artery syndrome.
Option A is incorrect because pain sensation is affected, as it is carried by the spinothalamic tract, which is supplied by the anterior spinal artery.
Option B is incorrect because temperature sensation is also carried by the spinothalamic tract.
Option C is incorrect because crude touch, like pain and temperature, is transmitted by the spinothalamic tract, which can be compromised in spinal artery syndrome.
Option E is incorrect because motor function is affected due to the involvement of the corticospinal tract, which is also supplied by the anterior spinal artery.
Question 50
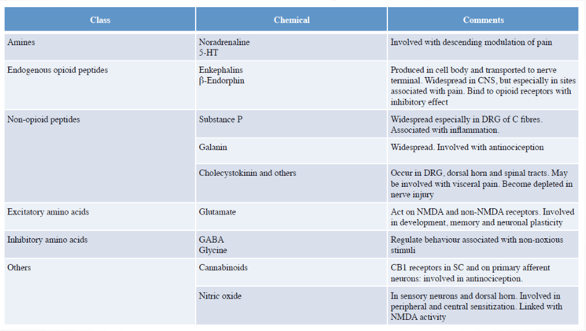
Answer: B) Substance P
Explanation: Substance P is a neuropeptide released by C fibres in the dorsal root ganglia and is involved in the transmission of pain signals. It is thought to enhance the perception of pain by increasing sensitivity to painful stimuli in the central nervous system.
Option A is incorrect because while glutamate is also involved in pain transmission, it mainly acts as an excitatory neurotransmitter in synapses between nociceptors and neurons in the dorsal horn, not specifically within the dorsal root ganglia of C fibres. It also plays a key role in the memory of pain.
Option C is incorrect because cholecystokinin is more involved in pain coming from viscera since it is mainly involved in digestion and satiety.
Option D is incorrect because galanin is associated with modulating pain & has inhibitory effects on pain pathways.
Option E is incorrect because nitric oxide it is primarily involved in peripheral & central sensitisation predominantly in sensory neurons.
Question 51
Answer: A) Microvascular disease
Explanation: The most common cause of complete CN III palsy, particularly affecting the central fibres of the oculomotor nerve, is microvascular disease, such as diabetes or hypertension. These conditions can lead to ischemia in the small blood vessels supplying the nerve. The central fibres, which control eye movements and the eyelid, are most susceptible to ischemia.
Option B is incorrect because compression by tumours or aneurysms typically affects the peripheral fibres of the oculomotor nerve, leading to loss of vasoconstriction of the pupil before complete palsy.
Option C is incorrect because meningitis can affect multiple cranial nerves such as the abducens nerve (CN VI), but it is less likely to cause isolated CN III palsy.
Option D is incorrect because neurodegenerative diseases do not typically cause isolated cranial nerve palsies.
Option E is incorrect because haemorrhage, while serious, is a less common cause of CN III palsy compared to microvascular disease.
Question 52
Answer: B) Periaqueductal grey matter.
Explanation: The periaqueductal grey matter (PAG) is the primary control centre for descending pain modulation. Located around the cerebral aqueduct in the midbrain, it plays a crucial role in inhibiting pain signals through connections with the medulla and spinal cord. The PAG activates endogenous opioid pathways, which suppress pain transmission.
Option A is incorrect because the medial lemniscus is involved in carrying sensory information, particularly fine touch, proprioception, and vibration, but it does not play a role in pain modulation.
Option C is incorrect as the superior colliculus is primarily involved in visual processing and the coordination of eye movements, not in pain control.
Option D is incorrect because the cerebral peduncles contain motor pathways that connect the brain to the spinal cord, but they are not involved in pain modulation.
Option E is incorrect as the medial longitudinal fasciculus coordinates eye movements by connecting the oculomotor, trochlear, and abducens nuclei.
Question 53
Answer: C) Medial rectus.
Explanation: The medial rectus muscle is essential for the convergence phase of the accommodation reflex, which is adduction (the inward movement of both eyes) to focus on a near object. This muscle pulls the eyes medially, allowing them to converge/focus when looking at something close, such as during reading or focusing on nearby objects. Refractive convergent strabismus is caused by excessive use of the accommodation reflex which is why children often present with adducted eyes.
Option A is incorrect because the ciliary muscle is involved in changing the shape of the lens for focusing (accommodation), but not in the actual convergence of the eyes.
Option B is incorrect because the levator palpebrae superioris is responsible for elevating the eyelid, is not characterised as an intraocular eye muscle and plays no role in the convergence of the eyes.
Option D is incorrect because the lateral rectus muscle abducts the eye, moving it away from the midline, which is the opposite of the action required for convergence.
Option E is incorrect because the superior rectus elevates the eye but is not responsible for the convergence of the eyes.

Question 54
Answer: A) Retinal detachment
Explanation: Retinal detachment typically starts in peripheral areas, but if the macula detaches, central vision will be affected. It is caused by vitreous fluid building up between the choroid & the retina causing the retina to detach.
Option B is incorrect because diabetic retinopathy is characterised by abnormal growth of blood vessels which may leak into the retina causing gradual vision loss, particularly affecting central vision.
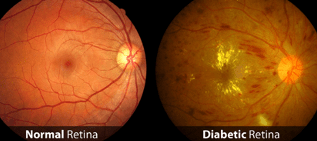
Option C is incorrect because retinal vein occlusion is characterised by blockage or obstruction of a vein that supplies the retina, leading to retinal swelling and bleeding, often described as a “blood and thunder” appearance.

Option D is incorrect because retinal artery occlusion is caused by blockage of the arteries supplying the retina, resulting in ischaemia. It typically affects central vision and is characterised by a pale retina and a “cherry red spot” at the fovea.
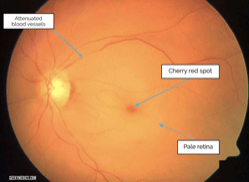
Option E is incorrect because glaucoma results from obstruction of the drainage of aqueous humor, leading to increased intraocular pressure that can damage the optic nerve and cause vision loss, often affecting peripheral vision initially.
Question 55)
Correct Answer:
B) Friedreich’s Ataxia
- Explanation: Friedreich’s ataxia is an autosomal recessive disorder caused by mutations in the FXN gene. It presents with progressive ataxia (loss of coordination and balance), dysarthria (inability to produce speech) ,spastic paraperesis ( lower limb weakness) , cardiomyopathy, and diabetes mellitus, all of which match the patient’s presentation.
Incorrect Answers:
A) Duchenne Muscular Dystrophy
- Explanation: Duchenne Muscular Dystrophy is an X-linked recessive disorder that causes progressive muscle weakness, primarily affecting proximal muscles. It is not associated with ataxia, dysarthria, cardiomyopathy, or diabetes in childhood. The FXN gene is not involved.
C) Parkinson’s Disease
- Explanation: Parkinson’s disease is a neurodegenerative disorder typically seen in older adults, characterized by bradykinesia, resting tremor, and rigidity. It does not present with ataxia or affect children, and there is no link to the FXN gene.
D) Huntington’s Disease
- Explanation: Huntington’s disease is an autosomal dominant disorder that presents in adulthood with chorea, cognitive decline, and psychiatric symptoms. It is caused by a mutation in the HTT gene, not the FXN gene, and does not cause ataxia, cardiomyopathy, or diabetes in childhood.
E) CMT-X1 (Charcot-Marie-Tooth Disease X-linked)
- Explanation: CMT-X1 is an X-linked recessive neuropathy presenting with peripheral nerve dysfunction, distal muscle weakness, and sensory loss. It does not cause ataxia, cardiomyopathy, or diabetes, and is associated with GJB1 gene mutations, not FXN.
Question 56)
Correct answer: B) It arises from astrocytes and is highly aggressive, often crossing the corpus callosum Glioblastoma multiforme is a highly aggressive primary brain tumour that arises from astrocytes. It is known for crossing the corpus callosum, leading to a “butterfly” appearance on imaging. It often leads to severe complications like increased intracranial pressure, brain herniation, and neurological deficits.
- A) It arises from oligodendrocytes and is typically slow-growing with minimal metastasis outside the brain
Incorrect: While oligodendrogliomas do arise from oligodendrocytes, they are typically less aggressive and slow-growing compared to glioblastoma. They rarely metastasise outside the brain, but this option does not fit glioblastoma’s characteristics. - C) It primarily originates from peripheral nervous system Schwann cells and is commonly associated with neurofibromatosis type 2
Incorrect: This describes a vestibular schwannoma (acoustic neuroma), which arises from Schwann cells in the peripheral nervous system and is associated with NF2. This tumour is usually slow-growing and not as aggressive as glioblastoma. - D) It is a secondary tumour, commonly metastasising from a lung carcinoma
Incorrect: While secondary brain tumours (brain metastases) can commonly come from primary lung cancers, the vignette describes a primary brain tumour. Glioblastomas are primary tumours that do not metastasise outside the brain. - E) It arises from meningeal cells and is commonly benign, compressing adjacent brain structures
Incorrect: This describes a meningioma, which arises from the meninges. Meningiomas are usually benign and cause symptoms by compressing adjacent brain tissue. Glioblastomas, by contrast, are malignant and infiltrative, rather than merely compressive.
Question 57)
Correct Answer:
B) LEMS is often associated with small cell lung carcinoma (SCLC).
- B) LEMS is often associated with small cell lung carcinoma (SCLC).
- Explanation: This is correct. LEMS is a well-known paraneoplastic syndrome that frequently occurs in patients with SCLC, making it important for clinicians to evaluate underlying malignancies when LEMS is diagnosed. Typical symptoms include amnesia, ataxia and myasthenia. Use of muscles help make it better. It also leads to autonomic dysregulation hence symptoms of dry mouth, incontinence and constipation.
Explanation of Options:
- A) LEMS is primarily caused by direct damage to the neuromuscular junction.
- Explanation: This is incorrect. LEMS is caused by antibodies that block presynaptic voltage-gated calcium channels, leading to a decrease in acetylcholine release, rather than direct damage to the neuromuscular junction.
- C) Symptoms of LEMS include only muscle weakness without any autonomic dysfunction.
- Explanation: This is incorrect. While muscle weakness is a hallmark symptom of LEMS, many patients also experience autonomic symptoms, such as dry mouth, constipation, and orthostatic hypotension.
- D) LEMS can be treated effectively with antibiotics.
- Explanation: This is incorrect. LEMS is not caused by a bacterial infection; therefore, antibiotics are not effective. Treatment typically includes therapies like 3,4-diaminopyridine (3,4-DAP) or immunotherapy.
- E) LEMS is an autoimmune disorder that primarily affects the peripheral nervous system.
- Explanation: While LEMS is considered an autoimmune condition, its primary effect is at the neuromuscular junction and it is specifically linked to the presynaptic nerve terminal rather than the peripheral nervous system as a whole.
Question 58)
Correct Answer:
B) Hyperopia (farsightedness) typically leads to difficulty seeing objects up close.
- B) Hyperopia (farsightedness) typically leads to difficulty seeing objects up close.
- Explanation: This statement is correct. Hyperopia occurs when the eyeball is too short or the cornea is too flat, causing light to focus behind the retina. As a result, individuals have trouble seeing close objects clearly. This is treated by using a convex lens

Explanation of Options:
- A) Myopia (nearsightedness) is caused by an excessively short eyeball.
- Explanation: This statement is incorrect. Myopia is usually caused by an excessively long eyeball or an overly curved cornea, which causes light to focus in front of the retina, making distant objects appear blurry. This is treated by a concave lens
- C) Astigmatism is primarily caused by a perfectly spherical cornea.
- Explanation: This statement is incorrect. Astigmatism is caused by an irregularly shaped cornea or lens, which leads to blurred vision at all distances due to irregular refractive of light on the retina. A perfectly spherical cornea would not cause astigmatism. Astigmatism is treated via a toric lens (custom to the patient)
- D) Presbyopia is a refractive error that can be corrected with laser surgery.
- Explanation: This statement is misleading. Presbyopia, the age-related loss of the eye’s ability to focus on close objects, is generally treated with reading glasses or multifocal lenses. While some laser procedures exist, they do not universally correct presbyopia as they do for other refractive errors. This is a version of hyperopia for older aged patients.
- E) All refractive errors can be effectively corrected using the same type of lenses.
- Explanation: This statement is incorrect. Different refractive errors require specific types of corrective lenses (e.g., concave lenses for myopia, convex lenses for hyperopia, and cylindrical lenses for astigmatism). Therefore, not all errors can be corrected using the same lenses.
Question 59)
Correct Answer: C) Amyotrophic Lateral Sclerosis (ALS)
C) Amyotrophic Lateral Sclerosis (ALS)
- Explanation: Correct. ALS is a form of Motor Neuron Disease (MND) characterized by the degeneration of both upper and lower motor neurons. It often presents with mixed symptoms such as muscle weakness, atrophy, fasciculations, hyperreflexia, and spasticity. The involvement of both upper and lower motor neurons, along with muscle atrophy and swallowing difficulties, makes ALS the most likely diagnosis. It occurs due to the build up of TDP43 proteins in motor neurons causing motor neuron degeneration. Even in late stages of this disease facial extraocular muscles and sphincters are spared and there are NO SENSORY IMPAIRMENTS.
Explanation of incorrect Answer Options:
A) Spinal Muscular Atrophy (SMA)
- Explanation: Incorrect. While SMA is a rare motor neuron disease, it is characterised by LMN symptoms only in the same level myotome.Only LMNs degenerate (resulting in fasciculations, weakness,atrophy and hyporeflexia)- due to mutation in SMN1 gene – survivor protein in motor neuron health. However in this case the patient suffers from UMN symptoms as well such as hyperreflexia.
B) Primary Lateral Sclerosis (PLS)
- Explanation: Incorrect. PLS is a rare form of MND that primarily affects upper motor neurons only, leading to progressive spasticity, weakness, and hyperreflexia. PLS does not cause muscle atrophy or fasciculations, as these are features of lower motor neuron involvement, which distinguishes it from ALS.
D) Multiple Sclerosis (MS)
- Explanation: Incorrect. MS is a demyelinating disorder affecting the central nervous system and presents with a wide range of symptoms, often including sensory disturbances, visual impairment, and muscle weakness. However, MS does not typically cause muscle atrophy or fasciculations, which are specific to motor neuron involvement, and is less likely to present with concurrent upper and lower motor neuron signs. Furthermore MS typically causes issues with the bladder control and sensory modalities which the patient does not suffer from.
E) Myasthenia Gravis (MG)
- Explanation: Incorrect. MG is an autoimmune neuromuscular disorder that leads to muscle weakness and fatigability, particularly in ocular, facial, and bulbar muscles. It does not cause muscle atrophy or fasciculations, nor does it involve both upper and lower motor neuron signs. MG typically improves with rest and often has a fluctuating course, unlike the progressive pattern seen in ALS.
Question 60)
Correct Answer: B) Right Temporal Lobe
Explanation: Correct. The temporal lobe contains Meyer’s Loop, where fibers from the inferior retinal quadrants (which correspond to the superior visual field quadrants) pass through. A lesion in the right temporal lobe affects the contralateral (left) visual field, specifically producing a left superior quadrantanopia. This is consistent with the findings in this patient.
Explanation of Answer Options:
A) Right Parietal Lobe
- Explanation: Incorrect. Lesions in the right parietal lobe typically affect Baum’s loop which contains the superior retinal quadrants (correspond to the inferior visual field). Lesions in the parietal lobe more commonly affect the contralateral inferior visual field, leading to a left inferior quadrantanopia.
C) Left Occipital Lobe
- Explanation: Incorrect. A lesion in the left occipital lobe would affect the visual field on the right side, due to the way visual pathways cross over. Additionally, occipital lobe lesions often produce homonymous hemianopia with macular sparing rather than isolating the inferior quadrant on one side.
D) Optic Chiasm
- Explanation: Incorrect. Lesions at the optic chiasm often affect the crossing fibers from the nasal hemiretinas, leading to bitemporal hemianopia (loss of the outer halves of the visual fields in both eyes). The optic chiasm does not typically produce quadrantopia unless the lesion is localized to only part of the chiasm, which is uncommon and unlikely to produce isolated inferior quadrantanopia. Typical lesions of the optic chiasm are due to a pituitary mass/ adenoma.
E) Right Optic Nerve
- Explanation: Incorrect. A lesion in the right optic nerve would cause monocular vision loss in the right eye rather than a quadrant-specific deficit in both eyes. Monocular vision loss does not lead to quadrant-specific visual field defects, such as a left inferior quadrantanopia.
Question 61)
Correct answer option: B
B) Retinoblastoma
- Explanation: This is the correct answer. Retinoblastoma is a serious and common cause of leukocoria in young children, often appearing as a white reflection in the pupil, referred to as a “cat’s eye reflex.” It can lead to symptoms like strabismus or difficulty with depth perception, which might cause the child to bump into objects. Retinoblastoma is an urgent medical condition that requires prompt ophthalmologic evaluation and intervention. The age of the child, along with the sudden behavioral symptoms and white reflex observed in photographs, is highly suggestive of retinoblastoma.
A) Congenital Cataract
- Explanation: Congenital cataracts can cause leukocoria due to the clouding of the lens, which reflects light abnormally. This condition is usually diagnosed at birth or shortly after, as it often causes noticeable visual impairment early on. While congenital cataracts can cause a white pupillary reflex, they typically produce a cloudy or gray appearance rather than a bright white reflection. It can cause impaired vision in the affected eye, but it’s less likely to be associated with the recent onset of bumping into objects, making it a less likely diagnosis here.
C) Optic Neuritis
- Explanation: Optic neuritis is an inflammation of the optic nerve that can lead to visual symptoms such as blurred or dim vision, colour vision loss, and even pain with eye movement. However, optic neuritis does not cause leukocoria (white pupillary reflex) and is rare in young children. Optic neuritis typically presents with decreased vision, but it would not produce a visible reflection in the pupil in photographs, making this diagnosis unlikely in this case.
D) Glaucoma
- Explanation: Paediatric glaucoma, particularly congenital glaucoma, caused by a buildup of fluid in the eye, which increases pressure and damages the optic nerve can cause symptoms such as a cloudy cornea, excessive tearing, and light sensitivity. It does not typically cause leukocoria. While untreated glaucoma can result in visual impairment, the main clinical signs would be different, such as an enlarged eye (buphthalmos) or a bluish corneal haze, rather than a white reflex in the pupil. Therefore, glaucoma is not a likely cause of the leukocoria and bumping into objects in this scenario.
E) Retinal Detachment
- Explanation: Retinal detachment can cause vision loss, and in some cases, it might lead to leukocoria if it results in significant retinal damage or fibrosis. However, retinal detachment in very young children is rare unless it is secondary to trauma or an underlying condition like retinoblastoma or Coats disease. In this case, the symptoms of a white reflex in photographs combined with visual difficulties are more characteristic of retinoblastoma, which is more commonly associated with leukocoria in young children. Therefore, while retinal detachment could contribute to visual issues, it is less likely to be the primary cause of leukocoria here.
Question 62)
Correct Answer: E) Eustachian Tube Dysfunction
E) Eustachian Tube Dysfunction
- Explanation: Correct. Eustachian Tube Dysfunction (ETD) can cause a sensation of fullness, intermittent hearing loss, and sometimes tinnitus due to an inability to equalize pressure in the middle ear. This leads to retraction of the tympanic membrane and conductive hearing loss, which fits with this patient’s presentation. Chronic ETD can cause symptoms to persist over time, making it the most likely diagnosis for her complaints.
Explanation of Answer Options:
A) Otosclerosis
- Explanation: Incorrect. Otosclerosis is a disease characterized by abnormal bone growth around the stapes bone in the middle ear, leading to conductive hearing loss. It often presents with progressive hearing loss and may affect both ears over time. However, otosclerosis typically does not cause a sensation of fullness or intermittent symptoms. Additionally, tympanic membrane retraction is not a typical finding in otosclerosis, making this diagnosis less likely.
B) Acute Otitis Media
- Explanation: Incorrect. Acute Otitis Media (AOM) usually presents with symptoms such as ear pain, fever, and possibly drainage, often in the context of a recent upper respiratory infection. The tympanic membrane is typically red and bulging, rather than retracted. Given the chronic nature of this patient’s symptoms and the absence of pain or infection signs, AOM is unlikely in this case.
C) Cholesteatoma
- Explanation: Incorrect. Cholesteatomas are abnormal skin growths that can develop in the middle ear behind the tympanic membrane. They can cause chronic ear drainage, conductive hearing loss, and sometimes a foul-smelling discharge. A retracted tympanic membrane may be observed, but cholesteatomas are usually associated with persistent drainage or a history of chronic ear infections, neither of which this patient reports.
D) Meniere’s Disease
- Explanation: Incorrect. Meniere’s Disease is a disorder of the endolymphatic system – increased endolymph production or reduced absorption → increased pressure and distention of membranous labyrinth. Typically presents with the triad of vertigo, fluctuating hearing loss, and tinnitus. They may also have a feeling of fullness in the affected ear. However, it generally causes sensorineural rather than conductive hearing loss and is often accompanied by episodes of vertigo, which the patient does not report. This makes Meniere’s Disease a less likely diagnosis.
Question 63)
Correct Answer: C) right sided Hemisensory Loss
C) Hemisensory Loss
- Explanation: Correct. The thalamus is a critical relay center for sensory pathways, particularly the ventral posterior nucleus, which processes sensory signals from the body. A thalamic infarction commonly leads to contralateral hemisensory loss affecting touch, pain, temperature, and proprioception. In this case, the patient’s symptoms of right-sided numbness and tingling are characteristic of a thalamic stroke, making hemisensory loss the most likely symptom.
Explanation of Answer Options:
A) ipsilateral left Hemiparesis
- Explanation: Incorrect. While thalamic infarction typically causes Hemiparesis, (weakness on one side of the body), It is contralateral hemiparesis (weakness on opposite side of body) therefore you would get right sided motor weakness hence this answer option is incorrect.
B) Hemianopia
- Explanation: Incorrect. Hemianopia, or loss of vision in half of the visual field, usually results from lesions in the optic tract, optic radiations, or occipital lobe, rather than the thalamus. The thalamus does play a role in processing visual information, but an isolated thalamic infarct typically does not produce visual field defects. Hemianopia is therefore an unlikely symptom in this case.
D) Aphasia
- Explanation: Incorrect. Aphasia, or difficulty with language, is generally associated with damage to the left cerebral cortex, particularly the Broca’s (left frontal) or Wernicke’s areas (left temporal) in the dominant hemisphere. While thalamic infarctions may occasionally lead to cognitive changes or mild confusion, they do not typically cause aphasia directly. This makes aphasia an unlikely symptom for a thalamic infarct.
E) Ataxia
- Explanation: Incorrect. Ataxia, or lack of voluntary coordination of muscle movements, is more commonly associated with cerebellar lesions or damage to the cerebellar pathways rather than isolated thalamic lesions. Thalamic infarcts may cause sensory disturbances that can indirectly impact coordination, but they do not directly cause ataxia. Thus, it is not the most likely symptom in this patient.
Question 64)
Correct Answer: C) Cluster Headache
- Explanation: Correct. Cluster headaches are characterized by severe, unilateral periorbital pain(around the eye or temple), often described as a stabbing or burning sensation. They occur in “clusters,” with multiple daily attacks lasting 15-180 minutes over a period of weeks to months, often at the same time each day. Associated ipsilateral autonomic symptoms on the same side as the pain—such as lacrimation (tearing), rhinorrea (nasal congestion), and eye redness—are classic features. The patient’s description of daily, intense, unilateral headaches with these autonomic symptoms makes cluster headache the most likely diagnosis.
Explanation of Answer Options:
A) Migraine
- Explanation: Incorrect. Migraines are typically characterized by moderate to severe, throbbing pain, often on one side of the head. They usually last from a few hours to several days and are often accompanied by nausea, vomiting, and sensitivity to light or sound. Migraines may present with an aura or warning symptoms, but they do not usually involve daily, short-lived attacks like those described. The pattern of daily, short, intense, and strictly unilateral episodes, as well as associated autonomic symptoms (tearing, nasal congestion, and eye redness), makes migraine less likely.
B) Tension Headache
- Explanation: Incorrect. Tension headaches are usually described as a bilateral, dull, and pressing or tightening pain, often feeling like a band around the head. They are typically mild to moderate in intensity and lack the autonomic features (like tearing and nasal congestion) described here. Additionally, tension headaches are generally not severe enough to cause the level of excruciating pain reported by the patient, making this diagnosis unlikely.
D) Temporal Arteritis
- Explanation: Incorrect. Temporal arteritis, or giant cell arteritis is a condition where the arteries, particularly those at the side of the head (the temples), become inflamed. This usually affects older adults and is associated with a throbbing temporal headache, scalp tenderness, and jaw claudication (pain with chewing). It can lead to visual disturbances and, if untreated, may result in blindness. Temporal arteritis typically does not present with acute, short-lived attacks as described here, and autonomic symptoms like tearing and nasal congestion are not common, making this diagnosis unlikely.
E) Trigeminal Neuralgia
- Explanation: Incorrect. Trigeminal neuralgia causes brief, severe, electric-shock-like facial pain, often triggered by touch, eating, or talking. The episodes are typically very short, lasting only seconds to a couple of minutes, and occur multiple times a day. Trigeminal neuralgia pain is not usually associated with autonomic symptoms such as tearing or nasal congestion. Given the longer duration of the attacks (45 minutes) and the associated autonomic symptoms, trigeminal neuralgia is less likely in this case.
Question 65)
Correct Answer: B) Bacterial Meningitis
B) Bacterial Meningitis
- Explanation: Correct. Bacterial meningitis commonly presents with a common triad of headache, fever, neck stiffness. They may also show altered mental status, which are all seen in this patient. The CSF findings typically show elevated protein, decreased glucose, and a high white blood cell count with a predominance of neutrophils. This combination of clinical features and CSF findings is characteristic of bacterial meningitis, making it the most likely diagnosis in this case. Immediate treatment with antibiotics is critical due to the potentially life-threatening nature of the condition. Common pathogens are pneumococcus and meningococcus.
Explanation of Answer Options:
A) Bacterial encephalitis
- Explanation: Incorrect. Bacterial encephalitis (infection of the brain tissue) can be caused by a range of bacterial diseases such as chlamydia. Typical symptoms include fever, altered mental status, and focal neurological signs, often without the neck stiffness typical of meningitis. Therefore this is not the correct answer.
C) Brain Abscess
- Explanation: Incorrect. A brain abscess may present with headache, fever, and focal neurological deficits, but neck stiffness is less common unless the abscess ruptures into the ventricles or is associated with meningitis. CSF findings in cases of an unruptured brain abscess are often non-specific and may show elevated protein but normal glucose levels, unlike the findings in this patient. A brain abscess is usually identified through imaging studies like CT or MRI, which are not mentioned here.
D) Viral Encephalitis
- Explanation: Incorrect. Viral encephalitis, such as herpes simplex (HSV2) encephalitis, presents with fever, altered mental status, and focal neurological signs, often without the neck stiffness typical of meningitis. CSF analysis in viral encephalitis typically shows elevated protein and normal glucose with lymphocytic predominance, rather than the neutrophilic predominance and decreased glucose seen in this patient. Additionally, the primary symptoms are often confusion, behavioural changes, and seizures rather than the classic triad of meningitis symptoms.
E) Fungal Meningitis
- Explanation: Incorrect. Fungal meningitis tends to affect immunocompromised patients (e.g., those with HIV/AIDS) and usually has a more subacute or chronic onset compared to bacterial meningitis. CSF findings typically show elevated protein, decreased glucose, and lymphocytic predominance. While some features of fungal meningitis may overlap with bacterial meningitis, the patient’s acute presentation and the neutrophil-predominant CSF findings make bacterial meningitis more likely in this case.
Question 66)
Correct answer: D
- D) Conduction aphasia (Correct Answer): Patients with conduction aphasia struggle with repetition due to damage in the arcuate fasciculus, which connects Broca’s and Wernicke’s areas. Their comprehension is intact, but they often make phonemic errors and have difficulty repeating sentences, as seen in this patient.
Explanation:
- A) Broca’s aphasia: Typically presents with non-fluent, effortful speech and good comprehension, but there is a marked difficulty in speech production, which isn’t a primary feature in this case.
- B) Wernicke’s aphasia: Characterized by poor comprehension and fluent, nonsensical speech. This patient has good comprehension.
- C) Guillain Barre syndrome: This is an autoimmune disease where patients’ own antibodies attack the patient’s peripheral nervous system. Now whilst this disease can cause issues with speech due to Dysarthria (inability to produce speech well due to poor motor control of vocal muscles) This patient has no motor issues and also no muscle weakness which is commonly seen in patients with GBS. Furthermore GBS patients typically have an infection e.g campylobacter which ends up causing this disease.
- E) Freidrech’s ataxia: This is an autosomal recessive non poly Q triplet repeat disorder, which causes a triplet repeat mutation in nuclear DNA responsible for mitochondrial function. Now whilst this disease can cause issues with speech due to Dysarthria (inability to produce speech well due to poor motor control of vocal muscles) This patient has no motor issues and also no muscle weakness which is commonly seen in patients with friedreich’s ataxia e.g. spastic paraparesis (leg stiffness).
Question 67)
Correct Answer: D
D) Brown-Séquard syndrome (Correct Answer): Brown-Séquard syndrome occurs due to a damaged hemisection of the spinal cord, leading to ipsilateral motor weakness and loss of proprioception/vibration below the lesion, along with contralateral loss of pain and temperature sensation. This patient’s presentation fits this classic pattern.
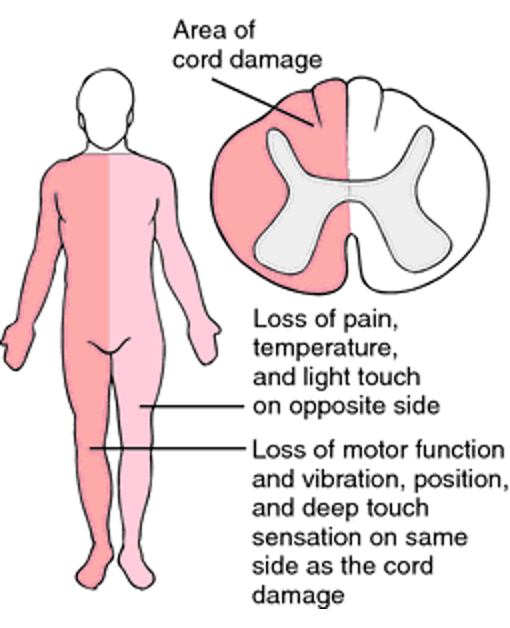
Remaining options
- A) Amyotrophic lateral sclerosis (ALS): ALS typically presents with both upper and lower motor neuron signs, but it does not cause any sensory loss as seen in this patient.
- B) Guillain-Barré syndrome: Guillain-Barré is a rapidly progressive, ascending paralysis that affects motor function, but it does not involve the characteristic sensory deficits seen here.
- C) Multiple sclerosis: While multiple sclerosis can present with a variety of motor and sensory symptoms, it typically involves a relapsing-remitting course and would not lead to this distinct pattern of motor weakness and sensory loss. It is also a chronic condition therefore would take a lot of time to develop these symptoms whereas this is acute due to the motor crash.
- E) Anterior spinal artery syndrome: This condition leads to bilateral loss of motor function and pain/temperature sensation below the level of injury, and also loss of the spinothalamic tract (pain and temperature) however it spares the Dorsal column therefore keeping vibration and proprioception intact, unlike the presentation in this patient.
Question 68)
Correct answer: B
- B) Epidural hemorrhage (Correct Answer): An epidural hemorrhage (EDH) often results from trauma, particularly the pterion causing injury to the middle meningeal artery. The characteristic clinical course involves an initial loss of consciousness, followed by a lucid interval, and then rapid neurological deterioration (as seen with this patient). The biconvex (lentiform) hyperdensity (like an American football shape) on CT scan is classic for an epidural hemorrhage.
Remaining options Explanation:
- A) Subarachnoid hemorrhage: This typically presents with a “thunderclap” headache, and while trauma can cause subarachnoid hemorrhage, the CT findings of a biconvex shape are not typical for subarachnoid hemorrhage, which usually shows blood in the basal cisterns or sulci. Typically a subarachnoid hemorrhage has a star-like shape bleed in a CT scan, and occurs due to rupture of berry aneurysms of the middle cerebral artery
- C) Subdural hemorrhage: This type of hemorrhage occurs from tearing of the subdural bridging veins, often in elderly or alcohol-dependent individuals, leading to a crescent-shaped hyperdensity– looks like a banana on CT. Subdural hemorrhages tend to have a slower progression compared to epidural hemorrhages and usually do not present with the rapid neurological decline seen here.
- D) Cerebral contusion: While cerebral contusions can occur following head trauma and may present with neurological symptoms, the CT scan in this case clearly shows a biconvex hyperdense, which is not typical of a contusion. Contusions usually appear as areas of mixed density with surrounding edema.

- E) Intracerebral hemorrhage: This refers to bleeding within the brain parenchyma and is usually caused by hypertension or trauma. The bleeding would appear within the brain tissue on CT, rather than as a biconvex extra-axial collection, as seen with an epidural hemorrhage. This is seen typically due to charcot bouchard aneurysms (small vessel aneurysm)

Question 69)
Correct answer: D
D) Parkinson’s disease (Correct Answer): Parkinson’s disease is a common autosomal dominant neurodegenerative disorder due to the degeneration of the substantia nigra reducing dopamine, it is characterized by bradykinesia, resting tremor, rigidity, and postural instability. This patient’s symptoms, including tremor, bradykinesia, stiffness, and decreased facial expression (hypomimia), are classic features of Parkinson’s disease. The micrographia (small handwriting) and the “cogwheel” rigidity on examination further point to this diagnosis.
Incorrect answer Explanation:
- A) Amyotrophic lateral sclerosis (ALS): ALS primarily affects motor neurons, leading to progressive weakness and muscle wasting, but it typically does not present with tremors, bradykinesia, or rigidity. ALS primarily involves upper and lower motor neuron signs, such as muscle fasciculations and spasticity, which are not described in this case.
- B) Huntington’s disease: Huntington’s disease is an autosomal dominant neurodegenerative disorder due to a mutation on Chromosome 4 leading to buildup of hunting proteins causing the degradation of the caudate nucleus which causes less D2 receptors and overstimulation of the indirect pathway. It is typically characterized by chorea (involuntary, jerky movements), psychiatric disturbances, and cognitive decline. While it does affect movement, the patient in this case presents with bradykinesia and rigidity, which are more characteristic of Parkinson’s disease rather than Huntington’s choreiform movements.
- C) Multiple system atrophy (MSA): MSA is a neurodegenerative disorder that can present with Parkinsonism, but it is also associated with autonomic dysfunction (e.g., orthostatic hypotension, bladder dysfunction), and more widespread cerebellar ataxia, which are not mentioned in this patient’s presentation.
- E) Wilson’s disease: Wilson’s disease is a rare disorder of copper metabolism that can affect the liver and brain, leading to movement disorders. While it can cause Parkinsonism-like symptoms due to copper deposition in the basal ganglia, it usually presents earlier in life (teens or young adults) and is associated with liver disease and psychiatric symptoms. There is no mention of these in the patient’s history.
Question 70)
Correct Answer: C
- C) Lewy body dementia (Correct Answer): Lewy body dementia is characterized by episodicmemory impairment, fluctuating cognition, visual hallucinations, and Parkinsonism (e.g., bradykinesia, stiffness). The presence of vivid visual hallucinations and movement difficulties in this patient, along with fluctuating mental status, strongly suggests Lewy body dementia. This is distinct from other forms of dementia in that it often involves both cognitive and motor symptoms early on.
Explanation:
- A) Alzheimer’s disease: Alzheimer’s disease typically presents with progressive episodic memory loss and cognitive decline, but it does not typically involve visual hallucinations, fluctuating cognition, or prominent Parkinsonism, which are key features of Lewy body dementia. Alzheimer’s patients may develop these symptoms later, but they are not early or prominent features.
- B) Vascular dementia: Vascular dementia is caused by multiple small strokes or other vascular issues. It often presents with a stepwise decline in cognitive function, focusing on executive dysfunction rather than the vivid hallucinations or fluctuating cognition seen here. The associated Parkinsonism also makes vascular dementia less likely.
- D) Frontotemporal dementia: Frontotemporal dementia typically affects behavior and languageearly in the disease process, with personality changes and disinhibition being common symptoms. Memory impairment is less prominent early on, and the visual hallucinations and Parkinsonismseen in this case are not features of frontotemporal dementia.
- E) Normal pressure hydrocephalus (NPH): NPH is associated with the triad of gait disturbance, urinary incontinence, and dementia. While the shuffling gait could be suggestive of NPH, the presence of visual hallucinations and Parkinsonism makes Lewy body dementia more likely, as these are not characteristic of NPH.
Question 71)
Correct answer: A
- A) Charcot-Marie-Tooth disease type 1 (CMT1) (Correct Answer): CMT1 is the most common subtype of Charcot-Marie-Tooth disease, a hereditary motor and sensory neuropathy. It is a demyelinating disorder, leading to slowed nerve conduction velocities, distal muscle wasting, weakness (especially foot drop), and sensory loss in a stocking-glove distribution. The family history, gradual progression, and high-arched feet (pes cavus) are also classic findings of CMT1. The involvement of both motor and sensory nerves with slow progression differentiates CMT1 from other conditions.
Incorrect answer Explanations:
- B) Spinal muscular atrophy (SMA) is a genetic disorder affecting lower motor neurons in the spinal cord, leading to muscle weakness and atrophy. However, SMA typically presents with proximal weakness rather than distal weakness and does not typically cause sensory symptoms or foot drop. The age of onset and the pattern of weakness do not match this condition, making it an unlikely diagnosis for this patient.
- C) Guillain-Barré syndrome (GBS) is an acute inflammatory demyelinating polyneuropathy characterized by rapid-onset muscle weakness, often following a viral infection. While GBS can lead to motor weakness and sensory changes, it typically presents with ascending weakness, affecting the legs first and then potentially progressing to the upper body. The gradual onset and chronicity of symptoms in this patient, along with a family history, make GBS an unlikely diagnosis. Furthermore it typically occurs following an infection which is not mentioned here.
- D) Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease affecting upper and lower motor neurons. ALS typically causes both upper and lower motor neuron signs, leading to muscle weakness, spasticity, and bulbar symptoms. However, the presence of sensory symptoms (e.g., stocking-glove distribution) and the absence of upper motor neuron signs in this patient suggest that ALS is not the correct diagnosis. Additionally, the family history and the specific nature of the weakness align more with a hereditary neuropathy.
- E) Hereditary spastic paraplegia (HSP): HSP primarily affects the upper motor neurons, leading to progressive spasticity and weakness in the legs, but it does not cause the distal sensory loss and foot deformities (like pes cavus) characteristic of CMT1. Nerve conduction studies in HSP would also be normal, as the pathology is in the central nervous system, rather than the peripheral nerves.
Question 72)
Correct answer: A
- A) Ideomotor apraxia (Correct Answer): Ideomotor apraxia is characterized by an inability to correctly perform a learned motor task on command, despite understanding the task. Patients can describe how to perform the action, but they cannot execute it. The issue arises from the disconnectionbetween the conceptual knowledge of an action and its execution.
Incorrect Answer Explanations:
- B) Ideational apraxia: In ideational apraxia, the patient loses the ability to plan and sequence multi-step actions, often leading to incorrect order of tasks or misuse of objects (e.g., using a comb to brush teeth). This differs from ideomotor apraxia, where patients retain the knowledge of the task but struggle with the motor execution. Damage here is often more widespread, involving the prefrontal cortex or the parietal lobes.
- C) Constructional apraxia: This type of apraxia affects the ability to draw or construct objects (e.g., copying shapes or building structures). It is commonly associated with damage to the right parietal lobe, leading to issues with spatial awareness. This patient’s primary difficulty is performing learned motor tasks, not spatial construction, which makes constructional apraxia less likely.
- D) Buccofacial apraxia: Also known as orofacial apraxia, this type specifically affects the ability to perform coordinated movements involving the face, mouth, or tongue (e.g., whistling or blowing). It is associated with damage to the frontal or insular regions of the brain. Since this patient’s difficulty lies in performing general motor tasks, not facial movements, buccofacial apraxia is unlikely.
- E) Limb-kinetic apraxia: Limb-kinetic apraxia is a disorder in which fine, precise movements of the limbs are impaired, leading to clumsy or imprecise actions. This can occur with damage to the premotor cortex or basal ganglia. Unlike ideomotor apraxia, limb-kinetic apraxia involves difficulty with the fine control of movements rather than a disconnect between knowledge of the task and execution.
Question 73)
Correct answer: A
- A) Arnold-Chiari malformation (Correct Answer): Arnold-Chiari malformation is when the lower part of the brain pushes down into the spinal canal and may cause altered flow of CSF. Can result in no clinical presentation but may prevent CSF from shunting. A severe example would be some of the cerebellum extending down into the foramen magnum and potentially obstructing CSF flow. This can cause non- communicating hydrocephalus by obstructing CSF flow. The patient’s symptoms of headache, blurry vision, neck pain, coordination problems, combined with the cerebellar herniation, strongly suggest Arnold-Chiari malformation as the underlying cause.
Incorrect answer Explanations:
- B) Meningitis: Meningitis can cause communicating hydrocephalus due to inflammation and scarring of the arachnoid villi, which impairs CSF absorption. However, meningitis typically presents with fever, neck stiffness, and signs of acute infection, none of which are mentioned in this case. While meningitis can lead to hydrocephalus, the MRI finding of cerebellar herniation is more indicative of Arnold-Chiari malformation.
- C) Choroid plexus papilloma: Choroid plexus papilloma is a rare tumor that leads to overproduction of CSF, causing communicating hydrocephalus without an obstructive cause. This condition would lead to ventricular enlargement but without herniation of brain structures or other signs of obstruction. The imaging finding of cerebellar herniation seen in this patient is not typical of choroid plexus papilloma, making this diagnosis unlikely.
- D) Subarachnoid hemorrhage: Subarachnoid hemorrhage (SAH) can lead to communicating hydrocephalus when blood obstructs the absorption of CSF at the arachnoid villi. However, SAH typically presents with a sudden onset of a severe headache (“thunderclap” headache), often accompanied by loss of consciousness or other signs of acute hemorrhage. The absence of such acute symptoms and the MRI findings make subarachnoid hemorrhage less likely in this case.
- E) Aqueductal stenosis: Aqueductal stenosis is a common cause of non-communicating hydrocephalus, where the cerebral aqueduct between the third and fourth ventricles becomes blocked, causing ventricular dilation proximal to the obstruction (lateral and third ventricles). This patient’s MRI shows the presence of cerebellar tonsil herniation makes aqueductal stenosis unlikely as the underlying cause.
Question 74)
Correct answer option: C
C) Arteriovenous malformation (AVM) (Correct Answer)
Explanation: An arteriovenous malformation (AVM) is a congenital vascular malformation due to an abnormal direct connection between an artery and a vein which results in conflicting pressures and leads it liable to rupturing. This is the most common cause under 45-year olds. This can lead to intracerebral hemorrhage.This is a common cause of hemorrhagic strokes in younger individuals, making it the most likely underlying cause in this scenario. The sudden onset of symptoms in a young patient is consistent with an AVM rupture.
Incorrect Answer Explanations:
A) Hypertension
- Explanation: Hypertension is the most common cause for intracerebral hemorrhage, especially in older patients. hypertension could lead to the rupture of aneurysms in small penetrating vessels (charcot- Bouchard aneurysm) in the brain, causing hemorrhage. While it’s a plausible cause, it may be less common in patients as young as 35 compared to other options.
B) Cerebral amyloid angiopathy
- Explanation: Cerebral amyloid angiopathy (CAA) is characterized by the deposition of amyloid protein in the walls of cerebral blood vessels, leading to increased fragility and a higher risk of hemorrhage. CAA is more common in elderly patients, but it can occur in younger individuals, especially those with genetic predispositions. However, it is relatively rare in a 35-year-old without significant risk factors, making this a less likely cause for an acute hemorrhagic stroke in a young patient.
D) Coagulopathy
- Explanation: Coagulopathy, or a bleeding disorder, can lead to intracerebral hemorrhage, especially in individuals with conditions like hemophilia or those on anticoagulation therapy. However, coagulopathy is less likely to be the primary cause of an intracerebral hemorrhage in a previously healthy 35-year-old without any known bleeding disorders or recent anticoagulation use. While this is a potential cause, it is not as common as AVMs in this age group.
E) Trauma
Explanation: Trauma can certainly cause intracerebral hemorrhage, particularly in younger individuals. However, in the absence of a reported history of recent head injury, this option is less likely. While traumatic hemorrhages typically occur due to falls or accidents, the sudden onset of symptoms without an identified mechanism suggests a non-traumatic cause.
Question 75:
Which of the following mechanisms is most associated with the pathophysiology of Huntington’s disease?
a) Loss of function mutations in mitochondrial DNA
b) Trinucleotide expansion of CAG repeats leading to toxic gain of function
c) Antibody-mediated destruction of voltage-gated calcium channels
d) Autosomal recessive inheritance leading to enzyme deficiencies
e) Mutation in nuclear frataxin gene impairing mitochondrial function
Correct answer: b) Trinucleotide expansion of CAG repeats leading to toxic gain of function
Explanation:
- Correct (b): Huntington’s disease is caused by an expansion of CAG trinucleotide repeats in the HTTgene, leading to a toxic gain of function of the huntingtin protein. This results in neurodegeneration, primarily affecting the basal ganglia and cortex
- Incorrect (a): Mitochondrial DNA mutations are more commonly associated with mitochondrial disorders such as mitochondrial myopathy or Leber’s hereditary optic neuropathy.
- Incorrect (c): Antibody-mediated destruction of voltage-gated calcium channels is characteristic of Lambert-Eaton myasthenic syndrome, not Huntington’s disease
- Incorrect (d): Huntington’s disease is inherited in an autosomal dominant manner, not recessive. Autosomal recessive conditions are typically linked to enzyme deficiencies.
- Incorrect (e): Frataxin gene mutations are implicated in Friedreich’s ataxia, not Huntington’s disease
Question 75:
A patient presents with progressive muscle weakness and is diagnosed with Myasthenia Gravis. The pathophysiology of this condition primarily involves:
a) Autoantibodies against presynaptic calcium channels
b) Autoantibodies against postsynaptic acetylcholine receptors
c) Trinucleotide repeat expansion leading to glutamine accumulation
d) Mitochondrial dysfunction leading to impaired ATP production
e) Antibody-mediated damage to the blood-brain barrier
Correct answer: b) Autoantibodies against postsynaptic acetylcholine receptors
Explanation:
- Correct (b): Myasthenia Gravis is an autoimmune disorder in which antibodies targets nicotininic acetylcholine receptors at the postsynaptic neuromuscular junction, impairing neuromuscular transmission and leading to muscle weakness
- Incorrect (a): Autoantibodies against presynaptic calcium channels are characteristic of Lambert-Eaton myasthenic syndrome, not Myasthenia Gravis
- Incorrect (c): Trinucleotide repeat expansions are linked to conditions like Huntington’s disease and some ataxias, not Myasthenia Gravis
- Incorrect (d): Mitochondrial dysfunction and ATP production issues are characteristic of mitochondrial myopathies, not Myasthenia Gravis
- Incorrect (e): Damage to the blood-brain barrier can occur in conditions like multiple sclerosis, but this is not the primary mechanism in Myasthenia Gravis.
Question 76:
Which of the following best describes the pathophysiology of paraneoplastic syndromes?
a) Direct metastasis of cancer cells to the CNS
b) Inflammatory damage due to tumour necrosis
c) Autoimmune attack on nervous system structures triggered by tumour antigens
d) Increased intracranial pressure due to space-occupying lesions
e) Compression of the spinal cord by a tumour
Correct answer: c) Autoimmune attack on nervous system structures triggered by tumour antigens
Explanation:
- Correct (c): Paraneoplastic syndromes occur when the immune system attacks normal tissue in response to antigens expressed by a tumour, leading to neurological symptoms.
- Incorrect (a): Paraneoplastic syndromes are not caused by direct metastasis of cancer to the CNS.
- Incorrect (b): While tumour necrosis can cause local inflammation, paraneoplastic syndromes are autoimmune in nature.
- Incorrect (d): Increased intracranial pressure is not the main mechanism behind paraneoplastic syndromes.
- Incorrect (e): Spinal cord compression can occur in cancer, but it is not related to the autoimmune mechanisms in paraneoplastic syndromes.
Question 77:
Which of the following neurotransmitters is primarily inhibitory in the central nervous system?
a) Acetylcholine
b) Glutamate
c) GABA
d) Dopamine
e) Serotonin
Correct answer: c) GABA
Explanation:
- Correct (c): GABA (gamma-aminobutyric acid) is the main inhibitory neurotransmitter in the central nervous system.
- Incorrect (a): Acetylcholine is typically excitatory in the CNS.
- Incorrect (b): Glutamate is the primary excitatory neurotransmitter in the CNS.
- Incorrect (d): Dopamine has various functions and can be excitatory or inhibitory depending on the pathway.
- Incorrect (e): Serotonin is primarily modulatory and can be excitatory or inhibitory.
Question 78:
A patient with a mitochondrial disorder most likely exhibits which of the following symptoms?
a) Chronic liver failure
b) Muscle weakness and exercise intolerance
c) Hypertension
d) Haemolytic anaemia
e) Peripheral neuropathy without motor involvement
Correct answer: b) Muscle weakness and exercise intolerance
Explanation:
- Correct (b): Correct (b): Muscle weakness and exercise intolerance are hallmark symptoms of mitochondrial disorders due to impaired oxidative phosphorylation. Since mitochondria are responsible for energy production (via ATP) in cells, tissues with high energy demands, such as skeletal muscles, are particularly affected. As a result, these patients often experience fatigue, muscle cramps, and difficulty with physical exertion. In severe cases, mitochondrial myopathies can also lead to progressive muscle degeneration and involvement of other organ systems
- Incorrect (a): While mitochondrial dysfunction can potentially affect the liver, chronic liver failure is not the most common presentation. In some specific mitochondrial disorders, like Mitochondrial DNA depletion syndromes, the liver might be involved, but this is far less frequent compared to muscular symptoms. Liver involvement, when present, usually occurs later in the disease course or in the context of more complex systemic involvement.
- Incorrect (c): Hypertension is not a direct manifestation of mitochondrial disorders. These disorders typically result in multisystemic dysfunction, with a focus on energy-demanding tissues, such as muscles and the central nervous system. Cardiovascular symptoms, when they occur, are more likely to involve heart muscle issues (e.g., cardiomyopathy), rather than blood pressure regulation problems.
- Incorrect (d): Haemolytic anaemia involves the destruction of red blood cells and is not a key feature of mitochondrial disorders. Although some rare mitochondrial diseases can involve bone marrow dysfunction, resulting in various cytopenias, mitochondrial disorders primarily present with neuromuscular or metabolic issues rather than haemolysis.
- Incorrect (e): Peripheral neuropathy can occur in mitochondrial disorders but usually involves both motor and sensory components. The neuropathy is often due to the energy deficits affecting nerves, leading to a mixed sensory-motor polyneuropathy. A purely sensory neuropathy without motor involvement would be atypical for mitochondrial diseases.
Question 79:
In Parkinson’s disease, which of the following is the primary neurotransmitter deficiency?
a) Serotonin
b) Acetylcholine
c) Dopamine
d) Glutamate
e) GABA
Correct answer: c) Dopamine
Explanation:
- Correct (c): Parkinson’s disease is primarily caused by the loss of dopaminergic neurons in the substantia nigra, leading to a deficiency in dopamine, which is crucial for motor control.
- Incorrect (a): Serotonin levels may be altered in Parkinson’s disease but are not the primary deficiency.
- Incorrect (b): Acetylcholine is involved in Parkinson’s, but it’s the imbalance caused by the loss of dopamine that affects motor function.
- Incorrect (d): Glutamate is an excitatory neurotransmitter, but its deficiency is not linked to the hallmark motor symptoms of Parkinson’s.
- Incorrect (e): GABA is inhibitory, and while it plays a role in neurotransmission, its deficiency is not central to Parkinson’s disease pathology.
Question 80:
Which of the following types of neoplastic progression is most closely associated with the loss of cellular differentiation and aggressive growth?
a) Hyperplasia
b) Metaplasia
c) Dysplasia
d) Anaplasia
e) Hypertrophy
Correct answer: d) Anaplasia
Explanation:
- Correct (d): Anaplasia refers to the complete loss of differentiation and cellular structure, a hallmark of malignant and aggressive cancers.
- Incorrect (a): Hyperplasia is the increase in the number of cells, but these cells maintain normal differentiation.
- Incorrect (b): Metaplasia is the replacement of one cell type by another but is not indicative of aggressive cancer.
- Incorrect (c): Dysplasia refers to disordered growth, a precancerous state, but it does not involve the loss of cellular differentiation seen in anaplasia.
- Incorrect (e): Hypertrophy is an increase in cell size, not related to cancer or differentiation loss.
Question 81:
In Huntington’s Disease, the pathological accumulation of abnormal huntingtin protein is most likely to affect which brain region?
a) Cerebellum
b) Substantia nigra
c) Hippocampus
d) Basal ganglia
e) Motor cortex
Correct answer: d) Basal ganglia
Explanation:
- Correct (d): The basal ganglia, particularly the striatum, are heavily affected in Huntington’s Disease, leading to motor dysfunctions such as chorea.
- Incorrect (a): The cerebellum is responsible for coordination, and while atrophy can occur, it is not the primary region affected in Huntington’s Disease.
- Incorrect (b): The substantia nigra is primarily affected in Parkinson’s disease, not Huntington’s.
- Incorrect (c): The hippocampus is mainly involved in memory but is not the primary target in Huntington’s Disease.
- Incorrect (e): The motor cortex plays a role in voluntary movement, but the basal ganglia are more directly affected in Huntington’s Disease.
Question 82:
A patient presents with signs of a haemorrhagic stroke. What is the most common cause of subarachnoid haemorrhage in young adults?
a) Rupture of an arteriovenous malformation
b) Intracerebral haemorrhage due to hypertension
c) Ruptured berry aneurysm
d) Subdural hematoma from trauma
e) Cortical vein thrombosis
Correct answer: c) Ruptured berry aneurysm
Explanation:
- Correct (c): Berry aneurysms are the most common cause of subarachnoid haemorrhage, particularly in younger adults, and typically arise from arterial bifurcations normally in the Circle of Willis.
- Incorrect (a): Arteriovenous malformations can cause haemorrhage but are less common than aneurysms.
- Incorrect (b): Hypertension is a major cause of intracerebral haemorrhage but not specifically subarachnoid haemorrhage.
- Incorrect (d): Subdural hematomas result from trauma but do not cause subarachnoid haemorrhage.
- Incorrect (e): Cortical vein thrombosis is a rare cause of haemorrhage and not commonly associated with subarachnoid haemorrhage.
Question 83:
Which of the following is a key risk factor for lacunar infarcts in small vessel ischemic stroke?
a) Atrial fibrillation
b) Diabetes mellitus
c) Hyperlipidemia
d) Hypertension
e) Obesity
Correct answer: d) Hypertension
Explanation:
- Correct (d): Hypertension is the most significant risk factor for lacunar infarcts, which involve the occlusion of small penetrating arteries in the brain(10 Stroke).
- Incorrect (a): Atrial fibrillation is a key risk factor for embolic strokes, not lacunar infarcts.
- Incorrect (b): Diabetes mellitus is a risk factor for vascular disease but is not the primary cause of lacunar infarcts.
- Incorrect (c): Hyperlipidemia contributes to atherosclerosis and larger vessel strokes but is less implicated in lacunar infarcts.
- Incorrect (e): Obesity increases the risk of cardiovascular disease, but hypertension is more closely linked to lacunar infarcts.
Question 84:
Which of the following is a classic sign of raised intracranial pressure (ICP)?
a) Decorticate posturing
b) Cushing’s triad
c) Positive Romberg’s sign
d) Diplopia
e) Bradykinesia
Correct answer: b) Cushing’s triad
Explanation:
- Correct (b): Cushing’s triad (hypertension, bradycardia, and irregular respiration) is a classic sign of raised intracranial pressure, often associated with impending brain herniation(09 Disorders of CSF cir…).
- Incorrect (a): Decorticate posturing is seen in severe brain injury but is not specific to raised ICP.
- Incorrect (c): Romberg’s sign tests for sensory ataxia, not increased ICP.
- Incorrect (d): Diplopia (double vision) may occur with raised ICP but is not as characteristic as Cushing’s triad.
- Incorrect (e): Bradykinesia is a feature of Parkinson’s disease, not raised ICP.
Question 85:
Which of the following conditions is most likely to present with a sudden onset “thunderclap” headache?
a) Lacunar infarct
b) Subarachnoid hemorrhage
c) Brain abscess
d) Ischemic stroke
e) Tension headache
Correct answer: b) Subarachnoid hemorrhage
Explanation:
- Correct (b): Subarachnoid hemorrhage is classically associated with a sudden, severe headache often described as a “thunderclap” headache. It is frequently caused by the rupture of a berry aneurysm(10 Stroke).
- Incorrect (a): Lacunar infarcts typically cause more subtle, progressive symptoms rather than a sudden, severe headache.
- Incorrect (c): Brain abscesses often cause more gradual symptoms like headache, fever, and neurological deficits, but not typically a thunderclap headache.
- Incorrect (d): Ischemic strokes are more likely to present with focal neurological deficits, such as weakness or speech difficulties, not with a severe headache.
- Incorrect (e): Tension headaches are not associated with sudden, severe onset and are usually more chronic or episodic in nature.
Question 86:
Communicating hydrocephalus is typically associated with which of the following symptoms?
a) Hemiplegia, aphasia, and sensory loss
b) Headache, papilledema, and vomiting
c) Gait disturbance, cognitive decline, and urinary incontinence
d) Neck stiffness, fever, and photophobia
e) Seizures, confusion, and hemiparesis
Correct answer: c) Gait disturbance, cognitive decline, and urinary incontinence
Explanation:
- Correct (c): The classic triad of hydrocephalus includes gait disturbance, cognitive decline, and urinary incontinence. These symptoms arise due to impaired CSF absorption leading to ventricular enlargement
- Incorrect (a): These are symptoms typically seen in large ischemic strokes, not in NPH.
- Incorrect (b): These are typical symptoms of raised intracranial pressure, not NPH.
- Incorrect (d): These symptoms are characteristic of meningitis, not NPH.
- Incorrect (e): Seizures and confusion may be associated with encephalitis or hemorrhagic stroke
Question 87:
A 70-year-old patient presents with sudden onset of right-sided weakness and slurred speech. CT scan confirms a stroke. Which artery is most likely involved based on the symptoms?
a) Anterior cerebral artery
b) Middle cerebral artery
c) Posterior cerebral artery
d) Basilar artery
e) Lenticulostriate arteries
Correct answer: b) Middle cerebral artery
Explanation:
- Correct (b): The middle cerebral artery (MCA) supplies the lateral aspects of the cerebral hemispheres, including areas responsible for motor function. Right-sided weakness and slurred speech suggest an infarction in the territory of the MCA, which affects the left hemisphere due to contralateral control(10 Stroke).
- Incorrect (a): The anterior cerebral artery (ACA) primarily affects the lower limbs and may not present with slurred speech.
- Incorrect (c): The posterior cerebral artery (PCA) mainly supplies the occipital lobe and is associated with visual disturbances, not motor deficits.
- Incorrect (d): The basilar artery supplies the brainstem, and a stroke here would typically present with bilateral symptoms or cranial nerve deficits, not just unilateral weakness.
- Incorrect (e): Lenticulostriate arteries supply deep structures of the brain and would lead to motor deficits but typically affect more specific muscle groups rather than broad motor functions like slurred speech.
Question 88:
Which neurological sign is indicative of meningeal irritation in a patient suspected of having meningitis?
a) Babinski’s sign
b) Kernig’s sign
c) Homan’s sign
d) Romberg’s sign
e) Lhermitte’s sign
Correct answer: b) Kernig’s sign
Explanation:
- Correct (b): Kernig’s sign is a classic indicator of meningeal irritation. It is tested by attempting to extend the knee while the hip is flexed at 90 degrees; pain or resistance indicates positive meningeal irritation(08 Infectious Diseases …).
- Incorrect (a): Babinski’s sign is a test for upper motor neuron lesions and is not specific to meningitis.
- Incorrect (c): Homan’s sign is used to assess for deep vein thrombosis, not meningeal irritation.
- Incorrect (d): Romberg’s sign tests proprioception and balance but does not indicate meningeal irritation.
- Incorrect (e): Lhermitte’s sign is an electric shock-like sensation down the spine with neck flexion, often seen in multiple sclerosis, but it is not used to assess meningeal irritation.
Question 89:
A 25-year-old male presents with sudden-onset headaches described as “thunderclap” and a stiff neck. What is the most appropriate initial imaging study to rule out subarachnoid haemorrhage?
a) MRI of the brain
b) CT scan of the brain
c) X-ray of the cervical spine
d) Ultrasound of the carotids
e) Lumbar puncture
Correct answer: b) CT scan of the brain
Explanation:
- Correct (b): A CT scan of the brain is the initial imaging study of choice for ruling out subarachnoid haemorrhage due to its speed and ability to detect acute bleeding(09 Disorders of CSF cir…).
- Incorrect (a): An MRI is more sensitive for detecting subtle changes but is not the first-line study in acute settings.
- Incorrect (c): X-rays of the cervical spine do not assess for intracranial haemorrhage.
- Incorrect (d): Ultrasound of the carotids is used to evaluate for carotid artery disease, not for assessing for subarachnoid hemorrhage.
- Incorrect (e): A lumbar puncture is performed after CT if bleeding is suspected, but it is not the initial imaging modality.
Question 90:
Which type of hydrocephalus is characterized by an accumulation of cerebrospinal fluid (CSF) due to impaired absorption rather than obstruction?
a) Non-communicating hydrocephalus
b) Communicating hydrocephalus
c) Normal pressure hydrocephalus
d) Acute hydrocephalus
e) Congenital hydrocephalus
Correct answer: b) Communicating hydrocephalus
Explanation:
- Correct (b): Communicating hydrocephalus occurs when there is impaired absorption of CSF despite normal flow between ventricles, often seen in conditions like meningitis(09 Disorders of CSF cir…).
- Incorrect (a): Non-communicating hydrocephalus results from an obstruction within the ventricular system, preventing normal CSF flow.
- Incorrect (c): Normal pressure hydrocephalus is a subtype characterized by ventricular enlargement with normal CSF pressure, but it is still linked to impaired absorption.
- Incorrect (d): Acute hydrocephalus can be either communicating or non-communicating and refers to a sudden increase in CSF volume.
- Incorrect (e): Congenital hydrocephalus is present at birth and can be due to a variety of causes, including genetic or developmental anomalies.
Question 91:
Which of the following diseases is most characteristically associated with bradykinesia and rigidity?
a) Huntington’s disease
b) Amyotrophic lateral sclerosis
c) Progressive supranuclear palsy
d) Parkinsonism
e) Corticobasal degeneration
Correct answer: d) Parkinsonism
Explanation:
- Correct (d): Parkinsonism refers to a group of disorders, including Parkinson’s disease, where bradykinesia (slowness of movement) and rigidity are hallmark features. These motor symptoms are due to degeneration of the dopaminergic neurons in the substantia nigra(13 Disorders of Motor C…).
- Incorrect (a): Huntington’s disease is primarily associated with chorea (involuntary, jerky movements) and cognitive decline, rather than bradykinesia and rigidity.
- Incorrect (b): Amyotrophic lateral sclerosis (ALS) leads to progressive muscle weakness and atrophy due to motor neuron degeneration but does not cause bradykinesia or rigidity.
- Incorrect (c): Progressive supranuclear palsy (PSP) can cause bradykinesia and rigidity but also presents with significant eye movement abnormalities and postural instability, making it distinct from classic Parkinsonism.
- Incorrect (e): Corticobasal degeneration also presents with movement issues, including rigidity, but it tends to involve asymmetric motor symptoms and apraxia, which distinguishes it from typical Parkinsonism.
