
Respiratory
Question 1:
Which of the following cells is primarily responsible for secreting surfactant in the alveoli?
a) Type I alveolar cells
b) Type II alveolar cells
c) Alveolar macrophages
d) Ciliated columnar cells
e) Smooth muscle cells
Answer: b) Type II alveolar cells
Explanation: Type II alveolar cells, also known as surfactant-producing cells or type II pneumocytes , are responsible for secreting surfactant, which reduces surface tension in the alveoli, preventing their collapse.
a) Type I alveolar cells: Incorrect. These cells line the alveoli and are involved in gas exchange, not surfactant production.
c) Alveolar macrophages: Incorrect. These cells function in immune defence by removing pathogens and debris from the alveoli, not surfactant production.
d) Ciliated columnar cells: Incorrect. These cells are part of the respiratory epithelium in the airways and are involved in moving mucus, not in surfactant secretion.
e) Smooth muscle cells: Incorrect. These cells help control airway diameter and airflow but do not produce surfactant.
Question 2:
Which of the following best describes the role of erythropoietin in the respiratory system?
a) It controls the rate of breathing.
b) It stimulates the production of red blood cells in response to hypoxia
c) It stimulates the production of RBC in response to high blood O2 levels
d) It produces sounds for speech.
e) It helps humidify inhaled air.
Answer: b) It stimulates the production of red blood cells in response to low oxygen levels.
Explanation: Erythropoietin is a hormone produced by the kidneys in response to low oxygen levels/Hypoxia in the blood. It stimulates the production of red blood cells to increase oxygen-carrying capacity.
a) It controls the rate of breathing: Incorrect. Breathing rate is primarily regulated by the brainstem in response to CO2 and O2 levels, not by erythropoietin.
c) It stimulates the production of RBC in response to high blood O2 levels: Incorrect. Erythropoietin is released in response to low oxygen levels (hypoxia), not high oxygen levels.
d) It produces sounds for speech: Incorrect. Sound production is primarily a function of the larynx and vocal cords, not erythropoietin.
e) It helps humidify inhaled air: Incorrect. Humidification of air occurs in the nasal cavity and upper respiratory tract, not via erythropoietin.
Question 3:
Which respiratory condition is characterized by the permanent enlargement and destruction of air sacs in the lungs, leading to decreased elastic recoil?
a) Asthma
b) Pneumonia
c) Emphysema
d) Bronchitis
e) Tuberculosis
Answer: c) Emphysema
Explanation: Emphysema is a chronic lung disease in which the air sacs (alveoli) in the lungs become damaged and lose their elasticity, making it difficult to exhale.
a) Asthma: Incorrect. Asthma is characterized by reversible bronchi and bronchioles narrowing and inflammation, not permanent destruction of air sacs.
b) Pneumonia: Incorrect. Pneumonia is an infection of the lungs that leads to inflammation and fluid accumulation, not destruction of air sacs.
d) Bronchitis: Incorrect. Chronic bronchitis involves inflammation and mucus production in the airways, but it does not destroy the air sacs in the lungs.
e) Tuberculosis: Incorrect. Tuberculosis is a bacterial infection that causes granulomas (a bunch of macrophages clumped together in response to inflammation or infection) in the lungs, but it is not characterized by the permanent enlargement of air sacs.
Question 4:
In pulmonary circulation, oxygenated blood is transported from the lungs to the heart through which vessel?
a) Pulmonary artery
b) Pulmonary vein
c) Aorta
d) Superior vena cava
e) Inferior vena cava
Answer: b) Pulmonary vein
Explanation: Pulmonary veins carry oxygenated blood from the lungs back to the heart to be pumped into the systemic circulation.
a) Pulmonary artery: Incorrect. The pulmonary artery carries deoxygenated blood from the heart to the lungs for oxygenation.
c) Aorta: Incorrect. The aorta carries oxygenated blood from the heart to the rest of the body, not from the lungs to the heart.
d) Superior vena cava: Incorrect. The superior vena cava carries deoxygenated blood from the upper body to the heart, not oxygenated blood from the lungs.
e) Inferior vena cava: Incorrect. The inferior vena cava carries deoxygenated blood from the lower body to the heart, not oxygenated blood from the lungs.
Question 5:
Which of the following is the primary stimulus for increasing the rate and depth of breathing during exercise?
a) Increased carbon dioxide (CO2) levels
b) Decreased oxygen (O2) levels
c) Increased oxygen (O2) levels
d) Increased stretch of the lungs
e) increased blood PH
Answer: a) Increased carbon dioxide (CO2) levels
Explanation: During exercise, increased metabolic activity leads to higher CO2 production. This will be detected by both the peripheral chemoreceptors in the aortic arch and carotid artery but also the central chemoreceptors in the brainstem and medulla . This increase in CO2 levels in the blood will lead to a decrease in PH and is the primary stimulus for increasing the rate and depth of breathing, allowing for efficient removal of CO2 and increased O2 intake.
b) Decreased oxygen (O2) levels: Incorrect. Oxygen levels do affect breathing, but CO2 levels are the more immediate trigger during exercise.
c) Increased oxygen (O2) levels: Incorrect. Increased oxygen does not stimulate an increase in breathing rate; the body adjusts breathing based on CO2 levels.
d) Increased stretch of the lungs: Incorrect. Stretch receptors in the bronchi help regulate breathing, but they are not the primary stimulus during exercise.
e) Increased blood pH: Incorrect. A rise in blood pH (alkalosis) would actually decrease the drive to breathe. During exercise, a decrease in blood pH occurs due to CO2 buildup due to an increased cellular respiration.
Question 6:
Which of the following lung volumes represents the maximum amount of air a person can exhale forcefully after taking the deepest possible breath?
a) Tidal volume
b) Inspiratory reserve volume
c) Expiratory reserve volume
d) Residual volume
e) Vital capacity
Answer: e) Vital capacity
Explanation: Vital capacity is the maximum amount of air a person can exhale forcefully after taking the deepest possible breath. It includes the inspiratory reserve volume, tidal volume, and expiratory reserve volume.
a) Tidal volume: Incorrect. Tidal volume is the amount of air inhaled or exhaled during normal breathing, not the maximum exhalation after a deep breath.
b) Inspiratory reserve volume: Incorrect. This is the additional air inhaled beyond a normal breath, not the maximum exhaled air.
c) Expiratory reserve volume: Incorrect. This is the extra air exhaled after a normal exhalation, but it does not represent the maximum exhalation.
d) Residual volume: Incorrect. This is the amount of air that remains in the lungs after maximal exhalation, not the air that can be exhaled.
Question 7:
Which component of the respiratory system is responsible for filtering, humidifying, and warming inspired air?
a) Alveoli
b) Trachea
c) Pharynx
d) Nasal cavity
e) Larynx
Answer: d) Nasal cavity
Explanation: The nasal cavity is equipped with structures like conchae and goblet cells, which help filter, humidify, and warm inspired air, preparing it for entry into the lungs.
a) Alveoli: Incorrect. Alveoli are the site of gas exchange, not air filtration, humidification, or warming.
b) Trachea: Incorrect. The trachea conducts air to the lungs but does not perform significant filtering or humidification.
c) Pharynx: Incorrect. The pharynx acts as a passageway for air and food but does not primarily filter, humidify, or warm air.
e) Larynx: Incorrect. The larynx is involved in voice production and protecting the airway during swallowing but is not primarily responsible for filtering or warming air.
Question 8:
What is the primary function of surfactant in the alveoli?
a) To decrease surface tension and prevent alveolar collapse
b) To trap inhaled particles and pathogens
c) To provide nutrients to alveolar cells
d) To increase surface tension and prevent alveolar collapse during exhalation
e) To protect against lung infections
Answer: a) To decrease surface tension and prevent alveolar collapse
Explanation: Surfactant is a substance produced by type II alveolar cells that reduces surface tension in the alveoli, preventing them from collapsing during exhalation. This ensures efficient gas exchange.
b) To trap inhaled particles and pathogens: Incorrect. This function is performed by mucus and cilia in the airways, not surfactant.
c) To provide nutrients to alveolar cells: Incorrect. Surfactant does not provide nutrients; its role is related to reducing surface tension.
d) To increase surface tension and prevent alveolar collapse during exhalation: Incorrect. Surfactant actually decreases surface tension, not increases it, to prevent alveolar collapse.
e) To protect against lung infections: Incorrect. While surfactant does have some immune properties, its primary function is not infection protection.
Question 9:
Which of the following conditions results from an autosomal recessive genetic mutation affecting chloride channels in the respiratory and digestive systems?
a) Asthma
b) Emphysema
c) Cystic fibrosis
d) Tuberculosis
e) Pneumonia
Answer: c) Cystic fibrosis
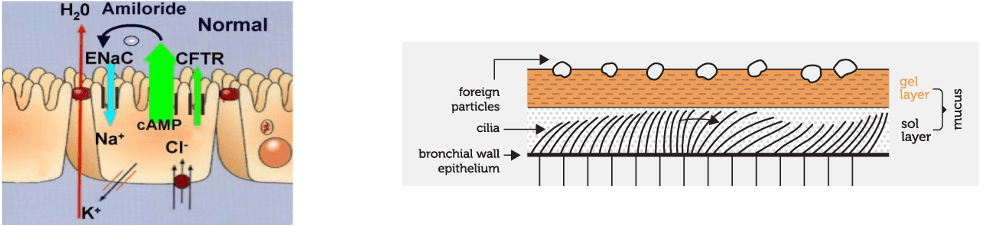
Explanation: Cystic fibrosis is an autosomal recessive disorder caused by mutations in the CFTR gene. This mutation causes a Mutated CFTR channel = NO downregulation of ENaC and Cl- ions cannot be pumped into ASL to attract water, as a result the Enac continually moves Na+ and water out of ASL uninhibited –> this creates thick, stagnant mucus found in the respiratory and digestive tract which can house pathogens in an ideal reproductive environment → This means Cilia cannot reach top of sol layer 🡪 also cannot move efficiently inside the thick mucous.This viscous mucus can obstruct airways, increase susceptibility to infections, and impair digestion, causing a range of symptoms and complications. A common disease in cystic fibrosis is pseudomonas aeruginosa (gram negative).
a) Asthma: Incorrect. Asthma is a chronic inflammatory condition that affects the airways but is not caused by a genetic mutation in chloride channels.
b) Emphysema: Incorrect. Emphysema is primarily caused by smoking and environmental factors, not a genetic mutation in chloride channels.
d) Tuberculosis: Incorrect. Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis, not a genetic mutation in chloride channels.
e) Pneumonia: Incorrect. Pneumonia is an infection of the lungs and is not related to genetic mutations affecting chloride channels.
Question 10:
Which lung volume always remains in the lungs, preventing lung collapse even after maximal exhalation?
a) Tidal volume
b) functional residual capacity
c) Expiratory reserve volume
d) Residual volume
e) Vital capacity
Answer: d) Residual volume
Explanation: The functional residual volume is the air that remains in the lungs after maximal exhalation. It ensures that the alveoli stay open and prevents lung collapse.
a) Tidal volume: Incorrect. Tidal volume is the amount of air exchanged during normal breathing. It does not remain in the lungs after maximal exhalation.
b) Functional residual capacity: Incorrect. This volume includes the air remaining after normal exhalation (residual volume plus expiratory reserve volume), but not all of it remains after maximal exhalation.
c) Expiratory reserve volume: Incorrect. This is the extra air that can be exhaled after a normal exhalation, but it can be fully exhaled, leaving no air in the lungs.
e) Vital capacity: Incorrect. Vital capacity is the total amount of air that can be exhaled after a maximal inhalation, but it does not account for the air that remains in the lungs.
Question 11:
What is the primary function of the pleural membranes surrounding the lungs?
a) Facilitating gas exchange
b) Providing protection against infections
c) Reducing friction during breathing
d) Secreting mucus for airway lubrication
e) Producing surfactant for lung expansion
Answer: c) Reducing friction during breathing
Explanation: The pleural membranes create a fluid-filled cavity that reduces friction between the lungs and chest wall during breathing, allowing for smooth respiratory movements.
a) Facilitating gas exchange: Incorrect. Gas exchange occurs in the alveoli, not in the pleural membranes.
b) Providing protection against infections: Incorrect. The pleural membranes are not primarily involved in immune defense.
d) Secreting mucus for airway lubrication: Incorrect. Mucus is secreted by goblet cells in the respiratory tract, not by the pleural membranes.
e) Producing surfactant for lung expansion: Incorrect. Surfactant is produced by type II alveolar cells, not by the pleural membranes.
Question 12:
Which of the following hormones can dilate the bronchioles and increase respiratory rate?
a) DHEA
b) cortisol
c) Aldosterone
d) Epinephrine
e) Thyroxine
Answer: d) Epinephrine
Explanation: Epinephrine, released during the “fight or flight” response, can dilate bronchioles and increase respiratory rate to enhance oxygen supply during times of stress or danger.
a) DHEA: Incorrect. DHEA is involved in hormone production but does not have a direct effect on bronchioles or respiratory rate.
b) Cortisol: Incorrect. While Cortisol is a stress hormone its primary function is inflammation and metabolism, but it does not directly dilate bronchioles.
c) Aldosterone: Incorrect. Aldosterone regulates sodium and water balance in the kidneys but does not influence bronchiole dilation or respiratory rate.
e) Thyroxine: Incorrect. Thyroxine (T4) regulates metabolism but does not directly affect bronchiole dilation.
Question 13:
During exercise, what happens to the respiratory rate and tidal volume?
a) Respiratory rate increases, tidal volume decreases
b) Respiratory rate decreases, tidal volume increases
c) Respiratory rate and tidal volume both increase
d) Respiratory rate and tidal volume both decrease
e) Respiratory rate remains unchanged, but tidal volume increases
Answer: c) Respiratory rate and tidal volume both increase
Explanation: During exercise, the body requires more oxygen to meet increased metabolic demands whilst getting rid of the increased Blood Co2 levels. To achieve this, both the respiratory rate (breaths per minute) and tidal volume (volume of air per breath) increase to deliver more oxygen to the tissues.
a) Respiratory rate increases, tidal volume decreases: Incorrect. Both respiratory rate and tidal volume increase during exercise to meet the increased oxygen demand.
b) Respiratory rate decreases, tidal volume increases: Incorrect. Respiratory rate does not decrease during exercise; it increases alongside tidal volume.
d) Respiratory rate and tidal volume both decrease: Incorrect. Both respiratory rate and tidal volume increase during exercise to improve oxygen delivery and carbon dioxide removal.
e) Respiratory rate remains unchanged, but tidal volume increases: Incorrect. Both respiratory rate and tidal volume increase during exercise, not just one to allow for increased Blood O2 levels and decreased CO2 levels.
Question 14:
Which specific part of the brain is primarily responsible for the automatic control of respiration, including basic rhythm and rate?
a) Cerebellum
b) Thalamus
c) Medulla oblongata
d) Pons
e) Hypothalamus
Answer: c) Medulla oblongata
Explanation: The medulla oblongata, located in the brainstem, is responsible for the automatic control of respiration. It regulates the basic rhythm and rate of breathing by monitoring blood gas levels and adjusting ventilation accordingly.
a) Cerebellum: Incorrect. The cerebellum coordinates motor control and balance, not respiration.
b) Thalamus: Incorrect. The thalamus processes sensory information but is not involved in respiratory control.
d) Pons: Incorrect. The pons assists with the smooth transition and more of the fine tuning between inhalation and exhalation but is not primarily responsible for rhythm and rate.
e) Hypothalamus: Incorrect. The hypothalamus regulates various autonomic functions, but respiration is controlled mainly by the brainstem.
Question 15:
In the context of respiratory control, what is the primary function of central chemoreceptors?
a) Detect changes in arterial oxygen levels
b) Monitor lung compliance
c) Respond to changes in arterial carbon dioxide levels
d) Regulate surfactant production
e) Control the rate of heart contractions
Answer: c) Respond to changes in arterial carbon dioxide levels
Explanation: Central chemoreceptors, primarily located in the medulla oblongata, play a vital role in regulating ventilation. They are highly sensitive to changes in arterial carbon dioxide (CO2) levels, triggering adjustments in respiratory rate to maintain appropriate CO2 and pH levels in the blood.
a) Detects changes in arterial oxygen levels: Incorrect. Peripheral chemoreceptors (in the carotid and aortic bodies) detect changes in oxygen levels, not central chemoreceptors.
b) Monitor lung compliance: Incorrect. Lung compliance is monitored by stretch receptors in the bronchi of lungs, not by central chemoreceptors.
d) Regulate surfactant production: Incorrect. Surfactant production is regulated by type II alveolar cells, not chemoreceptors.
e) Control the rate of heart contractions: Incorrect. Heart rate is regulated by the autonomic nervous system and not by central chemoreceptors.
Question 16:
What is the primary role of the mucociliary escalator in lung defence?
a) Trapping and removing inhaled pathogens and particles
b) Mucus secretion to protect the lining from chemicals
c) Cilia cells push air towards the alveoli
d) Producing surfactant for alveolar stability
e) Transmitting neural signals for breathing control
Answer: a) Trapping and removing inhaled pathogens and particles
Explanation: The mucociliary escalator consists of mucus-producing cells – pseudostratified columnar cells and cilia lining the airways. Its primary role is to trap and remove inhaled pathogens, dust, and particles by moving them upward toward the throat, where they can be swallowed or expelled.
b) Mucus secretion to protect the lining from chemicals: Incorrect. Although mucus protects the respiratory lining, the primary function of the mucociliary escalator is to trap and move debris.
c) Cilia cells push air towards the alveoli: Incorrect. The cilia move mucus upward, not air downward, toward the throat for expulsion.
d) Producing surfactant for alveolar stability: Incorrect. Surfactant production occurs in the alveoli, and it is unrelated to the mucociliary escalator.
e) Transmitting neural signals for breathing control: Incorrect. Neural control of breathing occurs in the brainstem, not through the mucociliary escalator.
Question 17:
In terms of lung defence, what is the role of immunoglobulin IgE?
a) Promotion of mucus production
b) Activation of macrophages
c) Inhibition of inflammation
d) Antagonism of IgA
e) Allergic responses and defence against parasites
Answer: e) Allergic responses and defence against parasites
Explanation: Immunoglobulin IgE is primarily associated with allergic responses and defence against parasites. It triggers the release of histamine and other chemicals in response to allergens or parasitic infections, leading to allergic reactions and immune defence.
a) Promotion of mucus production: Incorrect. IgE does not promote mucus production directly; this is typically stimulated by other immune responses and inflammation.
b) Activation of macrophages: Incorrect. IgE is involved in allergic responses and defence against parasites, not in directly activating macrophages.
c) Inhibition of inflammation: Incorrect. IgE actually promotes inflammation during allergic responses rather than inhibiting it.
d) Antagonism of IgA: Incorrect. IgE does not antagonise IgA; these immunoglobulins serve different immune functions.
Question 18:
In the context of respiratory physiology, explain how the Haldane effect influences the exchange of carbon dioxide in the blood.
a) The Haldane effect enhances carbon dioxide binding to haemoglobin in systemic capillaries.
b) The Haldane effect promotes carbon dioxide unloading from haemoglobin in pulmonary capillaries.
c) The Haldane effect reduces carbon dioxide transport in venous blood.
d) The Haldane effect increases carbon dioxide solubility in arterial blood.
e) The Haldane effect decreases carbon dioxide production in tissues.
Answer: b) The Haldane effect promotes carbon dioxide unloading from haemoglobin in pulmonary capillaries.
Explanation: The Haldane effect describes how oxygenation of blood in the lungs promotes the unloading of carbon dioxide from haemoglobin, facilitating CO2 removal.
a) The Haldane effect enhances carbon dioxide binding to haemoglobin in systemic capillaries: Incorrect. The Haldane effect is primarily concerned with the unloading of carbon dioxide, not its binding in systemic capillaries.
c) The Haldane effect reduces carbon dioxide transport in venous blood: Incorrect. The Haldane effect facilitates the unloading of CO2, but it does not reduce its transport in venous blood.
d) The Haldane effect increases carbon dioxide solubility in arterial blood: Incorrect. The Haldane effect influences CO2 unloading, not its solubility in arterial blood.
e) The Haldane effect decreases carbon dioxide production in tissues: Incorrect. The Haldane effect has no direct role in carbon dioxide production; it affects how CO2 is released from haemoglobin.
Question 19:
Which immunoglobulin plays a significant role in lung defence by binding to airborne pathogens in mucosa?
a) IgA
b) IgE
c) IgG
d) IgM
e) IgD
Answer: a) IgA
Explanation: Immunoglobulin A (IgA) is the primary antibody involved in mucosal immunity or any type of secretions e.g. in tears, including the respiratory mucosa. It plays a crucial role in binding to and neutralizing airborne pathogens.
b) IgE: Incorrect. IgE is primarily involved in allergic reactions and defence against parasitic infections, not mucosal immunity.
c) IgG: Incorrect. IgG is the most abundant antibody in circulation and is important for systemic immunity, but it is not the main antibody in mucosal surfaces.
d) IgM: Incorrect. IgM is mainly involved in the primary immune response and is found in the bloodstream, not in mucosal surfaces.
e) IgD: Incorrect. IgD is found on the surface of B cells and plays a role in initiating immune responses, but it is not significant in mucosal immunity.
Question 20:
What is the role of the CFTR protein?
a) Prevents airway collapse
b) Inhibiting cough reflex
c) Regulating ciliary movement
d) Regulating mucus production
e) Supporting alveolar gas exchange
Answer: d) Regulates mucus production
Explanation: The CFTR (Cystic Fibrosis Transmembrane Conductance Regulator) protein is responsible for regulating chloride transport in epithelial cells. It helps to downregulate the Enac channel causing less sodium to be pumped into the epithelial cell at the same time it allows for chloride ions to be pumped into the ASL layer to attract more water . When CFTR is dysfunctional (as in cystic fibrosis), it leads to the accumulation of thick, sticky mucus in the airways, impairing mucus clearance.
a) Prevents airway collapse: Incorrect. Airway collapse is more related to structural issues and smooth muscle tone, not CFTR function.
b) Inhibiting cough reflex: Incorrect. The cough reflex is a neural response, not directly related to CFTR protein function.
c) Regulating ciliary movement: Incorrect. While CFTR indirectly influences cilia function by affecting mucus consistency, its primary role is in ion transport and mucus regulation.
e) Supporting alveolar gas exchange: Incorrect. Gas exchange occurs in the alveoli and is unrelated to CFTR protein function, which is primarily involved in mucus and fluid regulation.
Question 21:
Which cells play a role in host defence in the respiratory system by phagocytosing pathogens and cellular debris?
a) T cells
b) B cells
c) Macrophages
d) Eosinophils
e) Mast cells
Answer: c) Macrophages
Explanation: Macrophages are immune cells found in the respiratory system that engulf and digest pathogens, cellular debris, and foreign particles, contributing to host defence.
a) T cells: Incorrect. T cells are involved in adaptive immunity, including targeting infected cells, but they do not phagocytose pathogens.
b) B cells: Incorrect. B cells produce antibodies, but they do not engage in phagocytosis.
d) Eosinophils: Incorrect. Eosinophils are involved in combating parasitic infections and allergic reactions, but they do not play a primary role in phagocytosis.
e) Mast cells: Incorrect. Mast cells release histamine and other mediators during allergic responses, but they do not perform phagocytosis.
Question 22:
Which type of vaccination exposes an individual to an inactivated or weakened pathogen to stimulate an immune response?
a) Passive Vaccination
b) Active Vaccination
c) DNA Vaccination
d) mRNA Vaccination
e) Subunit Vaccination
Answer: b) Active Vaccination
Explanation: Active vaccination involves administering a weakened or inactivated pathogen to stimulate the individual’s immune system to produce an immune response and memory cells against the pathogen.
a) Passive Vaccination: Incorrect. Passive vaccination involves the transfer of pre-formed antibodies, not exposure to a pathogen.
c) DNA Vaccination: Incorrect. DNA vaccines introduce genetic material coding for an antigen rather than a whole pathogen.
d) mRNA Vaccination: Incorrect. mRNA vaccines introduce messenger RNA that codes for a specific protein of the pathogen, not the whole pathogen.
e) Subunit Vaccination: Incorrect. Subunit vaccines use only specific parts of the pathogen, such as antigens, proteins or polysaccharides, rather than the whole pathogen.
Question 23:
Which nerves are responsible for the innervation of the diaphragm?
a) Phrenic nerves
b) Vagus nerves
c) Sympathetic nerves
d) Glossopharyngeal nerves
e) Recurrent laryngeal nerves
Answer: a) Phrenic nerves
Explanation: The diaphragm is primarily innervated by the phrenic nerves (C3-C5), which are responsible for controlling its contraction and initiating the process of breathing. (P.s tip C3-C5 keeps the diaphragm alive)
b) Vagus nerves: Incorrect. The vagus nerves primarily innervate organs like the heart, lungs, and digestive tract, but they do not innervate the diaphragm.
c) Sympathetic nerves: Incorrect. The sympathetic nerves are involved in the autonomic nervous system and do not directly innervate the diaphragm.
d) Glossopharyngeal nerves: Incorrect. The glossopharyngeal nerves are involved in taste sensation and the gag reflex, not diaphragm innervation.
e) Recurrent laryngeal nerves: Incorrect. The recurrent laryngeal nerves are branches of the vagus nerve that innervate the larynx, not the diaphragm.
Question 24: What is the approximate height of the Airway Surface Liquid (ASL) in the respiratory system?
a) 2 micrometres
b) 4 micrometres
c) 6 micrometres
d) 7 micrometres
e) 8 micrometres
Answer: d) 7 micrometres
Explanation: The Airway Surface Liquid (ASL) in the respiratory system has an approximate height of 7 micrometres. This thin layer of liquid is essential for maintaining proper mucociliary clearance and protecting the respiratory epithelium. The ASL layer is the same height as the cilia to allow effective beating and also to prevent the cilia from being squashed.
a) 2 micrometres: Incorrect. This height is too small to allow for effective mucociliary clearance.
b) 4 micrometres: Incorrect. While closer, 4 micrometres is still below the average ASL height.
c) 6 micrometres: Incorrect. This is slightly below the correct height of the ASL.
e) 8 micrometres: Incorrect. This height is slightly above the average ASL height, which is typically around 7 micrometres.
Question 25:
What is the primary function of goblet cells in the respiratory epithelium?
a) Secretion of surfactant
b) Production of mucus
c) Gas exchange
d) Immune cell activation
e) Ciliary movement
Answer: b) Production of mucus
Explanation: Goblet cells in the respiratory epithelium are specialized cells responsible for the production and secretion of mucus. This mucus helps trap and remove foreign particles, microbes, and debris from the airways, contributing to the protection and maintenance of the respiratory system.
a) Secretion of surfactant: Incorrect. Surfactant is produced by type II alveolar cells, not goblet cells.
c) Gas exchange: Incorrect. Gas exchange occurs in the alveoli and is not a function of goblet cells.
d) Immune cell activation: Incorrect. Goblet cells produce mucus but are not directly involved in immune cell activation.
e) Ciliary movement: Incorrect. Ciliary movement is facilitated by ciliated cells, not goblet cells.
Question 26:
What do peripheral chemoreceptors primarily detect in the bloodstream to regulate respiratory rate?
a) Oxygen concentration
b) Carbon dioxide concentration
c) pH level
d) Blood pressure
e) Haemoglobin levels
Answer: a) Oxygen concentration
Explanation: Peripheral chemoreceptors, such as the carotid bodies and aortic bodies, primarily detect changes in the concentration of oxygen (O2) in the bloodstream. When oxygen levels decrease (hypoxia), they send signals to increase respiratory rate, helping to improve oxygen delivery to tissues. While they also respond to changes in carbon dioxide (CO2) and pH levels, their main role is monitoring oxygen levels.
b) Carbon dioxide concentration: Incorrect. While carbon dioxide levels are primarily detected by central chemoreceptors in the brainstem, peripheral chemoreceptors respond mainly to low oxygen levels.
c) pH level: Incorrect. Although peripheral chemoreceptors can respond to changes in pH, their primary role is in detecting oxygen concentration.
d) Blood pressure: Incorrect. Baroreceptors, not chemoreceptors, are responsible for detecting changes in blood pressure.
e) Haemoglobin levels: Incorrect. Haemoglobin levels are monitored by different mechanisms in the body, not by peripheral chemoreceptors.
Question 27:
Which of the following statements about 2,3-diphosphoglycerate (2,3-DPG) is correct?
a) 2,3-DPG increases haemoglobin’s affinity for oxygen
b) 2,3-DPG decreases haemoglobin’s affinity for oxygen
c) 2,3-DPG is primarily produced in the lungs
d) 2,3-DPG enhances the binding of carbon monoxide to haemoglobin
e) 2,3-DPG is involved in the transport of carbon dioxide in the blood
Answer: b) 2,3-DPG decreases haemoglobin’s affinity for oxygen
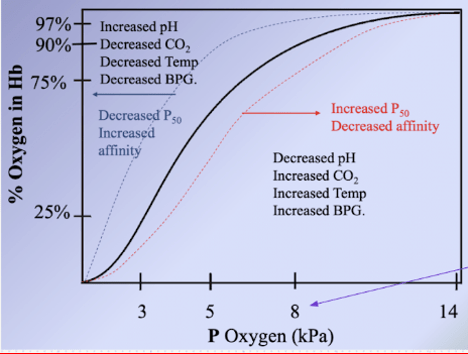
Explanation: 2,3-DPG is a molecule found in red blood cells that decreases haemoglobin’s affinity for oxygen. This allows haemoglobin to release oxygen more readily in peripheral tissues where oxygen levels are lower e.g. in exercise. (p.s. you can remember what causes haemoglobin to readily dissociate O2 by the Mnemonic ‘CADET FACE RIGHT’ C: Carbon dioxide (increased), A: acidosis (low Ph), D:2,3-DPG, E: exercise, T: temperature(increased) and ‘face right – referees to the haemoglobin curve shifting to the right meaning Haemaglobin dissacoiates O2 more readily)
a) 2,3-DPG increases haemoglobin’s affinity for oxygen: Incorrect. This is the opposite 2,3-DPG reduces haemoglobin’s affinity for oxygen, promoting oxygen release to tissues.
c) 2,3-DPG is primarily produced in the lungs: Incorrect. 2,3-DPG is primarily produced in red blood cells, not in the lungs.
d) 2,3-DPG enhances the binding of carbon monoxide to haemoglobin: Incorrect. Carbon monoxide binds to haemoglobin with high affinity, and 2,3-DPG does not enhance this binding.
e) 2,3-DPG is involved in the transport of carbon dioxide in the blood: Incorrect. Carbon dioxide is primarily transported as bicarbonate in the blood, and 2,3-DPG does not play a role in this process.
Question 28:
What distinguishes the left recurrent laryngeal nerve from the right recurrent laryngeal nerve in terms of its anatomical course?
a) The left recurrent laryngeal nerve loops around the aorta
b) The left recurrent laryngeal nerve is longer than the right recurrent laryngeal nerve
c) The left recurrent laryngeal nerve innervates different muscles than the right recurrent laryngeal nerve
d) The left recurrent laryngeal nerve is not involved in vocal cord movement
e) The left recurrent laryngeal nerve is not a branch of the vagus nerve
Answer: a) The left recurrent laryngeal nerve loops around the aorta
Explanation: The left recurrent laryngeal nerve takes a longer course than the right recurrent laryngeal nerve because it loops under the aortic arch on its way to innervate the muscles of the larynx. This anatomical distinction is important in clinical contexts, such as during certain surgical procedures, as it makes the left recurrent laryngeal nerve more susceptible to injury.
b) The left recurrent laryngeal nerve is longer than the right recurrent laryngeal nerve: Incorrect. While the left recurrent laryngeal nerve does take a longer course, the key distinction is that it loops around the aorta.
c) The left recurrent laryngeal nerve innervates different muscles than the right recurrent laryngeal nerve: Incorrect. Both the left and right recurrent laryngeal nerves innervate the intrinsic muscles of the larynx apart from the cricothyroid muscle.
d) The left recurrent laryngeal nerve is not involved in vocal cord movement: Incorrect. The left recurrent laryngeal nerve plays an essential role in controlling the vocal cords.
e) The left recurrent laryngeal nerve is not a branch of the vagus nerve: Incorrect. Both the left and right recurrent laryngeal nerves are branches of the vagus nerve.
Question 29:
Which of the following muscles primarily functions as an expiratory muscle?
a) Diaphragm
b) Rectus abdominis
c) Sternocleidomastoid
d) Scalene muscles
e) Pectoralis minor
Answer: b) Rectus abdominis
Explanation: The rectus abdominis muscle is one of the primary forced expiratory muscles (the abdominal muscles but also the internal intercostal muscles as well) . It contracts during forced expiration, helping to increase intra-abdominal pressure, which assists in pushing air out of the lungs. The diaphragm, on the other hand, is a primary muscle of inspiration, while the other muscles listed have different functions in respiration.
a) Diaphragm: Incorrect. The diaphragm is used for both inhalation (contracting and flattening) and exhalation (relaxing and doming up)
c) Sternocleidomastoid: Incorrect. The sternocleidomastoid muscle assists with forced inspiration by helping to lift the rib cage.
d) Scalene muscles: Incorrect. The scalene muscles also assist with forced inspiration by elevating the first two ribs.
e) Pectoralis minor: Incorrect. The pectoralis minor muscle assists with forced inspiration by lifting the ribs, not expiration.
Question 30:
Which part of the brain is responsible for fine-tuning and controlling the depth and rate of breathing, thereby influencing the inspiratory and expiratory rhythm generated by the medullary respiratory centres?
a) Ventral Respiratory Group (VRG)
b) Dorsal Respiratory Group (DRG)
c) Pneumotaxic Centre
d) Apneustic Centre
e) Hypothalamus
Answer: c) Pneumotaxic Centre
Explanation: The Pneumotaxic Centre, located in the upper pons of the brainstem, plays a crucial role in controlling the rate and depth of breathing by fine-tuning the output of the medullary respiratory centres, helping to regulate the inspiratory and expiratory rhythm. It works by inhibiting the apneustic centre creating more shallower breaths.
a) Ventral Respiratory Group (VRG): Incorrect. The VRG primarily regulates the rhythm of breathing, particularly forced expiration, but does not fine-tune the depth and rate of breathing.
b) Dorsal Respiratory Group (DRG): Incorrect. The DRG is primarily responsible for initiating inspiration but does not regulate the depth and rate of breathing.
d) Apneustic Centre: Incorrect. The apneustic centre promotes deep, prolonged inspiration, but it is counterbalanced by the pneumotaxic centre.
e) Hypothalamus: Incorrect. The hypothalamus regulates various autonomic functions but is not directly involved in controlling breathing rhythm.
Question 31:
What is the primary role of the Dorsal Respiratory Group (DRG) in the respiratory control centre?
a) Initiating inspiration
b) Initiating expiration
c) Regulating blood pH
d) Modulating cough reflex
e) Controlling voluntary breathing
Answer: a) Initiating inspiration
Explanation: The Dorsal Respiratory Group (DRG) is responsible for initiating the inspiratory phase of breathing by sending signals to the diaphragm and external intercostal muscles.
b) Initiating expiration: Incorrect. Expiration is typically passive and regulated by the ventral respiratory group (VRG) during forced breathing.
c) Regulating blood pH: Incorrect. While breathing indirectly affects blood pH, the DRG’s main role is initiating inspiration, not pH regulation.
d) Modulating cough reflex: Incorrect. The cough reflex is mediated by other neural pathways, not the DRG.
e) Controlling voluntary breathing: Incorrect. Voluntary control of breathing involves the cerebral cortex, not the DRG.
Question 32:
The Hering-Breuer reflex is a protective mechanism in the respiratory system that prevents overinflation of the lungs. Which receptors are primarily responsible for initiating this reflex?
a) J receptors
b) Carotid bodies chemoreceptors
c) Central chemoreceptors in medulla oblongata
d) Baroreceptors
e) Stretch receptors in the bronchi and bronchioles
Answer: e) Stretch receptors in the bronchi and bronchioles
Explanation: The Hering-Breuer reflex is triggered by stretch receptors located in the walls of the bronchi and bronchioles. These receptors sense lung inflation and send signals to the respiratory centres in the brainstem to inhibit further inhalation, preventing overinflation of the lungs during inspiration.
a) J receptors: Incorrect. J receptors respond to pulmonary capillary engorgement and are associated with the sensation of dyspnea, not the Hering-Breuer reflex.
b) Carotid bodies chemoreceptors: Incorrect. These chemoreceptors detect changes in blood oxygen levels and are involved in respiratory rate regulation, not lung inflation.
c) Central chemoreceptors in medulla oblongata: Incorrect. These chemoreceptors respond to changes in CO2 and pH, not lung inflation.
d) Baroreceptors: Incorrect. Baroreceptors detect changes in blood pressure, not lung inflation.
Question 33:
What is the key difference between a shunt and physiologic dead space in the respiratory system?
a) Shunt involves areas with poor ventilation and good perfusion, while physiologic dead space involves areas with good ventilation and poor perfusion.
b) Shunt involves areas with good ventilation and poor perfusion, while physiologic dead space involves areas with good ventilation and poor perfusion.
c) Shunt and physiologic dead space are essentially the same, involving areas with good ventilation and poor perfusion.
d) Shunt and physiologic dead space are essentially the same, involving areas with poor ventilation and poor perfusion.
e) Shunt involves areas with no ventilation and no perfusion, while physiologic dead space involves areas with good ventilation and good perfusion.
Answer: a) Shunt involves areas with poor ventilation and good perfusion, while physiologic dead space involves areas with good ventilation and poor perfusion.
Explanation: A shunt occurs when there is poor ventilation (air exchange) but good perfusion (blood flow) in certain lung regions, leading to wasted oxygen. In contrast, physiologic dead space involves areas with good ventilation but poor perfusion, resulting in inefficient removal of carbon dioxide. These are distinct concepts in respiratory physiology.
b) Shunt involves areas with good ventilation and poor perfusion: Incorrect. This describes physiologic dead space, not a shunt.
c) Shunt and physiologic dead space are essentially the same, involving areas with good ventilation and poor perfusion: Incorrect. Shunt and physiologic dead space are different physiological concepts.
d) Shunt and physiologic dead space are essentially the same, involving areas with poor ventilation and poor perfusion: Incorrect. A shunt involves poor ventilation with good perfusion, while physiologic dead space involves good ventilation with poor perfusion.
e) Shunt involves areas with no ventilation and no perfusion, while physiologic dead space involves areas with good ventilation and good perfusion: Incorrect. This is not an accurate description of either a shunt or physiologic dead space.

Question 34:
What is the primary mechanism behind hypoxic pulmonary vasoconstriction (HPV)?
a) Increased nitric oxide production leading to vasodilation for increased blood flow.
b) Activation of sympathetic nerves causing pulmonary arteriole constriction.
c) Elevated pH in response to hypoxia resulting in vasoconstriction to expire CO2.
d) Release of histamine causing relaxation of pulmonary arterioles to allow for increased blood flop.
e) Hypoxia-induced vasoconstriction causing pulmonary arteriole constriction and diverting blood flow to better ventilated alveoli.
Answer: e) Hypoxia-induced vasoconstriction causing pulmonary arteriole constriction and diverting blood flow to better ventilated alveoli
Explanation: Hypoxic pulmonary vasoconstriction (HPV) is primarily driven by the release of endothelin-1, which leads to the constriction of pulmonary arterioles in response to low oxygen levels. This redirection of blood flow optimizes oxygen exchange in the lungs.
a) Increased nitric oxide production leading to vasodilation for increased blood flow: Incorrect. Nitric oxide typically causes vasodilation, which is the opposite of what occurs in hypoxic pulmonary vasoconstriction. HPV involves constriction, not dilation, of the pulmonary arterioles.
b) Activation of sympathetic nerves causing pulmonary arteriole constriction: Incorrect. HPV is a local response to hypoxia within the lungs and is not mediated by the sympathetic nervous system, which primarily affects systemic circulation, not pulmonary circulation.
c) Elevated pH in response to hypoxia resulting in vasoconstriction to expire CO2: Incorrect. HPV is not directly related to pH changes or CO2 expiration. It is a response to low oxygen levels (hypoxia) rather than pH alterations.
d) Release of histamine causing relaxation of pulmonary arterioles to allow for increased blood flow: Incorrect. Histamine typically causes vasodilation and increased permeability in inflammatory responses, not vasoconstriction in response to hypoxia.
Question 35:
Which cell type best describes type 2 pneumocytes in the alveoli?
a) Squamous
b) Cuboidal
c) Columnar
d) Ciliated
e) Brush border
Answer: b) Cuboidal
Explanation: Type 2 pneumocytes are typically cuboidal in shape and are responsible for producing and secreting pulmonary surfactant, which reduces surface tension in the alveoli and helps prevent their collapse.
a) Squamous: Incorrect. Squamous cells are flat and thin, such as type 1 pneumocytes, which cover a large surface area for gas exchange, not type 2 pneumocytes.
c) Columnar: Incorrect. Columnar cells are typically taller and found in the respiratory tract lining (pseudostratified columnar cells) but are not characteristic of type 2 pneumocytes.
d) Ciliated: Incorrect. Ciliated cells are involved in moving mucus and debris out of the respiratory tract, not in surfactant production within the alveoli.
e) Brush border: Incorrect. Brush border cells are typically associated with absorption, such as in the intestines, and are not found in the alveoli.
Question 36:
From which spinal levels do the phrenic nerves originate?
a) C3 to C5
b) C6 to C8
c) T1 to T3
d) L1 to L3
e) S1 to S3
Answer: a) C3 to C5
Explanation: The phrenic nerves originate from the spinal cord levels C3 to C5 and play a crucial role in controlling the diaphragm, the primary muscle of respiration. (c3-C5 keeps the diaphragm alive)
b) C6 to C8: Incorrect. These levels correspond to nerves that innervate the upper limbs, not the diaphragm.
c) T1 to T3: Incorrect. These spinal levels are involved in innervating muscles and skin of the thorax and upper limbs, not the diaphragm.
d) L1 to L3: Incorrect. These spinal levels innervate the lower back and parts of the legs, not the diaphragm.
e) S1 to S3: Incorrect. These spinal levels innervate the lower limbs and pelvic organs, not the diaphragm.
Question 37:
Why is diving dangerous at significant depths?
A) Depletion of oxygen
B) Increased partial pressure of gases
C) Reduced buoyancy
D) Altered barometric pressure
E) Enhanced sunlight exposure
Answer: B) Increased partial pressure of gases
Explanation: Diving at significant depths leads to increased pressure, which results in higher partial pressures of gases, especially nitrogen and oxygen. This elevated pressure makes it easier for these gases to dissolve into bodily fluids and tissues, potentially leading to decompression sickness, also known as “the bends.” This condition can be hazardous and highlights the risks associated with deep-sea diving.
a) Depletion of oxygen: Incorrect. While oxygen is important, the primary danger at depth is not oxygen depletion but the effects of increased pressure on gas solubility.
c) Reduced buoyancy: Incorrect. Reduced buoyancy can affect divers’ ability to ascend and descend, but the primary danger at depth relates to gas pressure effects, not buoyancy alone.
d) Altered barometric pressure: Incorrect. While barometric pressure changes at depth, it is the resulting increased partial pressure of gases that poses a greater risk, not the pressure itself.
e) Enhanced sunlight exposure: Incorrect. Sunlight exposure decreases with depth, so this is not a relevant danger in deep-sea diving.
Question 38:
How does nitrogen toxicity primarily affect cells during deep-sea diving?
A) It disrupts cell membrane integrity
B) It reduces blood flow
C) It causes ischaemia
D) It stabilizes ion channels
E) It stimulates protein breakdown
Answer: A) It disrupts cell membrane integrity
Explanation: Nitrogen toxicity, which occurs at high partial pressures during deep-sea diving, can disrupt cell membrane integrity. The increased pressure causes nitrogen to dissolve in cell membranes, altering their structure and potentially affecting the normal function of ion channels and other membrane-bound proteins. This disruption in cell membrane integrity is one of the mechanisms behind the harmful effects of nitrogen narcosis and decompression sickness in divers.
b) It reduces blood flow: Incorrect. Nitrogen toxicity does not primarily reduce blood flow, although nitrogen bubbles can obstruct blood vessels during rapid ascent, leading to decompression sickness.
c) It causes ischemia: Incorrect. While nitrogen bubbles can cause ischemia, nitrogen toxicity specifically refers to the effect of nitrogen dissolving into cells and disrupting membrane function.
d) It stabilizes ion channels: Incorrect. Nitrogen toxicity destabilizes, rather than stabilizes, ion channels by affecting the cell membrane’s structure.
e) It stimulates protein breakdown: Incorrect. Nitrogen toxicity does not directly stimulate protein breakdown; its primary effect is on cell membranes.
Question 39:
Why is fast resurfacing avoided during deep-sea diving?
A) It promotes oxygen delivery to tissues
B) It reduces the risk of nitrogen narcosis
C) It prevents the formation of nitrogen bubbles
D) It minimizes the risk of decompression sickness
E) It would cause nitrogen bubbles in the bloodstream, potentially leading to ischemia
Answer: E) It would cause nitrogen bubbles in the bloodstream, potentially leading to ischemia
Explanation: as you resurface the pressure decreases therefore the volume of nitrogen in your body increases hence more nitrogen will be diffusing out of the tissuesin your body to your lungs. However, fast resurfacing during deep-sea diving is avoided because it can lead to the rapid release of dissolved nitrogen from tissues into the bloodstream. This sudden release of nitrogen can form bubbles in the blood, which can block blood vessels and lead to ischemia (lack of blood flow) in various tissues, causing serious health risks. It also can cause severe damage to the tissues which contain this gas due to the increased volume of gas as the diver resurfaces.
a) It promotes oxygen delivery to tissues: Incorrect. Fast resurfacing does not promote oxygen delivery; it increases the risk of nitrogen bubble formation, which can block oxygen delivery.
b) It reduces the risk of nitrogen narcosis: Incorrect. Slow resurfacing reduces the risk of decompression sickness, but nitrogen narcosis is more related to depth than resurfacing speed.
c) It prevents the formation of nitrogen bubbles: Incorrect. Fast resurfacing actually promotes nitrogen bubble formation, which is why it is avoided.
d) It minimizes the risk of decompression sickness: Incorrect. This statement is true, but it describes the effect of slow resurfacing, not fast resurfacing.
Question 40:
What is the primary purpose of the nasal conchae in the nasal cavity?
Options:
A) To produce mucus for lubrication
B) To detect olfactory stimuli
C) To enhance vocal resonance
D) To increase the surface area for air contact
E) To support the nasal septum
Answer: D) To increase the surface area for air contact
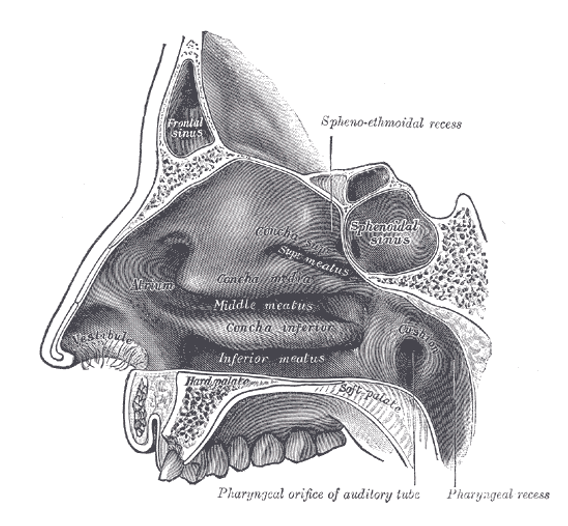
Explanation: The nasal conchae, or turbinates, are bony structures in the nasal cavity. Their main function is to increase the surface area inside the nasal cavity, which serves to warm, humidify, and filter inhaled air more effectively. This increased surface area allows for greater contact between the air and the nasal mucosa, improving the air conditioning process before it enters the lower respiratory system.
a) To produce mucus for lubrication: Incorrect. While the nasal cavity produces mucus, this is not the primary function of the nasal conchae.
b) To detect olfactory stimuli: Incorrect. Olfactory receptors in the nasal cavity detect smells, but this is not the function of the conchae, which serve to condition inhaled air.
c) To enhance vocal resonance: Incorrect. The nasal conchae do not significantly affect vocal resonance; their primary role is in air conditioning.
e) To support the nasal septum: Incorrect. The nasal septum is supported by cartilage and bone, not the nasal conchae.
Question 41:
Where do the posterior ethmoidal air cells drain into?
A) Superior concha
B) Middle meatus
C) Inferior concha
D) Nasolacrimal duct
E) Superior meatus
Answer: E) Superior meatus
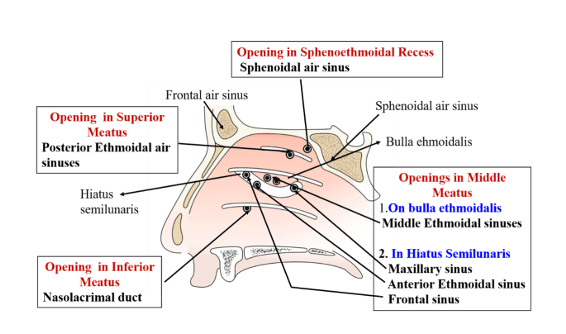
Explanation: The posterior ethmoidal air cells drain into the superior meatus of the nasal cavity, which helps to humidify and filter the inspired air.
a) Superior concha: Incorrect. The posterior ethmoidal air cells do not drain directly into the superior concha.
b) Middle meatus: Incorrect. The middle meatus is the drainage site for the anterior ethmoidal air cells and maxillary sinus, not the posterior ethmoidal air cells.
c) Inferior concha: Incorrect. The inferior concha is unrelated to the drainage of the ethmoidal air cells; it drains the nasolacrimal duct.
d) Nasolacrimal duct: Incorrect. The nasolacrimal duct drains tears from the eyes into the nasal cavity, not the ethmoidal air cells.

Question 42:
Where does the maxillary sinus drain into?
A) Superior concha
B) Middle meatus
C) Inferior concha
D) Nasolacrimal duct
E) Semilunar hiatus
Answer: E) Semilunar hiatus
Explanation: The maxillary sinus drains into the nasal cavity through the semilunar hiatus, which is part of the middle meatus. This drainage pathway is essential for maintaining proper nasal function and health.
a) Superior concha: Incorrect. The maxillary sinus does not drain into the superior concha.
b) Middle meatus: inCorrect. While the maxillary sinus drains into the middle meatus, it’s more specifically through the semilunar hiatus, therefore answer option E is more correct
c) Inferior concha: Incorrect. The inferior concha is associated with the drainage of the nasolacrimal duct, not the maxillary sinus.
d) Nasolacrimal duct: Incorrect. The nasolacrimal duct drains tears into the inferior meatus, not the maxillary sinus.
Question 43:
Among the following structures, which one is not a component of Little’s area in the nasal cavity?
A) Anterior ethmoidal artery
B) posterior ethmoidal artery
C) superior labial artery
D) Sphenopalatine artery
E) Greater palatine artery
Answer: B) Posterior Ethmoidal Artery
Explanation: Little’s area, also known as Kiesselbach’s plexus, comprises the anterior ethmoidal artery, Greater palatine, Sphenopalatine, and superior labial artery, and the superior labial artery. The posterior ethmoidal artery does not contribute to Little’s area. (TIP: a way to remember the blood vessels in little’s area is with the Mnemonic GASS: Greater Palatine artery, Anterior Ethmoidal artery, Sphenopalatine artery, Superior labial artery)
a) Anterior ethmoidal artery: Incorrect. The anterior ethmoidal artery is a key contributor to Little’s area (Kiesselbach’s plexus), a region rich in blood vessels in the anterior part of the nasal septum.
c) Superior labial artery:Incorrect. The superior labial artery, a branch of the facial artery, contributes to the blood supply of Little’s area.
d) Sphenopalatine artery:Incorrect. The sphenopalatine artery, which is a branch of the maxillary artery, also supplies Little’s area and is a significant contributor.
e) Greater palatine artery:Incorrect. The greater palatine artery, another branch of the maxillary artery, also supplies Little’s area.
Question 44:
In the brainstem, where is the apneustic centre primarily located, playing a role in regulating breathing patterns?
A) Medulla oblongata
B) Midbrain
C) lower Pons
D) Upper Pons
E) Cerebellum
Answer: C) lower Pons
Explanation: The apneustic centre is primarily located in the lower pons region of the brainstem. It is involved in the regulation of breathing patterns, particularly in controlling the duration and intensity of inspiration. The medulla oblongata also plays a crucial role in breathing regulation but is responsible for different aspects of respiratory control. (P.s just remember UPAL – Upper Pneumotaxic, Apneustic Lower)
a) Medulla oblongata: Incorrect. The medulla oblongata is involved in the control of respiration but is more associated with the dorsal and ventral respiratory groups, which control rhythm and rate, rather than the apneustic center.
b) Midbrain: Incorrect. The midbrain is not primarily involved in the control of respiratory patterns; it is associated more with functions like eye movement and auditory processing..
d) Upper Pons: Incorrect. The upper pons contains the pneumotaxic center, which regulates the rate and pattern of breathing, not the apneustic center.
e) Cerebellum: Incorrect. The cerebellum is primarily involved in coordinating movement and balance, not in respiratory control.
Question 45:
According to Boyle’s Law, how is the pressure of a gas related to its volume, assuming constant temperature and amount of gas?
A) Pressure and volume are directly proportional.
B) Pressure and volume are inversely proportional.
C) Pressure remains constant as volume changes.
D) Pressure increases exponentially with volume.
E) Pressure decreases exponentially with volume.
Answer: B) Pressure and volume are inversely proportional.
Explanation: Boyle’s Law states that, at a constant temperature and amount of gas, the pressure of a gas is inversely proportional to its volume. This means that as the volume of a gas decreases, its pressure increases, and vice versa. This law is fundamental in understanding the behaviour of gases, including how changes in volume and pressure affect breathing and lung function in the respiratory system.
a) Pressure and volume are directly proportional: Incorrect. Boyle’s Law states that pressure and volume are inversely proportional, not directly proportional.
c) Pressure remains constant as volume changes: Incorrect. Boyle’s Law indicates that pressure changes with volume; they do not remain constant relative to one another.
d) Pressure increases exponentially with volume: Incorrect. The relationship between pressure and volume is linear and inverse, not exponential.
e) Pressure decreases exponentially with volume: Incorrect. The relationship is not exponential; it is an inverse linear relationship as described by Boyle’s Law.
Question 46:
Which peripheral chemoreceptors are primarily innervated by the glossopharyngeal nerve (cranial nerve IX)?
A) Carotid bodies
B) Aortic bodies
C) Medullary chemoreceptors
D) Pulmonary chemoreceptors
E) J receptors
Answer: A) Carotid bodies
Explanation: The carotid bodies, located near the carotid bifurcation in the neck, are primarily innervated by the glossopharyngeal nerve (cranial nerve IX). These chemoreceptors are sensitive to changes in blood oxygen levels and play a crucial role in regulating ventilation by providing feedback to the respiratory centres in the brainstem when oxygen levels in the blood decrease. This reflex helps maintain adequate oxygenation in the body.
b) Aortic bodies: Incorrect. The aortic bodies, located along the aortic arch, are primarily innervated by the vagus nerve (cranial nerve X), not the glossopharyngeal nerve.
c) Medullary chemoreceptors: Incorrect. Medullary chemoreceptors are located in the brainstem and are not innervated by peripheral nerves such as the glossopharyngeal nerve.
d) Pulmonary chemoreceptors: Incorrect. Pulmonary chemoreceptors are involved in detecting changes in the lungs and are innervated by the vagus nerve (cranial nerve X), not the glossopharyngeal nerve.
e) J receptors: Incorrect. J receptors, located in the lungs, are primarily involved in the reflex control of respiration and are not innervated by the glossopharyngeal nerve.
Question 47:
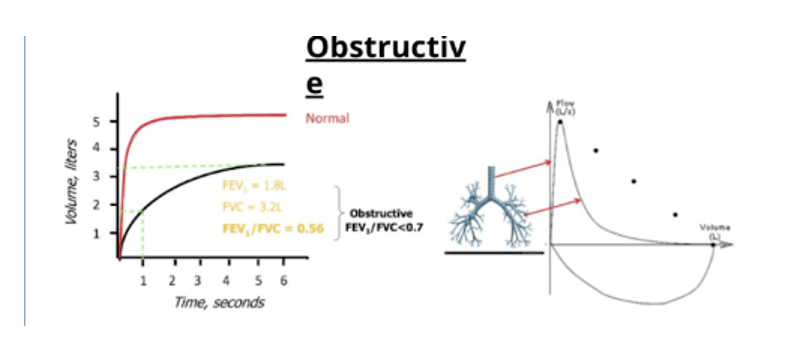
Obstructive pulmonary diseases are typically characterized by:
A) Increased lung compliance
B) Enlarged alveoli
C) Collapse of smaller airways
D) High expiratory flow rates
E) Decreased residual volume
Answer: C) Collapse of smaller airways
Explanation: Obstructive pulmonary diseases, such as chronic obstructive pulmonary disease (COPD) and asthma, are characterized by the narrowing or collapse of smaller airways, which leads to increased airway resistance and difficulty in expelling air from the lungs during expiration. This obstruction results in reduced airflow and impaired lung function.
a) Increased lung compliance: Incorrect. While increased lung compliance may occur in some obstructive diseases like emphysema, it is not a defining feature of all obstructive diseases. The primary issue is airway obstruction.
b) Enlarged alveoli: Incorrect. Enlarged alveoli (as seen in emphysema) can occur, but not all obstructive diseases involve this condition. Asthma, for example, involves airway narrowing without alveolar enlargement.
d) High expiratory flow rates: Incorrect. Obstructive pulmonary diseases are characterized by reduced expiratory flow rates, not increased ones, due to the airway obstruction.
e) Decreased residual volume: Incorrect. In obstructive diseases, residual volume is often increased due to air trapping, not decreased.
Question 48:
In obstructive pulmonary diseases, such as chronic obstructive pulmonary disease (COPD), how is the FEV1:FVC (Forced Expiratory Volume in 1 second to Forced Vital Capacity) ratio typically affected?
A) Increased FEV1:FVC ratio (FEV1:FVC is > 0.7)
B) Decreased FEV1:FVC ratio (FEV1:FVC is < 0.7)
C) Unchanged FEV1:FVC ratio
D) FEV1:FVC ratio is not applicable in obstructive diseases
E) FEV1 and FVC are both zero in obstructive diseases
Answer: B) Decreased FEV1:FVC ratio (FEV1:FVC < 0.7)
Explanation: In obstructive pulmonary diseases, such as COPD, the ability to exhale air quickly and effectively is impaired due to narrowed or collapsed airways. This results in a decreased FEV1:FVC ratio, typically defined as less than 0.7, as the forced expiratory volume in the first second (FEV1) is reduced relative to the forced vital capacity (FVC).
a) Increased FEV1 ratio (FEV1> 0.7): Incorrect. In obstructive diseases, the FEV1 ratio decreases, not increases, because of difficulty exhaling air therefore making FEV1/FVC <0.7
c) Unchanged FEV1 ratio: Incorrect. The ratio is usually decreased in obstructive diseases due to impaired exhalation.
d) FEV1 ratio is not applicable in obstructive diseases: Incorrect. The FEV1 ratio is a crucial measurement in diagnosing obstructive diseases and is very much applicable.
e) FEV1 and FVC are both zero in obstructive diseases: Incorrect. Neither FEV1 nor FVC drops to zero in obstructive diseases, though both may be reduced.
Question 49:
In restrictive pulmonary diseases, such as interstitial lung diseases, how is the FEV1:FVC (Forced Expiratory Volume in 1 second to Forced Vital Capacity) ratio typically affected?
A) Increased FEV1:FVC ratio (>0.8)
B) Decreased FEV1:FVC ratio
C) unchanged FEV1:FVC ratio
D) increased FEV1:FVC ratio (>0.7)
E) FEV1 and FVC are both zero in restrictive diseases
Answer: D) Increased FEV1:FVC ratio (>0.7)
Explanation: In restrictive pulmonary diseases, the lung tissue becomes stiff or less compliant, making it difficult to fully expand the lungs during inhalation. However, the airways themselves remain relatively open and unobstructed. This leads to an increased FEV1:FVC ratio because the forced expiratory volume in the first second (FEV1) remains relatively preserved compared to the forced vital capacity (FVC) which decreased. Both FEV1 and FVC is less than 80% of predicted.
a) Increased FEV1 ratio (>0.8): Incorrect. Although the FEV1 ratio can increase, an increase to greater than 0.8 is typically not seen in all cases of restrictive disease. Instead, the ratio usually increases above 0.7.
b) Decreased FEV1 ratio: Incorrect. In restrictive diseases, both FEV1 and FVC decrease proportionally, so the ratio usually remains normal or increased, not decreased.
c) Unchanged FEV1 ratio: Incorrect. The ratio can change, usually increasing slightly because FVC is reduced more than FEV1.
e) FEV1 and FVC are both zero in restrictive diseases: Incorrect. FEV1 and FVC are reduced in restrictive diseases, but not to zero
Question 50:
How many signals are typically required to fully activate T cells during an immune response?
A) One signal
B) Two signals
C) Three signals
D) Four signals
E) Five signals
Answer: B) Two signals
Explanation: T cells require two signals to become fully activated. The first signal is provided by the binding of the T cell receptor (TCR) to an antigen-presenting cell (APC) displaying a specific antigenic peptide on its surface in the context of major histocompatibility complex (MHC) molecules. This interaction is known as the TCR-MHC/antigen recognition. The second signal is a co-stimulatory signal, typically provided by molecules such as CD28 on the T cell interacting with B7 molecules on the APC. These two signals are essential for T cell activation and the initiation of an immune response.
a) One signal: Incorrect. One signal is not sufficient for full T cell activation. T cells require two distinct signals to initiate a complete immune response.
c) Three signals: Incorrect. Although additional signals (such as cytokines) can enhance the immune response, full activation of T cells requires only two signals.
d) Four signals: Incorrect. T cell activation does not require four signals.
e) Five signals: Incorrect. T cell activation is not that complex; two signals are sufficient to trigger the immune response.
Question 51:
During lung embryology, what surrounds the endoderm, forming the primitive lung bud?
A) Ectoderm
B) Splanchnic mesoderm
C) Pericardium
D) Yolk sac
E) Neuroectoderm
Answer: B) Splanchnic mesoderm
Explanation: During lung development, the endoderm forms the respiratory epithelium, and it is surrounded by the splanchnic mesoderm, which gives rise to the connective tissues, blood vessels, and other structures of the developing lung. This interaction between the endoderm and splanchnic mesoderm is crucial for the formation of the primitive lung bud.
A) Ectoderm (Incorrect) – The ectoderm forms the skin and nervous system, not the structures around the lung bud.
C) Pericardium (Incorrect) – The pericardium surrounds the heart, not the lungs.
D) Yolk sac (Incorrect) – The yolk sac provides early nutrients to the embryo but doesn’t contribute to lung development.
E) Neuroectoderm (Incorrect) – The neuroectoderm forms neural tissues, not the tissues surrounding the lung bud.
Question 52:
What significant event occurs during the pseudoglandular stage of lung development?
A) Formation of alveoli
B) Formation of respiratory bronchioles
C) Formation of terminal bronchioles
D) Formation of primitive alveolar ducts
E) Formation of surfactant-producing cells
Answer: C) Formation of terminal bronchioles
Explanation: The pseudoglandular stage of lung development is characterized by the formation of terminal bronchioles. During this stage, the conducting airways continue to branch and divide, resulting in the formation of smaller and more intricate airways. This stage is essential for the development of the lung’s complex branching structure. Alveoli formation occurs in subsequent stages of lung development.
A) Formation of alveoli (Incorrect) – Alveoli form later, during the alveolar stage, not the pseudoglandular stage.
B) Formation of respiratory bronchioles (Incorrect) – Respiratory bronchioles form during the canalicular stage, not during the pseudoglandular stage.
D) Formation of primitive alveolar ducts (Incorrect) – Alveolar ducts develop in the canalicular stage, after the pseudoglandular stage.
E) Formation of surfactant-producing cells (Incorrect) – Surfactant-producing cells form later, during the saccular and alveolar stages, not during the pseudoglandular stage.
Question 53:
Embryologically, from which germ layer does the pleura originate?
A) Endoderm
B) Ectoderm
C) Mesoderm
D) Ectomesenchyme
E) Neuroectoderm
Answer: C) Mesoderm
Explanation: The pleura, which is the membrane that surrounds the lungs, originates embryologically from the mesoderm. The mesoderm is one of the three primary germ layers during early embryonic development and gives rise to various tissues, including the musculoskeletal system, connective tissues, and serous membranes like the pleura. The parietal pleura is formed by the somatopleuric mesoderm whereas the visceral pleura is formed by the splanchnopleuric mesoderm.
A) Endoderm (Incorrect) – The endoderm forms the respiratory lining but does not contribute to the pleura.
B) Ectoderm (Incorrect) – The ectoderm forms external tissues like skin and nervous tissue, not the pleura.
D) Ectomesenchyme (Incorrect) – Ectomesenchyme forms facial structures, not the pleura.
E) Neuroectoderm (Incorrect) – Neuroectoderm gives rise to neural tissues, not the pleura.
Question 54:
In the human respiratory system, where is the last place where cartilage is found?
A) Trachea
B) Bronchi
C) Bronchioles
D) Terminal bronchioles
E) Terminal bronchi
Answer: E) Terminal bronchi
Explanation: Cartilage provides structural support to the airways in the respiratory system. It is found in the trachea and main bronchi but decreases as the airways become smaller. The respiratory bronchioles are the smallest branches of the airways and do not contain cartilage. The terminal bronchus is the last part where cartilage is found.
A) Trachea (Incorrect) – While cartilage is found in the trachea, it is also present in the bronchi, which are further down.
B) Bronchi (incorrect) – While the Bronchi do contain cartilage rings, this is more of a vague answer as there’s many types of bronchi so doesn’t specify which specific bronchi it is whereas option E is more specific and more correct
C) Bronchioles (Incorrect) – Bronchioles lack cartilage and rely on smooth muscle for support.
D) Terminal bronchioles (Incorrect) – These are too small to contain cartilage and only have smooth muscle.

Question 55:
In the human respiratory system, at which point does the BP segment begin?
A) Primary bronchi
B) Secondary bronchi
C) Tertiary bronchi
D) Terminal bronchus
E) Respiratory bronchioles
Answer: C) Tertiary bronchi
Explanation: Each bronchopulmonary segment is supplied by a segmental (tertiary) bronchus. A bronchopulmonary segment constitutes a section of the lung that receives its blood supply from a designated segmental/ tertiary bronchi and its associated blood vessels. These arteries stem from both the pulmonary and bronchial arteries, coursing through the core of the segment. Concurrently, veins and lymphatic vessels collect and transport fluids along the periphery of the segment.
A) Primary bronchi: Incorrect. The primary bronchi are the first division of the trachea and do not mark the beginning of the bronchopulmonary segment.
B) Secondary bronchi: Incorrect. The secondary bronchi further divides into tertiary bronchi but does not directly indicate the start of a bronchopulmonary segment.
D) Terminal bronchus: Incorrect. The terminal bronchioles are beyond the point where the bronchopulmonary segments are defined.
E) Respiratory bronchioles: Incorrect. Respiratory bronchioles are involved in gas exchange and are not the point where the bronchopulmonary segment begins.

Question 56:
How does a fixed upper airway obstruction affect the flow-volume graph?
a) Causes a steeper initial rise in flow
b) Results in a more pronounced plateau phase
c) Leads to a longer rapid rise at the start
d) Causes a leftward shift of the graph
e) No longer exhibits a rapid rise at the start
Answer: e) No longer exhibits a rapid rise at the start
Explanation: In the presence of a fixed upper airway obstruction, the flow-volume graph is characterized by the absence of the typical rapid rise in flow that occurs at the beginning of a normal expiratory curve. This obstruction restricts airflow, resulting in a distinct alteration of the graph pattern.
a) Causes a steeper initial rise in flow: Incorrect. A fixed upper airway obstruction does not result in a steeper initial rise.
b) Results in a more pronounced plateau phase: Incorrect. The plateau phase is not typically altered in this manner by a fixed obstruction.
c) Leads to a longer rapid rise at the start: Incorrect. The rapid rise at the start is diminished, not extended.
d) Causes a leftward shift of the graph: Incorrect. A leftward shift is not typically caused by a fixed airway obstruction.
Question 57:
What is the likely consequence of a defect in surfactant production in a foetus?
a) Increased lung compliance
b) Reduced lung compliance
c) Decreased alveolar surface area
d) Elevated pulmonary blood pressure
e) Enhanced foetal lung maturation
Answer: b) Reduced lung compliance
Explanation: Surfactant plays a crucial role in reducing surface tension within the alveoli, preventing their collapse during expiration. A defect in surfactant production would lead to increased surface tension, making it more difficult to inflate the lungs and reducing lung compliance. This can result in respiratory distress syndrome (RDS) in premature infants.
a) Increased lung compliance: Incorrect. A lack of surfactant would decrease lung compliance, not increase it due to the increase in surface tension of alveoli making them haver a lower surface area and harder to be filled with air and expand.
c) Decreased alveolar surface area: Incorrect. The surface area might be indirectly affected due to alveolar collapse, but the primary issue is reduced compliance.
d) Elevated pulmonary blood pressure: Incorrect. While pulmonary complications can arise, the direct consequence of reduced surfactant is not elevated pulmonary blood pressure.
e) Enhanced foetal lung maturation: Incorrect. A defect in surfactant production would impair, not enhance, lung maturation.
Question 58:
What does Dalton’s law state?
a) The total pressure of a gas mixture is equal to the sum of the partial pressures of its individual gases.
b) The volume of a gas is inversely proportional to its pressure.
c) The total pressure of a gas mixture is directly proportional to its volume.
d) Gas particles move randomly and collide with each other.
e) Gas pressure increases with increasing temperature.
Answer: a) The total pressure of a gas mixture is equal to the sum of the partial pressures of its individual gases.
Explanation: Dalton’s law of partial pressures states that in a mixture of non-reacting gases, the total pressure is the sum of the partial pressures exerted by each individual gas in the mixture. This law is fundamental in understanding gas behaviour in mixtures.
b) The volume of a gas is inversely proportional to its pressure: Incorrect. This describes Boyle’s law, not Dalton’s law.
c) The total pressure of a gas mixture is directly proportional to its volume: Incorrect. This does not describe Dalton’s law or any well-known gas law.
d) Gas particles move randomly and collide with each other: Incorrect. This describes the kinetic theory of gases, not Dalton’s law.
e) Gas pressure increases with increasing temperature: Incorrect. This describes Gay-Lussac’s law, not Dalton’s law.
Question 59:
What best describes what happens to the diffusion capacity of the lungs during moderate to intense exercise?
A) It decreases
B) It remains unchanged
C) It increases
D) It becomes irregular and unpredictable
E) It becomes linear and constant
Answer: C) It increases
Explanation: During moderate to intense exercise, various physiological adaptations occur that enhance the efficiency of gas exchange in the lungs. These adaptations include increased cardiac output, improved alveolar ventilation, and the opening of previously closed pulmonary capillaries. These factors collectively increase the diffusion capacity, allowing for more efficient oxygen uptake and carbon dioxide removal, which is essential for meeting the increased metabolic demands of exercising muscles.
A) It decreases:Incorrect. During exercise, the lungs typically enhance their ability to exchange gases.
B) It remains unchanged:Incorrect. Lung diffusion capacity usually increases during exercise due to better perfusion and ventilation matching.
D) It becomes irregular and unpredictable:Incorrect. Lung diffusion capacity increases in a predictable manner during exercise.
E) It becomes linear and constant:Incorrect. While diffusion capacity increases during exercise, it is not necessarily linear or constant.
Question 60:
Where does carbon dioxide (CO2) primarily bind to haemoglobin in the blood?
A) Haem iron within the haem groups.
B) Globin protein chains.
C) Porphyrin ring.
D) Carbonate ions.
E) Haemocyte located in plasma proteins.
Answer: B) Globin protein chains.
Explanation: Carbon dioxide primarily binds to the globin protein chains of haemoglobin, forming carbaminohaemoglobin. This binding primarily occurs at the amino acid residues of the globin chains rather than at the haem iron, which is responsible for oxygen binding. This binding helps transport a portion of CO2 from the tissues to the lungs for elimination.
A) Haem iron within the haem groups: Incorrect. The haem iron binds to oxygen, not carbon dioxide.
C) Porphyrin ring: Incorrect. The porphyrin ring structure is part of the haem group that binds oxygen, not carbon dioxide.
D) Carbonate ions: Incorrect. Carbon dioxide does not bind to haemoglobin in the form of carbonate ions. However the majority of Carbon dioxide is transported as carbonate ions in blood (70%)
E) Haemocyte located in plasma proteins: Incorrect. Haemocytes are not the primary binding sites for carbon dioxide.
Question 61:
During the Hamburger shift in red blood cells, which ion is exchanged for bicarbonate ions (HCO3-) to maintain electrochemical neutrality in the cell?
A) Sodium ions (Na+)
B) Nitrate ions (NO3-)
C) Calcium ions (Ca2+)
D) Phosphate ions (PO4 3-)
E) Chloride ions (Cl-)
Answer: E) Chloride ions (Cl-)
Explanation: During the hamburger/chloride shift, chloride ions (Cl-) are exchanged for bicarbonate ions (HCO3-) in red blood cells. This exchange helps maintain electrochemical neutrality within the cell as bicarbonate ions are transported from the tissues to the lungs for elimination while chloride ions enter the cell, preserving the overall charge balance.
A) Sodium ions (Na+ : Incorrect. Sodium ions are not involved in the chloride shift process.
B) Nitrate ions (NO3-): Incorrect. Nitrate ions are not exchanged during the chloride shift.
C) Calcium ions (Ca2+): Incorrect. Calcium ions do not play a role in the chloride shift.
D) Phosphate ions (PO4 3-): Incorrect. Phosphate ions are not involved in this exchange.

Question 62:
Which of the following statements about haemoglobin’s binding affinity is correct?
a) Deoxyhaemoglobin has a greater affinity for H+ ions than oxyhaemoglobin.
b) Haemoglobin always has the same affinity for H+ ions, regardless of its oxygenation state.
c) Oxygenated haemoglobin has a greater affinity for H+ ions than deoxyhaemoglobin.
d) Haemoglobin’s binding affinity for H+ ions is solely determined by pH levels in the blood.
e) Foetal haemoglobin (HbF) has a lower affinity for O2 compared to adult haemoglobin.
Answer: A. Deoxyhaemoglobin has a greater affinity for H+ ions than oxyhaemoglobin.
Explanation: Deoxyhaemoglobin, the form of haemoglobin without bound oxygen, has a higher affinity for H+ ions (protons) than oxyhaemoglobin, which is oxygen-bound haemoglobin. This property is essential for the Bohr effect, where haemoglobin releases oxygen more readily in tissues with lower pH (higher H+ concentration), facilitating oxygen delivery where it is needed most.
b) Haemoglobin always has the same affinity for H+ ions, regardless of its oxygenation state:Incorrect. Haemoglobin’s affinity for H+ ions changes depending on its oxygenation state.
c) Oxygenated haemoglobin has a greater affinity for H+ ions than deoxyhaemoglobin:Incorrect. Deoxyhaemoglobin, not oxygenated haemoglobin, has a higher affinity for H+ ions.
d) Haemoglobin’s binding affinity for H+ ions is solely determined by pH levels in the blood:Incorrect. While pH levels affect haemoglobin’s affinity for H+ ions, oxygenation state also plays a critical role.
e) Foetal haemoglobin (HbF) has a lower affinity for O2 compared to adult haemoglobin:Incorrect. Foetal haemoglobin (HbF) actually has a higher affinity for oxygen than adult haemoglobin (HbA), which is benefiical for oxygen transfer across the placenta due to the placental blood having a lower blood O2 level.
Question 63:
A 12-year-old girl presents with chest pain and breathing difficulties. Arterial blood gas analysis reveals a pH of 7.2 (7.35-7.45), a partial pressure of carbon dioxide (CO2) of 67 mmHg (35-45), and a bicarbonate (HCO3-) level of 24 mEq/L (22-26). What type of acid-base disturbance is primarily indicated by these values?
a) Uncompensated respiratory acidosis
b) Compensated respiratory acidosis
c) Uncompensated metabolic acidosis
d) Compensated metabolic acidosis
e) Uncompensated respiratory alkalosis
Answer: A. Uncompensated respiratory acidosis
Explanation: The arterial blood gas results indicate uncompensated respiratory acidosis. The low pH and elevated CO2 levels suggest that the primary disturbance is related to the respiratory system, with inadequate removal of CO2, leading to increased carbonic acid and lowered pH. The bicarbonate levels are within the normal range, indicating that full metabolic compensation has not occurred.
b) Compensated respiratory acidosis: Incorrect. Compensation would involve a corresponding rise in bicarbonate levels, which is not present in this case and a ph within the normal range which is not the case.
c) Uncompensated metabolic acidosis: Incorrect. The bicarbonate level is normal, and the CO2 level is elevated, indicating a respiratory issue rather than a metabolic one.
d) Compensated metabolic acidosis: Incorrect. This is respiratory acidosis due to the CO2 level being elevated but the bicarbonate levels being normal ( in metabolic acidosis you would expect normal CO2 levels and low Bicarbonate levels), indicating a respiratory issue rather than a metabolic one. Furthermore this is not compensated due to the low Ph and the normal Bicarbonate levels ( you would expect to see an increase if it was compensated)
e) Uncompensated respiratory alkalosis: Incorrect. Respiratory alkalosis would involve a higher pH and lower CO2 levels.
Question 64:
An 8-year-old child presents with weight loss and dehydration. Arterial blood gas analysis reveals the following values in order: pH 7.24 (normal range: 7.35-7.45), partial pressure of carbon dioxide (CO2) 22 mmHg (normal range: 35-45 mmHg), bicarbonate (HCO3-) 12 mEq/L (normal range: 22-26 mEq/L). What type of acid-base disturbance is primarily indicated by these values?
a) Uncompensated respiratory acidosis
b) Compensated respiratory acidosis
c) compensated metabolic acidosis
d) Partially compensated metabolic acidosis
e) Uncompensated respiratory alkalosis
Answer: D. Partially compensated metabolic acidosis
Explanation: The arterial blood gas results indicate partially compensated metabolic acidosis. The low pH and bicarbonate levels below the normal range suggest a primary metabolic acidosis since the symptoms don’t fit respiratory. The slightly decreased CO2 levels indicate partial compensation by the respiratory system to restore the pH towards normal.
a) Uncompensated respiratory acidosis: Incorrect. The bicarbonate levels are low, indicating a primary metabolic disturbance rather than a respiratory issue. Respiratory acidosis would mean elevated CO2 levels and normal bicarbonate levels.
b) Compensated respiratory acidosis: Incorrect. The disturbance is primarily metabolic, not respiratory, and the compensation is partial, not full.
c) Compensated metabolic acidosis: Incorrect. Compensation is partial, as the pH is still outside the normal range.
e) Uncompensated respiratory alkalosis: Incorrect. The disturbance is acidosis, not alkalosis due to the low Ph. Furthermore it is metabolic acidosis due to the Bicarb levels being low.
Question 65:
A 25-year-old individual presents with a persistent cough. Arterial blood gas analysis reveals the following values: pH 7.43 (normal range: 7.35-7.45), partial pressure of carbon dioxide (CO2) 60 mmHg (normal range: 35-45 mmHg), bicarbonate (HCO3-) 32 mEq/L (normal range: 22-26 mEq/L). What type of acid-base disturbance is primarily indicated by these values?
a) Uncompensated respiratory acidosis
b) compensated metabolic acidosis
c) Uncompensated metabolic alkalosis
d) Partially compensated metabolic alkalosis
e) Fully compensated respiratory acidosis
Answer: E. Fully compensated respiratory acidosis
Explanation:
The arterial blood gas results indicate fully compensated respiratory acidosis. The pH is within the normal range, suggesting compensation through increased bicarbonate levels (HCO3-), which are above the normal range. The elevated CO2 levels and the presence of a cough indicate a primary respiratory acidosis, likely due to impaired gas exchange in the lungs. The increased bicarbonate levels represent the metabolic compensation that has occurred in response to the respiratory acidosis, bringing the pH back into the normal range.
a) Uncompensated respiratory acidosis: Incorrect. The pH is within the normal range, indicating compensation.
b) compensated metabolic acidosis: Incorrect.whilst it it is compensated as the pH is normal, it is not Metabolic acidosis rather respiratory acidosis this is due to the CO2 levels being high suggesting a respiratory issue.
c) Uncompensated metabolic alkalosis: Incorrect. The primary disturbance is respiratory, not metabolic.
d) Partially compensated metabolic alkalosis: Incorrect. The primary disturbance is respiratory, not metabolic.
Question 66: A 22-year-old patient with fever presents with altered blood gas values: pH of 7.2 (normal range: 7.35-7.45), a partial pressure of carbon dioxide (CO2) of 60 mmHg (normal range: 35-45 mmHg), and a bicarbonate (HCO3-) level of 19 mEq/L (normal range: 22-26 mEq/L). What type of acid-base disturbance is primarily indicated by these values?
a) Uncompensated respiratory acidosis
b) Uncompensated metabolic acidosis
c) Uncompensated respiratory alkalosis
d) Compensated metabolic acidosis
e) Uncompensated mixed acidosis
Answer:
e) Uncompensated mixed acidosis
Explanation:
The arterial blood gas results suggest uncompensated mixed acidosis. The low pH indicates acidosis, and the elevated CO2 levels point to a primary respiratory acidosis, possibly due to impaired lung function. Additionally, the decreased bicarbonate (HCO3-) levels indicate a primary metabolic acidosis. The absence of full compensation, either metabolic or respiratory, classifies this as uncompensated mixed acidosis.
a) Uncompensated respiratory acidosis: Incorrect. Although the elevated CO2 indicates respiratory acidosis, the decreased bicarbonate levels also suggest a metabolic component, so this is not purely respiratory acidosis.
b) Uncompensated metabolic acidosis: Incorrect. The presence of high CO2 levels indicates that respiratory acidosis is also present, so this is not purely metabolic acidosis.
c) Uncompensated respiratory alkalosis: Incorrect. Alkalosis is not indicated by the low pH. The patient is in an acidosis state, not alkalosis.
d) Compensated metabolic acidosis: Incorrect. While metabolic acidosis is present, compensation has not fully occurred as indicated by the persistently low pH. Additionally the CO2 levels are high suggesting its also respiratory acidosis.
Question 67:
What is the primary function of erythropoietin (EPO)?
a) Regulation of blood glucose levels
b) Stimulation of muscle growth
c) Promotion of red blood cell production
d) Inhibition of blood clotting
e) Enhancement of bone density
Answer:
c) Promotion of red blood cell production
Explanation:
Erythropoietin (EPO) primarily functions to stimulate the production of red blood cells (erythropoiesis) in response to low oxygen levels in the blood. This hormone is released by the kidneys and, to a lesser extent, the liver, and it plays a crucial role in maintaining oxygen homeostasis in the body. EPO promotes the differentiation and maturation of red blood cell precursors in the bone marrow, increasing the oxygen-carrying capacity of the blood.
a) Regulation of blood glucose levels:Incorrect. Erythropoietin (EPO) is not involved in blood glucose regulation. This function is primarily managed by hormones like insulin and glucagon.
b) Stimulation of muscle growth: Incorrect. EPO is not involved in muscle growth; this is primarily the role of hormones like growth hormone and testosterone.
d) Inhibition of blood clotting:Incorrect. EPO does not play a role in inhibiting blood clotting. This function is managed by anticoagulants like heparin.
e) Enhancement of bone density:Incorrect. EPO does not enhance bone density. This is primarily regulated by calcium, vitamin D, and hormones like parathyroid hormone.
Question 68:
What happens to the oxygen dissociation curve when individuals ascend to high altitudes where oxygen levels are lower?
a) The curve shifts to the right, indicating decreased oxygen affinity of haemoglobin.
b) The curve shifts to the left, indicating increased oxygen affinity of haemoglobin.
c) The curve remains unchanged, with no shift in oxygen affinity.
d) The curve becomes steeper, making it more difficult for haemoglobin to release oxygen.
e) The curve shifts to the left causing a decreased oxygen affinity of haemoglobin and causing more CO2 to bind to globin
Answer:
b) The curve shifts to the left, indicating increased oxygen affinity of haemoglobin.
Explanation:
At high altitudes where oxygen levels are lower, the body adapts to enhance its oxygen-carrying capacity. One of the adaptations is a leftward shift of the oxygen dissociation curve. This shift indicates an increased affinity of haemoglobin for oxygen, making it easier for haemoglobin to bind to oxygen in the lungs and pick up oxygen more effectively. This adaptation helps improve oxygen uptake despite the reduced availability of oxygen at high altitudes.
a) The curve shifts to the right, indicating decreased oxygen affinity of haemoglobin: Incorrect. A rightward shift usually occurs in conditions like increased CO2, increased temperature, or acidosis, not high altitudes.
c) The curve remains unchanged, with no shift in oxygen affinity: Incorrect. The curve does shift to the left as an adaptive mechanism in response to low oxygen levels at high altitudes.
d) The curve becomes steeper, making it more difficult for haemoglobin to release oxygen: Incorrect. The curve does not become steeper in this context. The shift is to the left, which increases oxygen binding affinity, but it doesn’t change the steepness of the curve.
e) The curve shifts to the left causing a decreased oxygen affinity of haemoglobin and causing more CO2 to bind to globin: Incorrect. A leftward shift increases oxygen affinity, not decreases it, and does not directly impact CO2 binding.
Question 69:
What is the effect of hypoxia on the pulmonary vasculature in the lungs?
a) Hypoxia decreases pulmonary vascular resistance.
b) Hypoxia has no effect on pulmonary vascular resistance.
c) Hypoxia increases pulmonary vascular resistance.
d) Hypoxia causes pulmonary vasodilation.
e) None of the above.
Answer:
c) Hypoxia increases pulmonary vascular resistance.
Explanation:
Hypoxia, or low oxygen levels in the blood, triggers vasoconstriction (narrowing of blood vessels) in the pulmonary arterioles. This increase in pulmonary vascular resistance is a physiological response aimed at diverting blood flow away from poorly ventilated areas of the lungs to regions with better oxygenation. This mechanism helps optimize oxygen exchange in the lungs, even under conditions of reduced oxygen availability.
a) Hypoxia decreases pulmonary vascular resistance: Incorrect. Hypoxia does not decrease pulmonary vascular resistance; in fact, it does the opposite.
b) Hypoxia has no effect on pulmonary vascular resistance: Incorrect. Hypoxia does have a significant effect on increasing pulmonary vascular resistance.
d) Hypoxia causes pulmonary vasodilation: Incorrect. Hypoxia typically causes vasoconstriction in the pulmonary circulation, not vasodilation.
e) None of the above: Incorrect. Hypoxia increases pulmonary vascular resistance.
Question 70:
At high altitudes, individuals often experience respiratory alkalosis due to increased ventilation. What effect does this alkalotic condition have on the production of 2,3-DPG (2,3-diphosphoglycerate) in red blood cells?
a) Alkalosis increases the production of 2,3-DPG.
b) Alkalosis decreases the production of 2,3-DPG.
c) Alkalosis has no effect on 2,3-DPG production.
d) Alkalosis initially increases but then decreases 2,3-DPG production.
e) It has a modulating effect on production of 2,3-DPG.
Answer:
b) Alkalosis decreases the production of 2,3-DPG.
Explanation:
Respiratory alkalosis, which occurs at high altitudes due to increased ventilation, leads to a left shift in the oxygen dissociation curve. This shift decreases the production of 2,3-DPG, making haemoglobin have an increased affinity for O2 in the high altitude condition which has less O2 than normal.
a) Alkalosis increases the production of 2,3-DPG: Incorrect. Respiratory alkalosis typically inhibits 2,3-DPG production rather than increasing it. 2,3-DPG production is generally stimulated by conditions like hypoxia, acidosis, or anemia, not alkalosis.
c) Alkalosis has no effect on 2,3-DPG production: Incorrect. Alkalosis does have an effect, specifically a reducing effect, on 2,3-DPG production. Therefore, this option is incorrect.
d) Alkalosis initially increases but then decreases 2,3-DPG production: Incorrect. Alkalosis does not cause an initial increase in 2,3-DPG production; it typically leads to a decrease in production from the onset.
e) It has a modulating effect on production of 2,3-DPG: Incorrect. While factors like hypoxia modulate 2,3-DPG production, alkalosis specifically decreases it rather than having a purely modulatory effect.
Question 71:
In response to respiratory alkalosis caused by increased ventilation at high altitudes, the kidneys play a role in maintaining acid-base balance. What is the primary action of the kidneys in this situation?
a) Increased reabsorption of bicarbonate (HCO3-)
b) Increased excretion of bicarbonate (HCO3-)
c) Decreased secretion of bicarbonate (HCO3-)
d) Decreased secretion of hydrogen ions (H+)
e) Increased secretion of hydrogen ions (H+)
Answer:
b) increased excretion of Bicarbonate ions (HCO3-)
Explanation:
In response to respiratory alkalosis, the kidneys increase the excretion of bicarbonate (HCO3-) to help compensate for the alkalotic condition. This process helps to compensate to normalise pH levels in the blood.
a) Increased reabsorption of bicarbonate (HCO3-): Incorrect. Increasing the reabsorption of bicarbonate would exacerbate alkalosis by raising blood pH even further.
c) Decreased secretion of bicarbonate (HCO3-): Incorrect. Decreasing bicarbonate secretion would lead to increased levels of bicarbonate in the blood, which would worsen the alkalosis.
d) Decreased secretion of hydrogen ions (H+): Incorrect. While a reduction in hydrogen ion secretion could theoretically affect pH, the primary compensatory response is focused on bicarbonate excretion, not hydrogen ion retention.
e) Increased secretion of hydrogen ions (H+): Incorrect. Increasing hydrogen ion secretion would reduce blood acidity, which is the opposite of what is needed to correct alkalosis.
Question 72:
In individuals exposed to high-altitude hypoxia for an extended period, which adaptive process plays a crucial role in increasing oxygen delivery to tissues?
a) Erythrocyte apoptosis
b) Haemostasis inhibition
c) Angiogenesis
d) Bronchoconstriction
e) Increased blood viscosity
Answer:
c) Angiogenesis (growth of new blood vessels)
Explanation:
Chronic exposure to high-altitude hypoxia triggers the growth of new blood vessels, a process known as angiogenesis. This adaptation helps enhance oxygen delivery to tissues, improving overall tissue oxygenation despite lower oxygen availability at high altitudes. Furthermore hypoxia over an extended period of time will stimulate EPO production by kidneys to increase the amount of haemoglobin that can bind to O2.
a) Erythrocyte apoptosis: Incorrect. Erythrocyte apoptosis (programmed cell death of red blood cells) would decrease oxygen-carrying capacity and is not an adaptive mechanism in response to hypoxia. In reality the opposite occurs with increased RBC production due to EPO production.
b) Haemostasis inhibition: Incorrect. Inhibiting haemostasis (the process of blood clotting) does not play a role in increasing oxygen delivery to tissues during high-altitude adaptation.
d) Bronchoconstriction: Incorrect. Bronchoconstriction would reduce airflow and impair oxygenation, which is not an adaptive response to hypoxia.
e) Increased blood viscosity: Incorrect. Although increased blood viscosity can occur due to polycythemia (increased red blood cell count), it can actually impede blood flow and oxygen delivery. The primary beneficial adaptation is angiogenesis, not increased blood viscosity.
Question 73:
During prenatal development, where is the primary site for gaseous exchange?
a) Lungs
b) Umbilical cord
c) Heart
d) Liver
e) Placenta
Answer: e) Placenta
Explanation: The placenta is the specialized organ in prenatal development responsible for facilitating the exchange of oxygen and carbon dioxide between the foetal and maternal bloodstreams. It allows for the transfer of nutrients and removal of waste products, playing a crucial role in foetal development.
a) Lungs: Incorrect. The lungs are not the primary site for gaseous exchange during prenatal development. Although they are the main site post-birth, the fetal lungs are filled with fluid and are not involved in oxygen exchange until after birth when the newborn takes its first breath.
b) Umbilical cord: Incorrect. The umbilical cord acts as a conduit for blood between the fetus and the placenta, but it is not the site where gas exchange occurs. The actual exchange of gases happens in the placenta.
c) Heart: Incorrect. The heart is responsible for pumping blood throughout the fetal body but does not perform gas exchange. Oxygenated blood comes from the placenta, and the heart circulates it.
d) Liver: Incorrect. While the liver plays a significant role in metabolism and processing nutrients, it does not serve as a site for gaseous exchange in fetal development.
Question 74:
Why is breathing inhibited during foetal development and to prevent the inhalation of what…
a) Amniotic fluid
b) Umbilical cord
c) Blood
d) Surfactant
e) Foetal blood
Answer: A) amniotic fluid
Explanation: Breathing is inhibited during foetal development to prevent the inhalation of amniotic fluid.as the foetus develops the lungs are filled with amniotic fluid. Therefore inhaling the amniotic fluid is dangerous as not only can Meconium( the earliest stool of a new-born) be present in the amniotic fluid. Inhaling amniotic fluid can lead to respiratory issues and complications for the new-born.
b) Umbilical cord: Incorrect. The umbilical cord is involved in transporting blood between the fetus and placenta, but it is not a substance that could be inhaled.
c) Blood: Incorrect. The inhibition of breathing during fetal development is not primarily to prevent the inhalation of blood. The fetus does not inhale any fluids or gases until after birth.
d) Surfactant: Incorrect. Surfactant is a substance produced by the lungs to reduce surface tension and prevent alveolar collapse, but it is not something that would be inhaled by the fetus. Surfactant is crucial post-birth.
e) Fetal blood: Incorrect. Fetal blood circulates within the fetus and placenta, but it is not a substance that could be inhaled.
Question 75:
What type of respiratory disease can obesity contribute to?
a) Obstructive lung disease
b) Restrictive lung disease
c) emphysema
d) Autoimmune lung disease
e) bronchitis
Answer: b) Restrictive lung disease
Explanation: Obesity can contribute to restrictive lung disease, which is characterized by reduced lung expansion and decreased lung volumes. The excess fat in the chest and abdominal area can limit the ability of the lungs to fully expand during inhalation, leading to decreased lung function.
a) Obstructive lung disease: Incorrect. While obesity can exacerbate conditions like asthma, it primarily contributes to restrictive lung disease rather than obstructive lung diseases like COPD.
c) Emphysema: Incorrect. Emphysema is a type of obstructive lung disease often associated with smoking, not obesity. Obesity more commonly contributes to restrictive lung disease.
d) Autoimmune lung disease: Incorrect. Autoimmune lung diseases are related to immune system dysfunction and are not directly caused by obesity.
e) Bronchitis: Incorrect. Bronchitis is an obstructive condition, and while obesity can exacerbate respiratory conditions, it primarily contributes to restrictive lung disease.
Question 76:
What chemical stimulus promotes surfactant production by type 2 pneumocytes in the alveoli, especially during birth?
a) Acetylcholine
b) Carbonic Acid
c) Cortisol
d) Nitric oxide
e) Prostaglandins
Answer: c) Cortisol
Explanation: Cortisol, a steroid hormone, is a key chemical stimulus for the production of surfactant by type 2 pneumocytes in the alveoli. This hormone helps in the maturation of the foetal lungs and enhances the synthesis of surfactant, which is essential for reducing surface tension within the alveoli and preventing their collapse during exhalation. With birth being a stressful event, cortisol levels are high.
a) Acetylcholine: Incorrect. Acetylcholine is a neurotransmitter that plays a role in muscle contraction and parasympathetic responses but does not directly stimulate surfactant production.
b) Carbonic acid: Incorrect. Carbonic acid is involved in the regulation of blood pH but does not promote surfactant production.
d) Nitric oxide: Incorrect. Nitric oxide is a vasodilator involved in regulating blood flow, not surfactant production.
e) Prostaglandins: Incorrect. Prostaglandins are involved in inflammation and smooth muscle contraction but do not directly stimulate surfactant production.
Question 77:
What is the primary effect of epinephrine acting on β2-adrenergic receptors within the respiratory system?
a) Bronchoconstriction
b) Increased mucus production
c) Bronchodilation
d) Vasoconstriction
e) Reduced ventilation
Answer: c) Bronchodilation
Explanation: Epinephrine, when acting on β2-adrenergic receptors in the respiratory system, primarily induces bronchodilation. This leads to the relaxation of smooth muscle in the airways, resulting in an expansion of the air passages and improved airflow, which is beneficial in cases of bronchoconstriction or asthma exacerbation.
a) Bronchoconstriction: Incorrect. Epinephrine causes bronchodilation, not bronchoconstriction. Bronchoconstriction is associated with the activation of different pathways, such as the parasympathetic system.
b) Increased mucus production: Incorrect. Epinephrine does not increase mucus production. Its primary effect in the respiratory system is bronchodilation.
d) Vasoconstriction: Incorrect. Although epinephrine causes vasoconstriction, this effect is mediated by α-adrenergic receptors, not β2-adrenergic receptors, which are more involved in bronchodilation in the respiratory system.
e) Reduced ventilation: Incorrect. Epinephrine increases ventilation by dilating the bronchioles and enhancing airflow, not reducing it.
Question 78:
In the context of respiratory defence, what is the primary role of opsonins?
a) Stimulate mucus production
b) Neutralize toxins released by pathogens
c) Promote bronchoconstriction
d) Enhance phagocytosis via marking
e) promote the production of antibodies
Answer: d) Enhance phagocytosis via marking
Explanation: Opsonins are molecules that enhance the process of phagocytosis by marking pathogens for ingestion and destruction by phagocytes like macrophages and neutrophils. This is a crucial component of the body’s defence against respiratory infections, as it helps in the efficient removal of invading microorganisms from the airways.
a) Stimulate mucus production: Incorrect. Opsonins do not stimulate mucus production. Their role is to mark pathogens for destruction.
b) Neutralize toxins released by pathogens: Incorrect. Neutralisation of toxins is primarily carried out by antibodies, not opsonins.
c) Promote bronchoconstriction: Incorrect. Opsonins are involved in enhancing phagocytosis, not in regulating airway constriction.
e) Promote the production of antibodies: Incorrect. Opsonins themselves do not promote antibody production; instead, they enhance the immune response by marking pathogens for phagocytosis.
Question 79:
In individuals with cystic fibrosis (CF), which of the following best describes the primary issue related to CFTR channels?
a) Underproduction of mucus in the airways
b) Increased activity of the immune system
c) Airway Surface Liquid (ASL) too large, inhibiting airflow
d) Airway Surface Liquid (ASL) too small, impeding ciliary function
e) Excessive production of surfactant in the lungs
Answer: d) Airway Surface Liquid (ASL) too small, impeding ciliary function
Explanation: In cystic fibrosis (CF), mutations in the CFTR gene lead to the production of thick, sticky mucus in the airways. This thick mucus is due to no downregulation of Enac therefore this reduces the volume of the Airway Surface Liquid (ASL), which impairs the functioning of cilia and makes it difficult to clear mucus and pathogens from the airways. This contributes to the respiratory issues seen in individuals with CF.
a) Underproduction of mucus in the airways: Incorrect. The problem in CF is not underproduction but overproduction of thick, sticky mucus that obstructs the airways.
b) Increased activity of the immune system: Incorrect. While immune responses do occur in response to infections, the primary issue in CF is related to defective CFTR channels affecting mucus production.
c) Airway Surface Liquid (ASL) too large, inhibiting airflow: Incorrect. The issue in CF is a reduction in the volume of ASL, not an increase.
e) Excessive production of surfactant in the lungs: Incorrect. Surfactant production is not the primary issue in CF. The problem lies in the thick mucus obstructing the airways.
Question 80:
Which immune cells are primarily responsible for causing an inflammatory response in the respiratory system, especially when the system comes into contact with pathogens?
a) T cells
b) B cells
c) alveolar Macrophages
d) Neutrophils
e) Eosinophils
Answer: d) Neutrophils
Explanation: Neutrophils are the main immune cells that quickly respond to infections or pathogens in the respiratory system, initiating an inflammatory response to combat the invaders. They play a crucial role in the innate immune system’s first line of defence.
a) T cells: Incorrect. While T cells play a role in adaptive immunity, the primary cells responsible for an immediate inflammatory response are neutrophils.
b) B cells: Incorrect. B cells are involved in antibody production but are not the main drivers of the initial inflammatory response.
c) Alveolar Macrophages: Incorrect. Alveolar Macrophages play a role in phagocytosis and cytokine release in the respiratory system but are not the primary responders for acute inflammation in the respiratory system.
e) Eosinophils: Incorrect. Eosinophils are involved in allergic reactions and parasitic infections but are not the primary cells in general respiratory inflammation.
Question 81:
Which bacterial strain is a major contributor to the formation of colonies and chronic respiratory infections in individuals with Cystic Fibrosis?
a) Streptococcus pneumoniae
b) Escherichia coli
c) Pseudomonas aeruginosa
d) Staphylococcus aureus
e) Mycobacterium tuberculosis
Answer: c) Pseudomonas aeruginosa
Explanation: In individuals with Cystic Fibrosis (CF), one of the major bacterial pathogens responsible for formation within the respiratory tract and causing chronic infections is Pseudomonas aeruginosa. This bacterium’s ability to form biofilms on the airway surfaces makes it challenging to treat and contributes to lung damage and decreased lung function in CF patients.
a) Streptococcus pneumoniae: Incorrect. Streptococcus pneumoniae is a common cause of respiratory infections like pneumonia and sinusitis, but it is not the primary pathogen associated with chronic infections in Cystic Fibrosis (CF) patients.
b) Escherichia coli: Incorrect. Escherichia coli is primarily associated with gastrointestinal and urinary tract infections. It is not a major contributor to respiratory infections in Cystic Fibrosis.
d) Staphylococcus aureus: Incorrect. While Staphylococcus aureus can cause respiratory infections, especially in early CF, it is not as persistent or destructive as Pseudomonas aeruginosa in causing chronic infections in CF patients.
e) Mycobacterium tuberculosis: Incorrect. Mycobacterium tuberculosis causes tuberculosis, a serious respiratory disease, but it is not the primary pathogen associated with chronic respiratory infections in Cystic Fibrosis patients.
Question 82:
In allergic rhinitis, which plays a central role in the immune response and will be found in high levels in serum?
a) IgA
b) alveolar Macrophage
c) B lymphocytes
d) Neutrophils
e) IgE
Answer: e) IgE
Explanation: Allergic rhinitis is primarily mediated by mast cells, which release inflammatory mediators in response to the binding of allergens to IgE antibodies on their surface. While eosinophils are involved in the allergic response, mast cells are the key initiators of the allergic cascade in this condition.
a) IgA: Incorrect. IgA is primarily involved in mucosal immunity, protecting the body from pathogens at mucosal surfaces. While important in respiratory immunity, it does not play a central role in allergic rhinitis.
b) Alveolar Macrophage: Incorrect. Alveolar macrophages are key immune cells in the lungs, involved in clearing pathogens and debris, but they are not the primary mediators of allergic rhinitis.
c) B lymphocytes: Incorrect. B lymphocytes produce antibodies, including IgE, but they are not directly responsible for the allergic symptoms. The presence of IgE, rather than B cells themselves, is more relevant to allergic rhinitis.
d) Neutrophils: Incorrect. Neutrophils are primarily involved in bacterial infections and acute inflammatory responses but are not the main players in allergic rhinitis.
Question 83: In which nasal structure are olfactory sensory neurons (bipolar neurons) primarily located?
a) Sphenoethmoidal recess
b) Nasal conchae (turbinates)
c) Nasal septum
d) Nasopharynx
e) Paranasal sinuses
Answer: a) Sphenoethmoidal recess
Explanation: Olfactory sensory neurons, responsible for our sense of smell, are primarily located within the olfactory epithelium,which is located in the sphenoethmoidal recess of the nose
b) Nasal conchae (turbinates): Incorrect. The nasal conchae (turbinates) are structures within the nasal cavity that help to warm and humidify air but are not primarily associated with olfactory sensory neurons.
c) Nasal septum: Incorrect. The nasal septum divides the nasal cavity but is not the primary location for olfactory sensory neurons.
d) Nasopharynx: Incorrect. The nasopharynx is the upper part of the throat behind the nose and is involved in air passage, not olfaction.
e) Paranasal sinuses: Incorrect. The paranasal sinuses are air-filled spaces surrounding the nasal cavity but do not contain olfactory sensory neurons.
Question 84:
In oxygen transport, what factor primarily influences the release of oxygen from haemoglobin to peripheral tissues?
a) Decreased CO2
b) Higher tissue PO2 levels
c) Decreased temperature
d) Increased 2,3-DPG
e) Increased pH
Answer: d) Increased 2,3-DPG
Explanation: Elevated levels of 2,3-diphosphoglycerate (2,3-DPG) in erythrocytes promote the unloading of oxygen from haemoglobin, enhancing oxygen delivery to peripheral tissues. Factors such as increased acidity (decreased pH), elevated carbon dioxide (CO2) levels, and reduced temperature also contribute to this effect, but increased 2,3-DPG plays a significant role in optimizing oxygen release where it’s needed most in metabolically active tissues.
a) Decreased CO2: Incorrect. A decrease in carbon dioxide would generally lead to less oxygen being released from haemoglobin, not more, as it would raise the pH (Bohr effect).
b) Higher tissue PO2 levels: Incorrect. Higher oxygen levels in tissues would reduce the gradient for oxygen release from haemoglobin.
c) Decreased temperature: Incorrect. Lower temperatures stabilize the bond between oxygen and haemoglobin, reducing oxygen release.
e) Increased pH: Incorrect. An increase in pH (alkalosis) would make haemoglobin hold onto oxygen more tightly, reducing its release to tissues.
Question 85:
During the pseudoglandular stage of lung development, which structure primarily forms?
a) Bronchial tree
b) Lung lobes
c) Trachea
d) Paired cartilages
e) Respiratory Bronchioles
Answer: a) Bronchial tree
Explanation: The pseudoglandular stage of lung development primarily leads to the formation of the bronchial tree, including the branching bronchi and bronchioles. While subsequent stages of lung development involve the creation of alveoli, trachea, and other structures, the pseudoglandular stage focuses on the branching airways.
a) Decreased CO2: Incorrect. A decrease in carbon dioxide would generally lead to less oxygen being released from haemoglobin, not more, as it would raise the pH (Bohr effect).
b) Lung lobes: Incorrect. The formation of the lung lobes occurs earlier, during the embryonic stage, before the pseudoglandular stage.
c) Trachea: Incorrect. The trachea forms during the embryonic stage of lung development, prior to the pseudoglandular stage.
d) Paired cartilages: Incorrect. The paired laryngeal cartilages develop as part of the upper airway but are not the primary focus of the pseudoglandular stage.
e) Respiratory bronchioles: Incorrect. Respiratory bronchioles develop later in lung development, during the canalicular and saccular stages, when gas exchange structures begin to form.
Question 86:
If you have a gas at an initial pressure of 2 atm and you decrease its volume from 4 liters to 2 liters while keeping the temperature constant, what will happen to the pressure, according to Boyle’s Law?
a) The pressure remains at 2 atm.
b) The pressure decreases to 1 atm.
c) The pressure increases to 4 atm.
d) The pressure decreases to 0.5 atm.
e) The pressure increases to 8 atm.
Answer: c) The pressure increases to 4 atm.
Explanation: According to Boyle’s Law, when the volume of a gas is reduced while keeping the temperature constant, the pressure increases. In this case, the initial pressure was 2 atm, and when the volume is reduced by half, the pressure doubles, reaching 4 atm.
a) The pressure remains at 2 atm (Incorrect) – Boyle’s Law states that pressure and volume are inversely related, so pressure cannot stay the same if the volume decreases.
b) The pressure decreases to 1 atm (Incorrect) – This would happen if the volume were doubled, not halved.
d) The pressure decreases to 0.5 atm (Incorrect) – Pressure decreases when volume increases, not when volume decreases.
e) The pressure increases to 8 atm (Incorrect) – Doubling the pressure would result in 4 atm, not 8 atm.
Question 87:
At which vertebral level does the trachea bifurcate into the left and right main bronchi?
a) T3
b) T4
c) T5
d) T6
e) T7
Answer: b) T4
Explanation: The trachea bifurcates at the level of the sternal angle (angle of Louis), which is usually at the level of the second costal cartilage, corresponding to vertebral level T4.
a) T3 (Incorrect) – The tracheal bifurcation occurs at T4, not at T3.
c) T5 (Incorrect) – T5 is slightly below the bifurcation point.
d) T6 (Incorrect) – The bifurcation occurs higher, at T4, not T6.
e) T7 (Incorrect) – T7 is too low for the tracheal bifurcation.
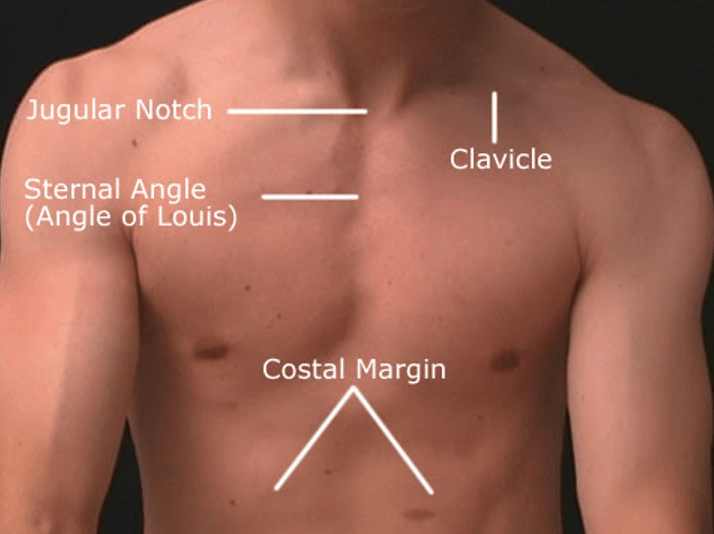
Question 88:
What makes up the posterior border of the trachea?
a) Nucleus pulposus
b) Cricotracheal ligament
c) Laryngopharynx
d) Arytenoid muscle
e) Trachealis
Answer: e) Trachealis muscle
Explanation: The posterior border of the trachea is formed by the trachealis muscle, which connects the ends of the tracheal cartilage rings and allows for adjustments in tracheal diameter during swallowing (as the oesophagus expands) and other activities.
a) Nucleus pulposus (Incorrect) – This is part of the intervertebral discs, not related to the trachea. This functions as a shock absorber.
b) Cricotracheal ligament (Incorrect) – This ligament connects the cricoid cartilage to the trachea but does not form its posterior border.
c) Laryngopharynx (Incorrect) – The laryngopharynx is part of the throat, not the posterior tracheal border.
d) Arytenoid muscle (Incorrect) – The arytenoid muscles are involved in vocal cord movement, not the structure of the trachea.
Question 89:
In the trachea, what shape do the cartilage rings typically have?
a) O-shaped
b) Oval
c) C-shaped
d) Spiral
e) Helix
Answer: c) C-shaped
Explanation: The cartilage rings in the trachea are C-shaped, with the open ends of the rings facing posteriorly. This shape helps maintain the tracheal structure while allowing flexibility for swallowing and other movements.
a) O-shaped (Incorrect) – Tracheal rings are open at the back and covered by the trachealis muscle, making them C-shaped, not O-shaped.
b) Oval (Incorrect) – The rings are not oval but C-shaped with an open posterior part.
d) Spiral (Incorrect) – Tracheal rings are not spiral; they are C-shaped.
e) Helix (Incorrect) – Tracheal cartilage does not form a helical structure.
Question 90:
In the respiratory zone of the lungs, where does the first part of this zone begin?
a) Respiratory bronchioles
b) Terminal bronchioles
c) Tertiary bronchi
d) Alveolar sacs
e) Trachea
Answer: a) Respiratory bronchioles
Explanation: The respiratory zone of the lungs begins with the respiratory bronchioles. This is where the exchange of oxygen and carbon dioxide occurs within the alveoli, making it a critical part of the respiratory system.
b) Terminal bronchioles (Incorrect) – Terminal bronchioles are part of the conducting zone, not the respiratory zone.
c) Tertiary bronchi (Incorrect) – These are also part of the conducting airways and don’t contribute to gas exchange.
d) Alveolar sacs (Incorrect) – Alveolar sacs are part of the respiratory zone but are not the first structures; respiratory bronchioles come first.
e) Trachea (Incorrect) – The trachea is part of the conducting zone, not the respiratory zone.
Question 91:
Which part of the brain primarily controls voluntary breathing?
a) Cerebellum
b) Pons
c) Cerebral cortex
d) DRG of medulla oblongata
e) VRG of medulla oblongata
Answer: c) Cerebral cortex
Explanation: The voluntary control of breathing, especially during activities like speaking, singing, or breath-holding, is primarily associated with the cerebral cortex, particularly the motor cortex in the frontal lobe. While the brainstem, medulla oblongata, and other brain regions play crucial roles in automatic or involuntary breathing, voluntary control is governed by the cerebral cortex.
a) Cerebellum (Incorrect) – The cerebellum is involved in motor control and coordination but not in controlling breathing.
b) Pons (Incorrect) – The Pons which contain the apneustic and pneumotaxic centre are responsible for fine tuning of breathing.
d) DRG of medulla oblongata (Incorrect) – The dorsal respiratory group controls involuntary passive inhalation and exhalation but also forced inspiration, not voluntary.
e) VRG of medulla oblongata (Incorrect) – The ventral respiratory group also controls involuntary forced inhalation and exhalation, not voluntary.
Question 92:
During a 5-kilometer (5K) race, which muscles are primarily engaged during expiration (exhalation)?
a) Diaphragm and external intercostal muscles
b) Diaphragm and scalene muscles
c) Rectus abdominis and external intercostal muscles
d) Rectus abdominis and internal intercostal muscles
e) Transversus abdominis and serratus anterior muscles
Answer: d) Rectus abdominis and internal intercostal muscles
Explanation: During vigorous physical activities like a 5K race, active expiration is aided by the contraction of the rectus abdominis muscles, which compress the abdominal contents, and the internal intercostal muscles, which help lower the ribcage. These muscles work together to facilitate forceful exhalation and assist in expelling air from the lungs, helping the athlete maintain a steady breathing rhythm.
a) Diaphragm and external intercostal muscles — Incorrect: The diaphragm is primarily involved in inspiration (inhalation), and the external intercostal muscles assist in lifting the rib cage during inhalation, not forced expiration.
b) Diaphragm and scalene muscles — Incorrect: The diaphragm and scalene muscles are both involved in inspiration, with the scalene muscles elevating the first and second ribs to help expand the chest in forced inspiration.
c) Rectus abdominis and external intercostal muscles — Incorrect: The rectus abdominis is involved in expiration, but the external intercostal muscles are active in inspiration.
e) Transversus abdominis and serratus anterior muscles — Incorrect: While the transversus abdominis contributes to forced expiration, the serratus anterior primarily assists in arm movements and forced inhalation.
Question 93:
Which lung volume represents the maximum amount of air a person can exhale after taking the deepest breath possible?
a) Inspiratory Reserve Volume (IRV)
b) Expiratory Reserve Volume (ERV)
c) Vital Capacity (VC)
d) Residual Volume (RV)
e) Total Lung Capacity (TLC)
Answer: c) Vital Capacity (VC) (4800 ml)
Explanation: Vital Capacity (VC) is the maximum amount of air a person can exhale after taking the deepest breath possible. It includes tidal volume, inspiratory reserve volume, and expiratory reserve volume.
a) Inspiratory Reserve Volume (IRV) — Incorrect: IRV refers to the extra volume of air you can inhale after a normal inhalation, not exhalation. (2400ml)
b) Expiratory Reserve Volume (ERV) — Incorrect: ERV is the extra volume of air that can be forcefully exhaled after a normal exhalation, but it doesn’t account for the total volume exhaled after a deep breath. (1200ml)
d) Residual Volume (RV) — Incorrect: RV refers to the air remaining in the lungs after a forceful exhalation (1200ml)
e) Total Lung Capacity (TLC) — Incorrect: TLC is the total volume of the lungs, including both inhaled air and the residual volume (6000ml)
Question 94:
Which respiratory muscle primarily assists with forced expiration during activities like coughing or sneezing?
a) Diaphragm
b) External intercostal muscles
c) Internal intercostal muscles
d) Sternocleidomastoid
e) Scalene muscles
Answer: c) Internal intercostal muscles
Explanation: The internal intercostal muscles assist with forced expiration during activities that require increased expiratory effort, such as coughing or sneezing.
a) Diaphragm — Incorrect: The diaphragm contrtacts and flattens in inhalation, not forced expiration. b)External intercostal muscles — Incorrect: These muscles assist with inspiration by elevating the ribs, not with expiration. d) Sternocleidomastoid — Incorrect: This muscle assists with forced inhalation, not expiration. e) Scalene muscles — Incorrect: These muscles are involved in lifting the ribs during forced inhalation, not in expiration.
Question 95:
Which gas law describes the relationship between the pressure and volume of a gas while keeping the temperature constant?
a) Charles’s Law
b) Boyle’s Law
c) Dalton’s Law
d) Avogadro’s Law
e) Graham’s Law
Answer: b) Boyle’s Law
Explanation: Boyle’s Law states that the pressure of a gas is inversely proportional to its volume when temperature is held constant.
a) Charles’s Law — Incorrect: Charles’s Law describes the relationship between temperature and volume, not pressure and volume.
c) Dalton’s Law — Incorrect: Dalton’s Law pertains to the partial pressures of gases in a mixture, not the pressure-volume relationship.
d) Avogadro’s Law — Incorrect: Avogadro’s Law relates to the volume of gas and the number of gas molecules, not pressure and volume.
e) Graham’s Law — Incorrect: Graham’s Law deals with the rate of gas diffusion, not pressure and volume.
Question 96:
During an asthma attack, which of the following physiological changes occurs in the airways?
a) Bronchoconstriction
b) Increased compliance
c) Decreased mucus production
d) Lower airway resistance
e) Increased functional residual capacity (FRC)
Answer: a) Bronchoconstriction
Explanation: During an asthma attack, the smooth muscle in the bronchioles contracts, causing bronchoconstriction and narrowing of the airways, which leads to increased airway resistance and breathing difficulties.
b) Increased compliance — Incorrect: Compliance refers to the ability of the lungs to stretch; during asthma, airway resistance increases, but compliance generally decreases.
c) Decreased mucus production — Incorrect: During asthma, mucus production often increases, contributing to airway blockage.
d) Lower airway resistance — Incorrect: Airway resistance increases during an asthma attack due to airway narrowing.
e) Increased functional residual capacity (FRC) — Incorrect: FRC is typically reduced or unaffected during an asthma attack
Question 97:
Which of the following best represents the primary function of the pneumotaxic centre in the pons?
a) Initiating inspiration
b) Regulating the depth of breathing
c) Adjusting respiratory rate based on blood oxygen levels
d) Fine-tuning respiratory rhythm by inhibiting the inspiratory centre
e) Stimulates the inspiratory centre (DRG)
Answer: d) Fine-tuning respiratory rhythm by inhibiting the inspiratory centre
Explanation: The pneumotaxic centre in the upper pons fine-tunes the respiratory rhythm by inhibiting the inspiratory centre (dorsal respiratory group) in the medulla and the Apneustic centre, helping to prevent overinflation of the lungs during inspiration whilst causing shorter and shallower breaths.
a) Initiating inspiration — Incorrect: The pneumotaxic centre does not initiate inspiration; this function is primarily controlled by the dorsal respiratory group.
b) Regulating the depth of breathing — Incorrect: The pneumotaxic centre influences the duration, not the depth of breathing.
c) Adjusting respiratory rate based on blood oxygen levels — Incorrect: Blood oxygen levels affect the chemoreceptors that influence the medulla, not directly the pneumotaxic centre.
e) Stimulates the inspiratory centre (DRG) — Incorrect: The pneumotaxic centre inhibits, not stimulates, the inspiratory centre. This is the role of the Apneustic centre to allow for deeper and longer breaths.
Question 98:
Which type of pneumocyte is primarily responsible for producing pulmonary surfactant in the alveoli?
a) Type I pneumocyte
b) Type II pneumocyte
c) Type III pneumocyte
d) Type A pneumocyte
e) Type B pneumocyte
Answer: b) Type II pneumocyte
Explanation: Type II pneumocytes, also known as great alveolar cells, are cuboidal cells responsible for producing and secreting pulmonary surfactant, a substance that reduces surface tension in the alveoli and prevents their collapse.
a) Type I pneumocyte — Incorrect: Type I pneumocytes are involved in gas exchange, not surfactant production.
c) Type III pneumocyte — Incorrect: There is no Type III pneumocyte; this is a distractor option.
d) Type A pneumocyte — Incorrect: This is not a recognized classification of alveolar cells.
e) Type B pneumocyte — Incorrect: Similar to “Type A,” this is not a valid classification.
Question 99:
Which of the following factors contributes to increased airway resistance?
a) Decreased mucus production
b) Bronchoconstriction
c) Reduced airway inflammation
d) Increased alveolar surface area
e) Normal responsiveness of smooth muscle
Answer: b) Bronchoconstriction
Explanation: Bronchoconstriction (narrowing of the airways) is a key factor contributing to increased airway resistance, leading to airflow limitation and respiratory symptoms.
a) Decreased mucus production — Incorrect: Increased, not decreased, mucus production would contribute to airway resistance.
c) Reduced airway inflammation — Incorrect: Reduced inflammation would lower, not increase, airway resistance.
d) Increased alveolar surface area — Incorrect: Increased surface area improves gas exchange but does not affect airway resistance.
e) Normal responsiveness of smooth muscle — Incorrect: Increased or abnormal responsiveness, not normal, would contribute to higher airway resistance.
Question 100:
Which of the following statements best describes the function of type I pneumocytes in the alveoli?
a) Secretion of pulmonary surfactant
b) Production of mucus to trap foreign particles
c) Gas exchange, facilitating oxygen uptake and carbon dioxide removal
d) Proliferation and repair of alveolar tissue
e) Detoxification of harmful substances
Answer: c) Gas exchange, facilitating oxygen uptake and carbon dioxide removal
Explanation: Type I pneumocytes are specialized for gas exchange. They have thin, squamous cell membranes that allow for efficient diffusion of oxygen into the bloodstream and removal of carbon dioxide from the bloodstream.
a) Secretion of pulmonary surfactant — Incorrect: This function is carried out by Type II pneumocytes, not Type I.
b) Production of mucus to trap foreign particles — Incorrect: Mucus production occurs in the bronchi, not the alveoli, and is not related to Type I pneumocytes.
d) Proliferation and repair of alveolar tissue — Incorrect: Type II pneumocytes are responsible for alveolar repair, not Type I.
e) Detoxification of harmful substances — Incorrect: This is a function of alveolar macrophages, not pneumocytes.
Question 101:
What is the main function of the cilia lining the respiratory tract?
a) Gas exchange
b) Filtration of air
c) Production of mucus
d) Secretion of hormones
e) Thermoregulation
Answer: b) Filtration of air
Explanation: The main function of the cilia lining the respiratory tract is to filter inhaled air by trapping dust, debris, and microorganisms in the mucus they produce and move out of the respiratory passages.
a) Gas exchange — Incorrect: Gas exchange occurs in the alveoli, not via the cilia.
c) Production of mucus — Incorrect: Goblet cells and glands produce mucus, not the cilia.
d) Secretion of hormones — Incorrect: Cilia do not secrete hormones; this is a function of endocrine glands.
e) Thermoregulation — Incorrect: Cilia do not regulate temperature; they help clear mucus and trapped particles from the airways.
Question 102:
Which lymphatic duct drains lymph from the left upper limb and the entire lower body?
a) Right lymphatic duct
b) Thoracic duct
c) Subclavian duct
d) Cisterna chyli
e) Lumbar duct
Answer: b) Thoracic duct
Explanation: The thoracic duct is the largest lymphatic vessel in the human body. It is responsible for draining lymph from various regions (basically all the body apart from the upper right side of the body), including the left upper limb and the entire lower body. This duct plays a significant role in returning lymph, which carries waste products and excess fluid, back into the bloodstream.
a) Right lymphatic duct — Incorrect: The right lymphatic duct only drains lymph from the right upper limb, right side of the head, and right thorax, not the left upper limb or lower body.
c) Subclavian duct — Incorrect: The subclavian ducts do not exist; this is a distractor. Lymph from the thoracic duct empties into the subclavian vein.
d) Cisterna chyli — Incorrect: The cisterna chyli is a dilation at the lower end of the thoracic duct, but it is not a duct itself. This serves as a collecting point for the lymph of the lower body.
e) Lumbar duct — Incorrect: The lumbar ducts are part of the lymphatic system but drain into the cisterna chyli, not directly into the bloodstream.

Question 103:
Where does the azygous vein primarily drain into?
a) Brachiocephalic trunk
b) Pulmonary artery
c) Right atrium
d) Superior vena cava (SVC)
e) Pulmonary vein
Answer: d) Superior vena cava (SVC)
Explanation:
The azygos vein primarily drains into the superior vena cava (SVC), which is a large vein that carries deoxygenated blood from the upper half of the body to the right atrium of the heart. This drainage plays a crucial role in the venous circulation of the upper body.
a) Brachiocephalic trunk — Incorrect: The brachiocephalic trunk is an artery, not a vein, and it does not receive blood from the azygous vein.
b) Pulmonary artery — Incorrect: The pulmonary artery carries deoxygenated blood from the heart to the lungs and does not connect to the azygous system.
c) Right atrium — Incorrect: whilst indirectly it doesn’t drain into the right atria. The azygos vein does not directly drain into the right atrium; instead, it drains into the superior vena cava, which leads to the right atrium.
e) Pulmonary vein — Incorrect: The pulmonary veins carry oxygenated blood from the lungs to the left atrium and are not involved in systemic venous drainage.
Question 104:
What is the primary function of the thymus gland?
a) Production of respiratory enzymes
b) Regulation of bicarbonate levels
c) Maturation of T lymphocytes (T cells)
d) Production of T lymphocytes
e) Filtration of blood cells
Answer: c) Maturation of T lymphocytes (T cells)
Explanation: The thymus gland plays a crucial role in the immune system. Its primary function is to facilitate the maturation and development of T lymphocytes (T cells), which are essential for cell-mediated immunity and the immune response to infections and foreign substances in the body.
a) Production of respiratory enzymes — Incorrect: The thymus gland is not involved in the production of respiratory enzymes.
b) Regulation of bicarbonate levels — Incorrect: Bicarbonate regulation is related to renal and respiratory functions, not the thymus gland.
d) Production of T lymphocytes— Incorrect: whilst the Thymus plays a crucial role regarding T cells, however T cells are formed in the bone marrow then travel to the thymus to mature
e) Filtration of blood cells — Incorrect: Blood cell filtration occurs primarily in the spleen, not the thymus.
Question 105:
Among the following structures, which is the most anterior in the mediastinum?
a) Trachea
b) Oesophagus
c) Aorta
d) Brachiocephalic artery
e) Common carotid artery
Answer: a) Trachea
Explanation: In the mediastinum, the trachea is the most anterior structure, followed by the brachiocephalic artery, common carotid artery, aorta, and the oesophagus, which is the most posterior of the options provided.
b) Oesophagus — Incorrect: The oesophagus is posterior to the trachea in the mediastinum. c) Aorta — Incorrect: The aorta lies posterior to the trachea. d) Brachiocephalic artery — Incorrect: Although the brachiocephalic artery is anterior to the aorta, it is still posterior to the trachea. e) Common carotid artery — Incorrect: The common carotid artery is posterior to the trachea.
Question 106:
At which spinal level does the aorta pass through the diaphragm via the aortic hiatus?
a) T6
b) T8
c) T10
d) T12
e) L2
Answer: d) T12
Explanation: The aorta and cisterna chyli (this has 12 letters hence T12) passes through the diaphragm at the level of the 12th thoracic vertebra (T12) via the aortic hiatus, which is situated anteriorly and slightly to the left. Oesophagus passes through T10, (oesophagus has 10 letters) inferior Vena cava enters through T8 ( Vena cava has 8 letters)
a) T6 — Incorrect: T6 is too high in the thoracic spine; the aorta does not pass through the diaphragm at this level.
b) T8 — Incorrect: The inferior vena cava passes through the diaphragm at T8, not the aorta.
c) T10 — Incorrect: The oesophagus passes through the diaphragm at T10, not the aorta.
e) L2 — Incorrect: L2 is in the lumbar spine, below the level where the aorta passes through the diaphragm.
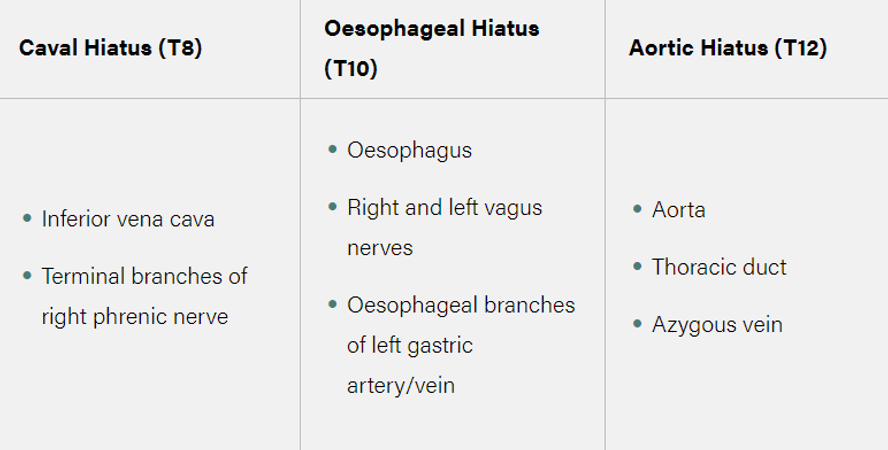
Question 107:
In relation to the lung hilum, the phrenic nerve passes:
a) Posterior
b) Anterior
c) Superior
d) Inferior
e) Medial
Answer: b) Anterior
Explanation: The phrenic nerve passes anterior to the lung hilum as it travels downward to innervate the diaphragm. This nerve controls the contraction of the diaphragm, a crucial muscle involved in breathing.
a) Posterior — Incorrect: The vagus nerve passes posterior to the hilum, not the phrenic nerve.
c) Superior — Incorrect: The phrenic nerve does not pass superior to the lung hilum; it runs anterior to it.
d) Inferior — Incorrect: The phrenic nerve does not pass inferior to the hilum.
e) Medial — Incorrect: The phrenic nerve does not run medially to the lung hilum.
Question 108:
Which statement accurately describes the innervation of the larynx by the recurrent laryngeal nerve?
a) The recurrent laryngeal nerve innervates the cricothyroid muscle exclusively.
b) It provides motor innervation to all intrinsic laryngeal muscles and sensory innervation to the mucous membrane below the vocal cords.
c) The recurrent laryngeal nerve only innervates the vocal cords.
d) It supplies sensory fibres to the epiglottis and motor fibres to the diaphragm.
e) None of the above.
Answer: b) It provides motor innervation to all intrinsic laryngeal muscles and sensory innervation below the vocal cords.
Explanation: The recurrent laryngeal nerve plays a crucial role in laryngeal innervation. It provides motor innervation to all intrinsic laryngeal muscles except the cricothyroid muscle and supplies sensory fibres to the mucous membrane below the vocal cords.
a) The recurrent laryngeal nerve innervates the cricothyroid muscle exclusively. — Incorrect: The cricothyroid muscle is innervated by the external branch of the superior laryngeal nerve, not the recurrent laryngeal nerve. c) The recurrent laryngeal nerve only innervates the vocal cords. — Incorrect: The recurrent laryngeal nerve innervates more than just the vocal cords; it supplies all intrinsic laryngeal muscles except the cricothyroid. d) It supplies sensory fibres to the epiglottis and motor fibres to the diaphragm. — Incorrect: The recurrent laryngeal nerve does not innervate the diaphragm or the epiglottis. e)None of the above. — Incorrect: Option B is correct.
Question 109:
Which nerve innervates the cricothyroid muscle?
a) Recurrent laryngeal nerve
b) Vagus nerve
c) Glossopharyngeal nerve
d) Internal branch of superior laryngeal nerve
e) External branch of the superior laryngeal nerve
Answer: e) External branch of the superior laryngeal nerve
Explanation: The cricothyroid muscle is primarily innervated by the external branch of the superior laryngeal nerve. This nerve is a branch of the vagus nerve (cranial nerve X) and plays a crucial role in controlling the tension of the vocal cords
a) Recurrent laryngeal nerve — Incorrect: The recurrent laryngeal nerve innervates all intrinsic laryngeal muscles except the cricothyroid.
b) Vagus nerve — Incorrect: While the vagus nerve gives rise to the superior laryngeal nerve, it does not directly innervate the cricothyroid muscle.
c) Glossopharyngeal nerve — Incorrect: The glossopharyngeal nerve is involved in taste and sensation in the throat but does not innervate the cricothyroid muscle.
d) Internal branch of superior laryngeal nerve — Incorrect: The internal branch provides sensory innervation above the vocal cords but does not innervate the cricothyroid muscle.
Question 110:
What type of epithelium lines the trachea?
a) Simple squamous
b) Pseudostratified Cuboidal
c) Pseudostratified columnar
d) Simple cuboidal
e) Transitional epithelium
Answer: c) Pseudostratified columnar
Explanation: The trachea is lined with pseudostratified ciliated columnar epithelium, which helps trap and move mucus and debris away from the lungs due to the presence of cilia on the cells’ surfaces. This epithelial type is well-suited for the respiratory tract’s functions.
a) Simple squamous — Incorrect: Simple squamous epithelium lines structures involved in gas exchange, like the alveoli, not the trachea. b) Pseudostratified cuboidal — Incorrect: The trachea is not lined by cuboidal epithelium; it has columnar cells. d) Simple cuboidal — Incorrect: This type of epithelium lines smaller bronchioles, not the trachea. e) Transitional epithelium — Incorrect: Transitional epithelium is found in the urinary bladder, not the respiratory tract.
Question 111) A 67-year-old man with COPD is evaluated for a lung transplant. Which of the following tests would best evaluate his respiratory muscle function?
A) Tidal volume
B) Forced expiratory volume
C) Maximal inspiratory pressure
D) Total lung capacity
E) Diffusing capacity of the lungs
Answer: C) Maximal inspiratory pressure
Explanation: Maximal inspiratory and expiratory pressures measured at the mouth reflect respiratory muscle strength and endurance. Tidal volume, forced expiratory volume, total lung capacity, and diffusing capacity do not directly measure respiratory muscle function. Maximal inspiratory pressure is typically the most affected in COPD patients.
a) Tidal volume — Incorrect: Tidal volume measures the amount of air inhaled and exhaled during a normal breath but does not specifically evaluate respiratory muscle strength. (500ml)
b) Forced expiratory volume — Incorrect: Forced expiratory volume assesses airflow and lung function but does not provide direct information about respiratory muscle strength. (1200ml)
d) Total lung capacity — Incorrect: Total lung capacity measures the maximum volume of air in the lungs, but it doesn’t directly assess respiratory muscle strength.(6000ml)
e) Diffusing capacity of the lungs — Incorrect: Diffusing capacity evaluates the ability of gases to move across the alveolar-capillary membrane, not muscle function.
Question 112) A 60-year-old man undergoes a bronchoscopy and biopsy of a lung nodule. The procedure irritates the airway and triggers coughing. Which of the following best describes the physical mechanism of coughing?
A) Activation of stretch receptors in the airway
B) Stimulation of the pharyngeal reflex
C) Irritation of nerves in the larynx
D) Phrenic nerve irritation
E) Disruption of surfactant in the alveoli
Answer: C) Irritation of nerves in the larynx
Explanation: Coughing is triggered by stimulation of sensory nerves in and below the larynx, which leads to a reflex contraction of expiratory muscles and opening of the glottis. Stretch receptors and the pharyngeal reflex modulate but do not initiate cough. Inflammation of bronchioles and disruption of alveolar surfactant do not directly stimulate cough receptors.
A) Activation of stretch receptors in the airway — Incorrect: While stretch receptors in the airway play a role in regulating breathing, they do not directly trigger coughing. B) Stimulation of the pharyngeal reflex— Incorrect: The pharyngeal reflex is related to swallowing and gagging, not coughing. D) Phrenic nerve irritation — Incorrect: The phrenic nerve controls the diaphragm, and its irritation causes hiccups, not cough. E) Disruption of surfactant in the alveoli — Incorrect: Surfactant issues are related to lung compliance and respiratory distress, not coughing.
Question 113) A 6-year-old girl presents with recurrent sinus infections and frequent colds. Testing identifies a rare genetic defect impairing ciliary function in her airway epithelial cells. This will primarily affect which normal lung defense mechanism?
A) Mucus secretion
B) Alveolar macrophage function
C) Cough reflex sensitivity
D) Mucociliary clearance
E) IgA production
Answer: D) Mucociliary clearance
Explanation: Mucociliary clearance depends on beating cilia to transport mucus. Defects in ciliary structure or function impair mucociliary clearance and predispose to recurrent airway infections, while leaving other defense mechanisms intact. Mucus secretion, macrophage function, cough reflex, and IgA levels are not directly affected.
A) Mucus secretion — Incorrect: Mucus secretion itself is not directly affected by ciliary dysfunction. B)Alveolar macrophage function — Incorrect: Macrophage function is independent of ciliary activity. C)Cough reflex sensitivity — Incorrect: The cough reflex does not directly depend on ciliary function. E) IgA production — Incorrect: IgA production is part of the immune system and is not affected by ciliary function.
Question 114) A 45-year-old woman with cystic fibrosis has progression of her lung disease. Which of the following airway surface liquid abnormalities contributes most to her recurrent infections?
A) Increased mucus secretion
B) Impaired chloride transport
C) Decreased pH
D) Abnormal sodium absorption
E) Decreased bicarbonate secretion
Answer: B) Impaired chloride transport
Explanation: The hallmark airway defect in cystic fibrosis is mutated CFTR, which impairs chloride transport across respiratory epithelium. This leads to dehydration and acidification of airway surface liquid. Impaired mucociliary clearance allows mucus stasis and bacterial colonization. The other options may occur in CF but are secondary effects.
A) Increased mucus secretion — Incorrect: In CF it is the opposite as the mucus becomes sticky and thick as more water leves it due to increased chloride transport into the epithelial cells.
C) Decreased pH — Incorrect: pH changes are secondary effects in CF but not the primary cause.
D) Abnormal sodium absorption — Incorrect: Abnormal sodium absorption occurs in CF, but it is secondary to chloride transport issues.
E) Decreased bicarbonate secretion — Incorrect: Decreased bicarbonate secretion is a related feature but not the main abnormality causing infections.
Question 115) A 45-year-old woman comes to the clinic with a 2-week history of progressive shortness of breath, cough, and wheezing. She is diagnosed with pneumonia. Which of the following cells is most important for clearing this bacterial lung infection at first interaction?
A) Helper T cells
B) Cytotoxic T cells
C) Regulatory T cells
D) Alveolar macrophages
E) Neutrophils
Answer: E) Neutrophils
Explanation: Neutrophils are critical effector cells of the innate immune system that phagocytose and kill extracellular bacteria like pneumonia-causing species. Alveolar macrophages also participate but to a lesser degree. The adaptive immune T cells listed play no direct role in initial bacterial clearance.
A) Helper T cells — Incorrect: Helper T cells are part of the adaptive immune system, which responds later in infections.
B) Cytotoxic T cells — Incorrect: Cytotoxic T cells target virus-infected or cancerous cells, not bacteria.
C) Regulatory T cells — Incorrect: Regulatory T cells modulate immune responses but are not directly involved in bacterial clearance.
D) Alveolar macrophages — Incorrect: Although important, macrophages play a secondary role to neutrophils at first site of bacterial infections.
Question 116) A 6-year-old boy has frequent bouts of wheezing, cough, and respiratory infections. Testing shows elevated IgE and eosinophilia. Which cells are most likely participating in the pathologic immune response in his airways?
A) Mast cells
B) Neutrophils
C) Macrophages
D) B lymphocytes
E) Natural killer cells
Answer: A) Mast cells
Explanation: The clinical history and findings suggest allergic asthma, in which mast cells activated by IgE release inflammatory mediators contributing to airway hyperreactivity, mucus secretion, and bronchoconstriction. Eosinophils may also be involved but mast cells are the central effectors.
B) Neutrophils — Incorrect: Neutrophils are primarily involved in bacterial infections and inflammation, not allergic asthma.
C) Macrophages — Incorrect: Macrophages play a role in immune defense but are not central to allergic asthma.
D) B lymphocytes — Incorrect: B cells produce antibodies but are not the key cells in this allergic response.
E) Natural killer cells — Incorrect: NK cells target virus-infected cells and tumors, not asthma-related inflammation.
Question 117) A 67-year-old man with 50 pack-years of smoking is found to have lung carcinoma. Which immune deficiency likely contributed most to his risk of developing lung cancer?
A) Reduced mucosal IgA
B) Impaired macrophage function
C) Loss of TLR signaling
D) Defective T cell responses
E) Lower complement activity
Answer: A) Reduced mucosal IgA
Explanation: Smoking impairs production of secretory IgA, an important immunoglobulin in mucosal immunity of the airways. This contributes to bacterial colonization, chronic inflammation, and reduced clearance of carcinogens. The other options may occur but play less direct roles in lung cancer risk.
B) Impaired macrophage function — Incorrect: Macrophage impairment can contribute to infections but is less directly related to cancer risk.
C) Loss of TLR signaling — Incorrect: Toll Like Receptors signalling is responsible for activating the immune response as it recognises pathogens but also bridges the innate immunity to the adaptive immunity.This works by the TLR detecting pathogen-associated molecular patterns (PAMPs) (e.g. antigens).
D) Defective T cell responses — Incorrect: While T cells are important for cancer surveillance, reduced IgA is more directly related to carcinogen clearance.
E) Lower complement activity — Incorrect: The complement system is not directly related to lung cancer risk in smokers.
Question 118) A newborn baby girl delivered at 35 weeks gestation develops significant respiratory distress shortly after birth. Chest x-ray shows diffuse reticulogranular opacities. She likely has deficiency of which of the following?
A) Laminin
B) Surfactant
C) Clara cells
D) Alveolar macrophages
E) Mucociliary escalator
Answer: B) Surfactant
Explanation: Surfactant production by type 2 alveolar cells dramatically increases late in gestation. Premature infants often lack adequate surfactant, leading to collapse of unstable alveoli and respiratory distress syndrome. Laminin deficiency causes disrupted lung morphogenesis. Defects of Clara cells, macrophages, and the mucociliary escalator do not cause neonatal respiratory distress.
A) Laminin — Incorrect: Laminin defects affect tissue structure but are not the primary cause of neonatal respiratory distress.
C) Clara cells — Incorrect: Clara cells produce surfactant proteins, but a general Clara cell defect is not the main issue here.
D) Alveolar macrophages — Incorrect: Macrophage deficiencies cause immune problems but do not explain respiratory distress in a premature infant.
E) Mucociliary escalator — Incorrect: The mucociliary escalator is involved in airway defense but does not cause neonatal respiratory distress syndrome.
Question 119) A newborn baby girl has a complex congenital heart defect. Prenatal ultrasound at 18 weeks gestation showed normal lung development. This suggests normal formation of which of the following embryonic lung structures?
A) Tracheoesophageal septum
B) Pleuroperitoneal canals
C) Lung buds
D) Primary bronchi
E) Secondary bronchi
Answer: C) Lung buds
Explanation: During the pseudoglandular stage at 4-17 weeks gestation, lung buds form and branch from the primitive foregut. Normal formation on ultrasound rules out major defects in early lung morphogenesis. The other structures develop after 17 weeks.
A) Tracheoesophageal septum — Incorrect. This structure divides the trachea and esophagus early in development, and major defects would have been visible earlier than 18 weeks.
B) Pleuroperitoneal canals — Incorrect. These form the diaphragm, and defects here would lead to conditions like diaphragmatic hernia, not lung developmental abnormalities.
D) Primary bronchi — Incorrect. The primary bronchi develop later, after the lung buds have formed, and would not have been the focus of an 18-week scan.
E) Secondary bronchi — Incorrect. Secondary bronchi develop even later, and while important, their normal development would not have been indicated at this stage of pregnancy.
Question 120) A baby boy born at 30 weeks gestation develops neonatal respiratory distress syndrome. He likely has deficiency in production of which of the following lung proteins?
A) Mucin
B) Tubulin
C) Cadherin
D) Surfactant protein B
E) Antiprotease
Answer: D) Surfactant protein B
Explanation: Surfactant protein B production increases dramatically late in gestation and is critical for reducing alveolar surface tension. Preterm infants often lack adequate surfactant protein B, leading to neonatal RDS. The other proteins listed are not directly involved in lung maturation.
A) Mucin — Incorrect. Mucin is a component of mucus and plays no direct role in preventing alveolar collapse, which is the cause of respiratory distress syndrome.
B) Tubulin — Incorrect. Tubulin is a structural protein involved in cilia movement, not surfactant production or lung maturation.
C) Cadherin — Incorrect. Cadherin is involved in cell adhesion, not surfactant production or lung function in premature infants.
E) Antiprotease — Incorrect. Antiproteases protect the lungs from enzymatic damage by neutralising proteases, but they do not influence surfactant production, which is critical in preventing alveolar collapse in preterm infants.
Question 121) A 6-month-old infant presents with failure to thrive and respiratory distress. Chest x-ray shows diffuse pulmonary infiltrates. Lung biopsy reveals abnormal type II alveolar cells lacking lamellar bodies. This infant likely has deficient production of which substance?
A) Mucin
B) Surfactant
C) Antiprotease
D) Interleukin-1
E) Complement
Answer: B) Surfactant
Explanation: Lamellar bodies in type II alveolar cells contain and store surfactant. Absence of lamellar bodies indicates impaired surfactant production, leading to infant respiratory distress syndrome. Mucin, antiprotease, interleukin-1, and complement are not stored in lamellar bodies.
A) Mucin — Incorrect. Mucin is involved in forming mucus and does not play a role in surfactant production or the function of type II alveolar cells, which are responsible for producing surfactant in the lungs.
C) Antiprotease — Incorrect. Antiproteases prevent enzymatic damage to lung tissue but are not related to the production of surfactant or the functionality of type II alveolar cells.
D) Interleukin-1 — Incorrect. Interleukin-1 is a cytokine involved in the immune response and inflammation, not surfactant production. The infant’s respiratory issues are related to insufficient surfactant, not an immune response.
E) Complement — Incorrect. Complement proteins are part of the immune system and assist in pathogen elimination. They do not play a role in surfactant production or in the function of type II alveolar cells, which are deficient in this case.
Question 122) A 50-year-old smoker is diagnosed with emphysema. Which of the following gas exchange abnormalities is his primary functional impairment?
A) Ventilation-perfusion mismatch
B) Diffusion limitation
C) Shunting
D) Low inspired pO2
E) Reduced haemoglobin affinity
Answer: B) Diffusion limitation
Explanation: In emphysema, destruction of alveolar walls reduces the surface area for gas exchange, impairing diffusion. Ventilation-perfusion mismatches and shunting do not occur. The patient still inhales normal pO2. Oxygen affinity of haemoglobin is unchanged.
A) Ventilation-perfusion mismatch — Incorrect. While emphysema can lead to ventilation-perfusion mismatch, it is not the primary impairment. The main problem in emphysema is the destruction of alveolar walls, which directly affects diffusion rather than ventilation-perfusion.
C) Shunting — Incorrect. Shunting occurs when blood bypasses the alveoli and is not oxygenated, which is not the primary issue in emphysema. In emphysema, alveolar walls are destroyed, impacting gas diffusion rather than creating significant shunting.
D) Low inspired pO2 — Incorrect. The partial pressure of inspired oxygen (pO2) is not reduced in patients with emphysema. The issue is the reduced ability of damaged alveoli to facilitate gas exchange, not the oxygen level in the air.
E) Reduced haemoglobin affinity — Incorrect. Hemoglobin affinity for oxygen is unaffected in emphysema. The primary problem is the destruction of alveoli, which reduces the surface area for gas exchange, leading to diffusion limitation, not altered haemoglobin function.
Question 123) A 28-year-old man suffers a pneumothorax, causing 50% collapse of his right lung. How will this physiologic alteration most significantly affect his pulmonary gas exchange?
A) Increased shunting in the right lung
B) Impaired diffusion in the right lung
C) Ventilation-perfusion mismatch
D) Elevated alveolar pCO2
E) Metabolic acidosis
Answer: C) Ventilation-perfusion mismatch
Explanation: The collapsed right lung alveoli will be ventilated but not perfused (therefore will be dead space), creating a major V/Q mismatch. Shunting and diffusion are not directly affected. pCO2 changes reflect ventilation not perfusion. There is no metabolic component.
A) Increased shunting in the right lung — Incorrect. Shunting refers to blood passing through areas of the lung without being oxygenated due to lack of ventilation. In a pneumothorax, the affected lung area is not ventilated but perfused, leading to ventilation-perfusion mismatch rather than pure shunting so in reality it would lead to dead space.
B) Impaired diffusion in the right lung — Incorrect. Diffusion impairment affects gas exchange across the alveolar membrane. In this case, the primary issue is that the lung is collapsed and cannot be ventilated, leading to ventilation-perfusion mismatch, not diffusion impairment.
D) Elevated alveolar pCO2 — Incorrect. Elevated alveolar pCO2 would reflect poor ventilation overall, but in pneumothorax, the main issue is a mismatch between ventilation and perfusion in the affected lung, rather than a systemic rise in alveolar CO2.
E) Metabolic acidosis — Incorrect. Metabolic acidosis is not directly related to the primary effects of a pneumothorax. The main issue here is a ventilation-perfusion mismatch due to lung collapse, not a metabolic disturbance.
Question 124) A 67-year-old woman with severe COPD presents with dyspnea and confusion. Arterial blood gas shows:
pH 7.28 (normal 7.35-7.45)
PaCO2 58 mmHg (normal 35-45 mmHg)
HCO3 32 mEq/L (normal 22-26 mEq/L)
This blood gas pattern indicates which acid-base disorder?
A) Uncompensated Metabolic acidosis
B)Partially compensated Metabolic alkalosis
C) Partially compensated Respiratory acidosis
D) compensated Respiratory alkalosis
E) Combined metabolic and respiratory acidosis
Answer: C)Partially compensated Respiratory acidosis
Explanation: The low pH and high PaCO2 indicate respiratory acidosis. The kidneys have appropriately increased bicarbonate to partially compensate. There is no metabolic component.
A) Uncompensated Metabolic acidosis — Incorrect. Metabolic acidosis would be indicated by a low bicarbonate level, which is not seen here. It is respiratory due to High pCO2. The elevated HCO3 and PaCO2 reflect a respiratory issue with partial compensation.
B) Partially compensated Metabolic alkalosis — Incorrect. Metabolic alkalosis would present with an elevated pH, which is not the case here. The low pH indicates acidosis, and the elevated PaCO2 suggests a respiratory rather than metabolic cause. However it is partially compensated due to an increased bicarbonate level suggesting the kidneys are tyring to compensate.
D) Compensated Respiratory alkalosis — Incorrect. It is not compensated as the PH is still abnormal. Respiratory alkalosis would present with a low PaCO2 and a high pH. This patient has a high PaCO2 and low PH indicating respiratory acidosis.
E) Combined metabolic and respiratory acidosis — Incorrect. A combined disorder would show high PaCO2 and low HCO3 without compensation. In this case, the elevated bicarbonate shows compensation, ruling out a combined acidosis.
Question 125) A 28-year-old woman has diabetic ketoacidosis with arterial pH 7.1, HCO3- 12 mEq/L, and PaCO2 28 mmHg. As she improves with treatment, which finding indicates the lungs contributing to resolution of her acidosis?
A) pH 7.35, HCO3- 18 mEq/L, PaCO2 40 mmHg
B) pH 7.28, HCO3- 18 mEq/L, PaCO2 32 mmHg
C) pH 7.32, HCO3- 20 mEq/L, PaCO2 36 mmHg
D) pH 7.45, HCO3- 25 mEq/L, PaCO2 45 mmHg
E) pH 7.5, HCO3- 30 mEq/L, PaCO2 50 mmHg
Answer: D) pH 7.45, HCO3- 25 mEq/L, PaCO2 45 mmHg
Explanation: A normal pH with elevated PaCO2 and HCO3- indicates complete compensation of her metabolic acidosis by respiratory alkalosis, blowing off CO2. The other findings show incomplete compensation.
A) pH 7.35, HCO3- 18 mEq/L, PaCO2 40 mmHg — Incorrect. This pH and PaCO2 reflect a near-normal state but suggest that the lungs are not continuing to compensate by lowering PaCO2 to resolve the acidosis.
B) pH 7.28, HCO3- 18 mEq/L, PaCO2 32 mmHg — Incorrect. While the pH is improving, the PaCO2 is not sufficiently low to indicate adequate respiratory compensation.
C) pH 7.32, HCO3- 20 mEq/L, PaCO2 36 mmHg — Incorrect. Though the pH and HCO3 are improving, the PaCO2 is not low enough to reflect sufficient respiratory compensation.
E) pH 7.5, HCO3- 30 mEq/L, PaCO2 50 mmHg — Incorrect. This pattern suggests respiratory acidosis with metabolic alkalosis, not resolution of ketoacidosis.
Question 126) A hospitalized patient has a central venous catheter sampling mixed venous blood. Which blood gas values reflect optimal pulmonary gas exchange?
A) High O2, low CO2
B) High O2, high CO2
C) Low O2, low CO2
D) Low O2, high CO2
E) Equal O2 and CO2
Answer: A) High O2, low CO2
Explanation: Well-oxygenated blood entering the left heart should have high O2 and low CO2, indicating optimal gas exchange in the lungs. Low O2 indicates poor oxygenation. High CO2 suggests inadequate ventilation.
B) High O2, high CO2 — Incorrect. High CO2 in blood returning to the heart indicates inadequate removal of CO2 by the lungs, suggesting poor gas exchange.
C) Low O2, low CO2 — Incorrect. Low oxygen indicates inadequate gas exchange, and low CO2 could suggest hyperventilation, but it does not reflect optimal pulmonary function.
D) Low O2, high CO2 — Incorrect. This pattern suggests poor oxygenation and inadequate CO2 removal, indicating severely impaired gas exchange.
E) Equal O2 and CO2 — Incorrect. Oxygen and carbon dioxide levels are never equal in optimal gas exchange, as O2 should be high and CO2 low in oxygenated blood.
Question 127) Which type of vaccine contains preformed antibodies that confer immediate but temporary protection?
A) Conjugate vaccine
B) Live attenuated vaccine
C) Inactivated vaccine
D) Passive vaccine
E) Subunit vaccine
Answer: D) Passive vaccine
Explanation: Passive vaccines contain preformed antibodies, usually monoclonal antibodies, that provide rapid protection without immune memory. The other types stimulate the recipient’s own antibody response.
A) Conjugate vaccine — Incorrect. Conjugate vaccines contain antigens linked to proteins to enhance immune response and to produce their own antibodies, but they do not provide immediate immunity through preformed antibodies.
B) Live attenuated vaccine — Incorrect. Live attenuated vaccines contain weakened forms of pathogens that stimulate the immune system to produce its own antibodies, not preformed antibodies.
C) Inactivated vaccine — Incorrect. Inactivated vaccines use killed pathogens to stimulate an immune response without preformed antibodies.
E) Subunit vaccine — Incorrect. Subunit vaccines contain specific parts of a pathogen, such as proteins, to trigger an immune response to produce their own antibodies, but they do not provide preformed antibodies.
Question 128) Which type of vaccine contains a weakened form of a live pathogen that still activates immune responses?
A) Subunit
B) Toxoid
C) Conjugate
D) Passive
E) Live attenuated
Answer: E) Live attenuated
Explanation: Live attenuated vaccines contain viruses or bacteria that are still alive but altered to reduce virulence and activate immunity without major infection. The other types do not contain live organisms.
A) Subunit — Incorrect. Subunit vaccines contain only specific components of a pathogen e.g. antigen and do not use live organisms.
B) Toxoid — Incorrect. Toxoid vaccines contain inactivated toxins rather than live pathogens and are used to protect against toxin-mediated diseases like tetanus.
C) Conjugate — Incorrect. Conjugate vaccines link weak antigens to stronger protein carriers to cause an enhanced immune response, but they do not contain live organisms.
D) Passive — Incorrect. Passive vaccines provide preformed antibodies and do not contain live pathogens.
Question 129) Which type of vaccine links a weak polysaccharide antigen to a stronger protein carrier to improve immunogenicity?
A) Inactivated
B) Subunit
C) DNA
D) Conjugate
E) Adjuvanted
Answer: D) Conjugate
Explanation: Conjugate vaccines covalently link polysaccharide antigens to carrier proteins, which improves their ability to generate T-cell dependent antibody responses.
A) Inactivated — Incorrect. Inactivated vaccines use killed pathogens without linking polysaccharides to proteins.
B) Subunit — Incorrect. Subunit vaccines use isolated antigen components but do not involve linking polysaccharides to protein carriers.
C) DNA — Incorrect. DNA vaccines use genetic material to stimulate an immune response, not polysaccharide-protein conjugation.
E) Adjuvanted — Incorrect. Adjuvanted vaccines include substances to enhance the immune response, but they do not link polysaccharides to proteins.
Question 130) Which type of vaccine contains only the antigenic parts of a pathogen, not the whole organism?
A) Live
B) Inactivated
C) Conjugate
D) Subunit
E) Passive
Answer: D) Subunit
Explanation: Subunit vaccines include only purified antigenic components of a pathogen, such as proteins or polysaccharides, not whole organisms. This improves their safety profile.
A) Live — Incorrect. Live vaccines contain weakened forms of the whole pathogen.
B) Inactivated — Incorrect. Inactivated vaccines use the entire pathogen, albeit in a killed form.
C) Conjugate — Incorrect. Conjugate vaccines involve a linked polysaccharide-protein antigen but can include the whole pathogen in some formulations.
E) Passive — Incorrect. Passive vaccines deliver preformed antibodies rather than components of a pathogen.
Question 131) Which of the following best describes the advantage of a conjugate vaccine over a plain polysaccharide vaccine?
A) Conjugate vaccines provide longer-lasting immunity.
B) Conjugate vaccines tend to be cheaper
C) Conjugate vaccines contain additional adjuvants.
D) Conjugate vaccines cover a wider variety of strains.
E) Conjugate vaccines have fewer side effects.
Answer: A) Conjugate vaccines provide longer-lasting immunity.
Explanation: Linking polysaccharide antigens to carrier proteins in conjugate vaccines makes them T-cell dependent and able to generate better immune responses and immune memory, whereas plain polysaccharide vaccines work poorly for immune memory. Conjugate vaccines provide longer protection and work in young children, but do not inherently contain novel adjuvants, cover more strains, or have fewer side effects compared to plain polysaccharide vaccines.
B) Conjugate vaccines tend to be cheaper — Incorrect. Conjugate vaccines are typically more complex and expensive to produce than plain polysaccharide vaccines, as they involve linking antigens to protein carriers to enhance immune response. Cost is not the advantage of conjugate vaccines.
C) Conjugate vaccines contain additional adjuvants — Incorrect. Conjugate vaccines do not inherently contain additional adjuvants. Their primary advantage is that they stimulate a T-cell dependent immune response, improving long-term immunity, especially in younger populations.
D) Conjugate vaccines cover a wider variety of strains — Incorrect. Conjugate vaccines do not inherently cover more strains than plain polysaccharide vaccines. Their key benefit lies in creating a stronger and longer-lasting immune response, particularly in children.
E) Conjugate vaccines have fewer side effects — Incorrect. Conjugate vaccines do not necessarily have fewer side effects compared to plain polysaccharide vaccines. The main advantage is improved immunogenicity and immune memory, not a reduced side effect profile.
Question 132) Asthma is known to be an obstructive disease, what would you expect to occur in an asthma patient
- A decrease in FVC
- FEV1/FVC >0.7
- A decrease in FEV1
- Bronchodilation
- A thick sticky mucus lining the airways
Answer: C) A decrease in FEV1
Explanation: In obstructive diseases the FEV1/FVC ratio decreases and becomes below 0.7, therefore you would expect to see a decreased FEV1 as there’s an obstruction (bronchoconstriction) so it is harder to exhale air therefore less air will be exhaled in the first second.
A) Decrease in FVC — Incorrect. While forced vital capacity (FVC) can decrease in severe asthma due to air trapping, it is not the most characteristic finding. A more prominent issue is the reduction in FEV1 due to obstruction. You would expect to see a decrease in FVC in a restrictive disease.
B) FEV1/FVC >0.7 — Incorrect. In asthma, the ratio of FEV1/FVC typically falls below 0.7 due to the significant reduction in FEV1 caused by airway obstruction. Unlike asthma in restrictive diseases you would expect a ratio above 0.7
D) Bronchodilation — Incorrect. Bronchodilation occurs as a response to medications (such as beta-agonists) used to treat asthma. However, the disease itself is characterized by bronchoconstriction, not bronchodilation.
E) Thick sticky mucus lining the airways — Correct but incomplete. While asthma patients do produce thick, sticky mucus, this is just one part of the disease. The characteristic feature of asthma is airway obstruction, leading to decreased FEV1 and FEV1/FVC.
