
Urology
Question 1:
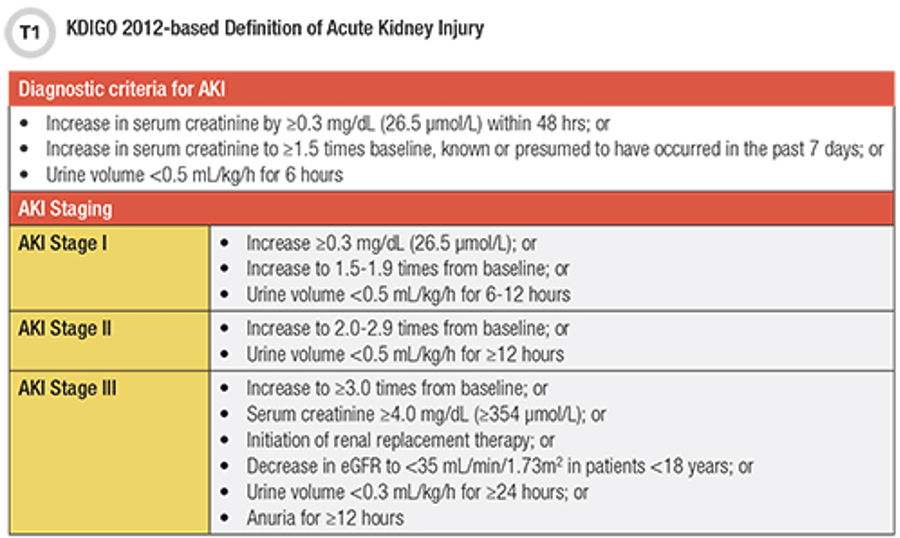
Answer: B) 26 µmol/L of creatinine
Explanation: Creatinine is a widely used biomarker for assessing renal function and detecting acute kidney injury (AKI). An increase in serum creatinine levels typically indicates impaired kidney function, as creatinine is a by-product of muscle metabolism that is normally filtered out by the kidneys.
Option A is incorrect because albumin levels are not a direct marker of AKI. Albuminuria (increased albumin in the urine) can indicate chronic kidney disease but is not a standard marker for acute kidney injury. It can be detected on a urine dipstick test.
Option C is incorrect because albumin at 30 µmol/L is also not relevant for diagnosing AKI.
Option D is incorrect because while creatinine is indeed used to detect AKI, a level of 30 µmol/L is not specifically significant without knowing the baseline and the rate of increase. The threshold rise in creatinine is critical for AKI diagnosis.
Option E is incorrect as inulin is used in specific tests to measure glomerular filtration rate (GFR) but is not commonly used as a marker for acute kidney injury in clinical settings.
Question 2:
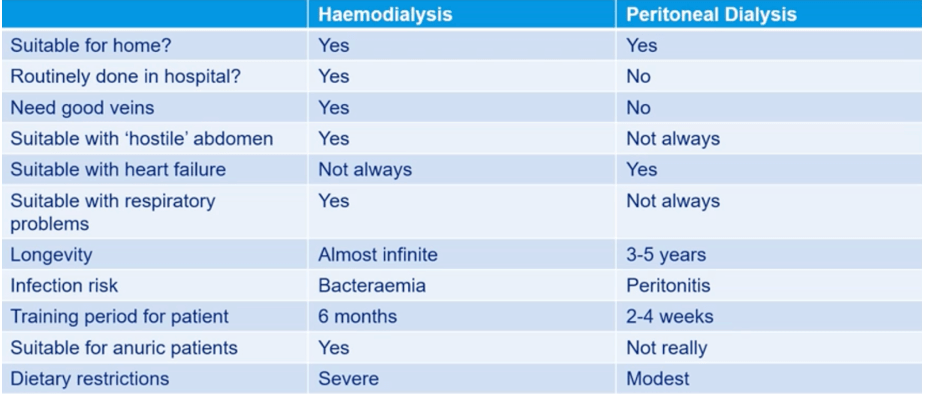
Answer: D) Peritoneal dialysis
Explanation: Peritoneal dialysis is less suitable for patients with respiratory issues, particularly those with chronic respiratory disease or volume overload, as it involves instilling fluid into the peritoneal cavity. The fluid can elevate the diaphragm, leading to reduced lung expansion, which may worsen respiratory function or exacerbate breathing difficulties.
Option A is incorrect because haemodialysis does not affect the diaphragm or lung expansion directly, making it more suitable for patients with respiratory conditions.
Option B is incorrect because hemofiltration is similar to haemodialysis in that it does not involve fluid in the abdominal cavity, thus avoiding respiratory compromise.
Option C is incorrect because hemodiafiltration, a combination of haemodialysis and hemofiltration, also does not involve fluid in the abdomen, making it relatively safe for patients with respiratory issues.
Option E is incorrect because a kidney transplant is a permanent solution rather than a temporary therapy, and it does not directly impact respiratory function in the way peritoneal dialysis might.

Question 3:
Answer: B) Testicular cancer
Explanation: Testicular cancer has the highest incidence rate among males aged 30-34. It is the most common cancer in young adult men, especially in the 15-35 age range. The disease often presents as a painless mass in the testicle and has a high cure rate if detected early.
Option A is incorrect because prostate cancer primarily affects older men, typically those over 50, with incidence rates increasing significantly with age.
Option C is incorrect as bladder cancer is more common in older adults, with risk increasing significantly after age 55.
Option D is incorrect because renal (kidney) cancer is also more prevalent in older adults, with peak incidence typically occurring in those over 60.
Option E is incorrect because benign prostatic hyperplasia (BPH) is a non-cancerous enlargement of the prostate that is common in older men, not in the 30-34 age group.

Question 4:
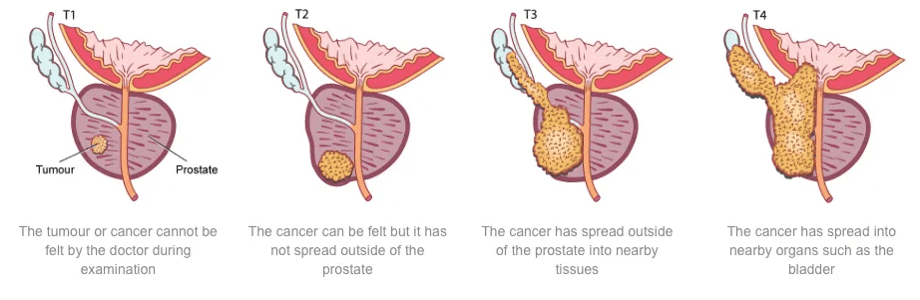
Answer: C) T1c
Explanation: Most prostate cancers are diagnosed at stage T1c due to widespread use of prostate-specific antigen (PSA) testing in routine screenings. T1c refers to prostate cancers that are not palpable on digital rectal examination (DRE) and are not visible by imaging but are detected due to elevated PSA levels. This stage is common because PSA screening often identifies prostate cancer before symptoms appear or the tumour can be physically detected.
Option A is incorrect because T1 is a broader category that includes T1a, T1b, and T1c. T1c specifically is the most frequently diagnosed stage due to PSA testing.
Option B is incorrect because T1a and T1b cancers are typically incidental findings in tissue removed for other reasons, such as surgery for benign prostatic hyperplasia (BPH) and are not the most common stage at diagnosis through screening.
Option D is incorrect because T2 cancers are confined to the prostate but are palpable or visible on imaging, often detected when there are some symptoms or a palpable mass.
Option E is incorrect because T3 and T4 indicate locally advanced or metastatic disease, which is less common at diagnosis, especially in populations undergoing routine screening.

Question 5:
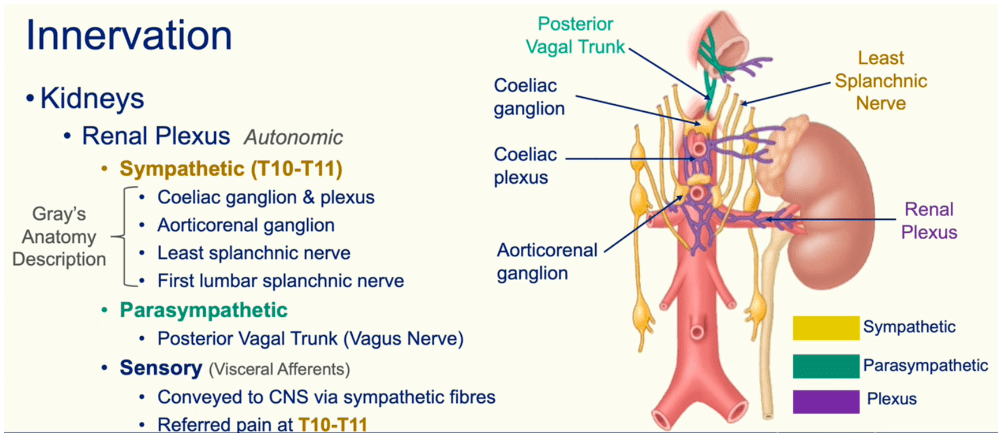
Answer: E) Greater splanchnic nerve
Explanation: The kidneys receive sympathetic innervation primarily from the coeliac ganglion and plexus, the aorticorenal ganglion, the least splanchnic nerve, and the first lumbar splanchnic nerve. These nerves provide sympathetic input, which affects blood flow, filtration, and renal tubular function.
Option A is incorrect because the coeliac ganglion and plexus contribute sympathetic fibres to the renal plexus, which supplies the kidneys.
Option B is incorrect because the aorticorenal ganglion provides sympathetic innervation to the kidneys.
Option C is incorrect because the least splanchnic nerve, arising from the lower thoracic sympathetic trunk, supplies the kidneys through the renal plexus.
Option D is incorrect because the first lumbar splanchnic nerve also plays a role in providing sympathetic input to the kidneys.
Question 6:
Answer: D) Teratomas
Explanation: Teratomas are germ cell tumours and are one of the primary types of testicular cancers arising from germ cells. They contain different tissue types and can occur in the testicles, often as part of mixed germ cell tumours, especially in younger men. Therefore, they are classified as germ cell tumours, not non-germ cell tumours.
Option A is incorrect because stromal tumours, which include Leydig cell and Sertoli cell tumours, are non-germ cell tumours that can occur in the testes.
Option B is incorrect because spermatic cord tumours, which are typically non-germ cell in origin, can develop in or near the testes and may lead to secondary issues in testicular tissue.
Option C is incorrect because lymphoid and hematopoietic tumours, although rare in the testicles, are considered non-germ cell tumours that can affect the testicular area.
Option E is incorrect because secondary tumours, or metastases from other cancers, can occur in the testes and are non-germ cell in origin.

Question 7:
Answer: C) High HCO₃⁻
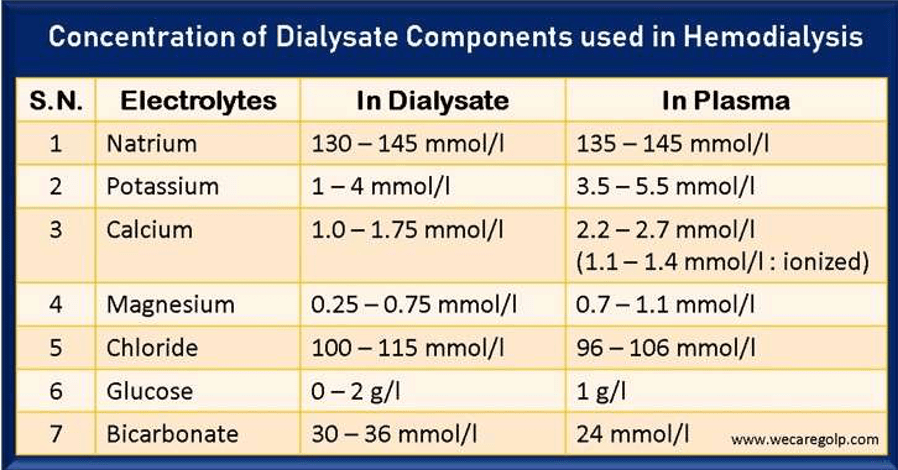
Explanation: Dialysate used in dialysis is carefully composed to help remove waste products from the blood while maintaining electrolyte balance. In patients with end-stage kidney disease, metabolic acidosis is common, so the dialysate typically contains a high concentration of bicarbonate (HCO₃⁻) to help buffer and correct acidosis.
Option A is incorrect because the sodium (Na⁺) concentration in dialysate is usually similar to normal plasma levels to avoid rapid shifts that could lead to imbalances or complications.
Option B is incorrect because high potassium (K⁺) levels would be dangerous in dialysis patients, as hyperkalaemia is often an issue due to impaired renal function. Dialysate typically has lower levels of K⁺ to help reduce serum potassium levels.
Option D is incorrect because high hydrogen ions (H⁺) would worsen acidosis, not alleviate it. Instead, bicarbonate in the dialysate helps to neutralize excess H⁺ in the patient’s blood.
Option E is incorrect because oxygen (O₂) is not directly added to the dialysate; oxygenation is managed separately if needed.
Question 8:
Answer: B) Ciprofloxacin
Explanation: Ciprofloxacin is often considered a third-line treatment for complicated & uncomplicated urinary tract infections (UTIs) & upper and lower UTIs, particularly in cases where first-line treatments (such as nitrofurantoin or trimethoprim-sulfamethoxazole) and second-line treatments (like beta-lactams) have failed, or the bacteria are resistant. Ciprofloxacin, a fluoroquinolone, is effective against many gram-negative bacteria that commonly cause UTIs & has great penetration into the bloodstream. However, it is reserved as a third line treatment since it increases risk of C. Difficile infection & can have severe side effects such as Achilles tendonitis, QT elongation & aortic aneurysm.
Option A is incorrect because ceftriaxone is usually reserved for severe or complicated UTIs that require intravenous therapy, rather than routine third-line oral treatment.
Option C is incorrect because amphotericin is an antifungal, not typically used to treat bacterial UTIs.
Option D is incorrect because pivmecillinam, while effective for UTIs, is more commonly used as a first- or second-line option in some regions, rather than a third-line treatment.
Option E is incorrect because trimethoprim is commonly used as a first-line treatment rather than a third-line option, especially if the bacteria are not resistant since it can not enter the bloodstream & is unsafe for pregnant women.
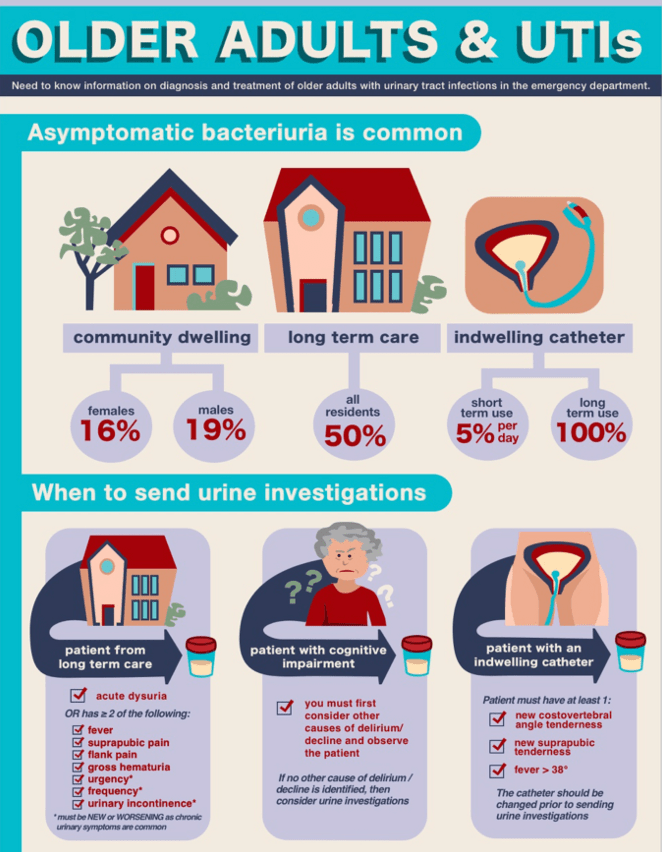
Question 9:
Answer: D) Temperature decreased by 1.5º
Explanation: A decrease in body temperature by 1.5º is not typically used as a clinical sign for diagnosing urinary tract infections (UTIs) in elderly individuals. Infections generally cause fever (increased temperature), but in elderly patients, the signs can sometimes be atypical, and they may present with hypothermia rather than hyperthermia. However, a specific decrease in temperature by 1.5º is not a recognised diagnostic marker for UTIs, instead old people tend to have a 1.5º increase in temperature.
Option A is incorrect because dysuria, or painful urination, is a common symptom of UTIs in elderly patients.
Option B is incorrect because haematuria, or blood in the urine, can be a sign of UTIs and may indicate inflammation or infection of the urinary tract.
Option C is incorrect because increased frequency and urgency are typical UTI symptoms, even more so in elderly individuals.
Option E is incorrect because suprapubic pain, or discomfort in the lower abdomen, is also a common symptom of UTIs.
Question 10:
Answer: C) T11-L2
Explanation: Pain from the ureters is typically referred to the dermatomes corresponding to spinal levels T11-L2. This pain often manifests as severe flank pain that radiates to the lower abdomen and groin, known as “loin to groin” pain, due to the sympathetic innervation of the ureters at these spinal levels.
Option A is incorrect because T10-T11 it is the referred region of pain of the kidneys.
Option B is incorrect because T0-L1 is the referred region of pain of the uterovaginal plexus.
Option D is incorrect because T11-L1 is the referred region of pain of the ovarian plexus although can initially be T10-T11 corresponding & often confused with appendicitis.
Option E is incorrect because T10-L2 extends beyond the typical range of T11-L2, including areas less commonly associated with ureteric pain.

Question 11:
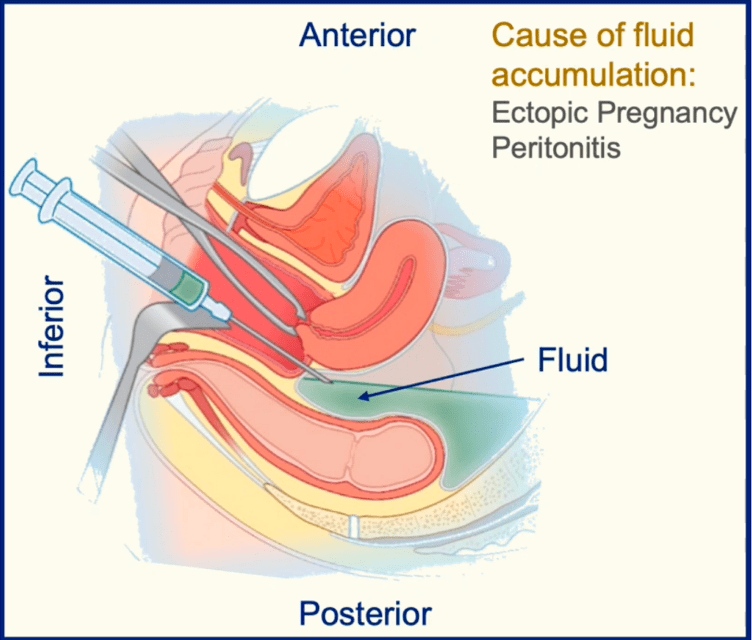
Answer: A) Rupture of ileum
Explanation: Fluid accumulation in the pouches of the broad ligament, specifically the vesicouterine pouch (between the bladder and uterus) and rectouterine pouch (also known as the pouch of Douglas, between the uterus and rectum), is often caused by conditions that directly affect the pelvic or abdominal area with inflammatory or infectious processes.
Option A is correct because rupture of the ileum, which is part of the small intestine, is not as likely to directly cause fluid accumulation in the pelvic pouches. While intestinal perforation can lead to peritonitis and diffuse fluid accumulation, the ileum is located higher up in the abdomen, so any leakage may not localise to the pelvic pouches as directly as other conditions listed here. The rectouterine pouch is drained via culdocentesis whereby a needle is inserted into the pouch via the posterior fornix in order to absorb excess fluid.
Option B is incorrect because rupture of the colon can lead to direct leakage of fluids and bacteria into the abdominal and pelvic cavity, potentially resulting in fluid accumulation in the pelvic pouches.
Option C is incorrect because ectopic pregnancy, particularly if it ruptures in the fallopian tube, can lead to haemorrhage or fluid accumulation in the rectouterine pouch due to its proximity to the reproductive organs.
Option D is incorrect because appendicitis, especially if ruptured, can lead to peritoneal fluid or pus spreading to the pelvic area, causing accumulation in the pelvic pouches.
Option E is incorrect because pelvic inflammatory disease (PID) often causes fluid or purulent exudate to collect in the pelvic cavity, which can accumulate in these pouches due to its proximity to the female reproductive organs.
Question 12:
Answer: D) Hypercalcaemia
Explanation: In chronic kidney disease (CKD), the kidneys are unable to excrete waste products effectively, leading to a build-up of nitrogenous compounds in the blood (azotaemia), as well as disturbances in electrolytes. Hyperkalaemia (high potassium levels) and hyperphosphatemia (high phosphate levels) are direct consequences of impaired renal function, as the kidneys lose their ability to excrete potassium and phosphate. Additionally, anaemia is a common consequence of CKD due to decreased erythropoietin production by the kidneys. Option D is correct because hypercalcaemia (high calcium levels) is not typically a direct consequence of CKD; in fact, patients with CKD often experience hypocalcaemia (low calcium levels) due to the kidneys’ impaired ability to convert vitamin D to its active form, leading to decreased intestinal absorption of calcium and contributing to secondary hyperparathyroidism.
Option A is incorrect because azotaemia is a hallmark of kidney dysfunction due to the accumulation of nitrogenous waste.
Option B is incorrect as hyperkalaemia is a direct result of the kidneys’ inability to excrete potassium.
Option C is incorrect because hyperphosphatemia occurs due to the decreased ability to excrete phosphate in CKD.
Option E is incorrect since anaemia is a well-known complication of CKD due to insufficient erythropoietin production.
Question 13:
Answer: B) Albumin
Explanation: To diagnose chronic kidney disease (CKD), it is essential to measure not only the estimated glomerular filtration rate (eGFR) but also markers of kidney damage. Albuminuria, which refers to the presence of albumin in the urine, is a key indicator of kidney damage. The measurement of albumin in the urine (often through a urine albumin-to-creatinine ratio) helps to assess the degree of kidney injury and is critical in the diagnosis and staging of CKD. It can also be indirectly measured using a urine-dipstick test which can highlight any presence of protein in urine.
Option A is incorrect because while creatinine is used to calculate eGFR, it alone does not indicate kidney damage. Furthermore, kidney damage is only indicated on eGFR when almost half of the renal function is impaired, thus it is crucial to conduct a urine-dipstick test as any small presence can indicate the potential of CKD regardless of how early the damage is.
Option C is incorrect since urine output can provide some information about kidney function but is not a definitive measure for diagnosing CKD. Decreased urine output typically takes a very long time to develop thus it is more useful for the diagnosis of acute kidney injury.
Option D is incorrect because the PTH blood test is more relevant for assessing complications of CKD rather than diagnosing it.
Option E is incorrect as measuring calcitriol concentration is not standard for diagnosing CKD, although it may be relevant in assessing metabolic bone disease associated with CKD.

Question 14:
Answer: E) Weight (or muscle mass)
Explanation: The estimated glomerular filtration rate (eGFR) is commonly calculated using factors such as age, gender, race, and serum creatinine concentration. These factors help adjust the eGFR value to account for differences in kidney function related to demographic characteristics and creatinine production, ensuring a more accurate assessment. Weight or muscle mass is not directly included in standard eGFR equations; however, creatinine levels can be indirectly influenced by muscle mass.
Option A is incorrect because age is an essential factor in the eGFR calculation, as kidney function typically decreases with age.
Option B is incorrect because gender is used in the calculation, reflecting differences in baseline creatinine levels between men and women.
Option C is incorrect as race was traditionally included, particularly to adjust for differences observed in Black populations; however, its use in eGFR calculations is now debated and being re-evaluated in some guidelines.
Option D is incorrect because creatinine concentration is fundamental to calculating eGFR, as it reflects kidney filtration ability.
Question 15:
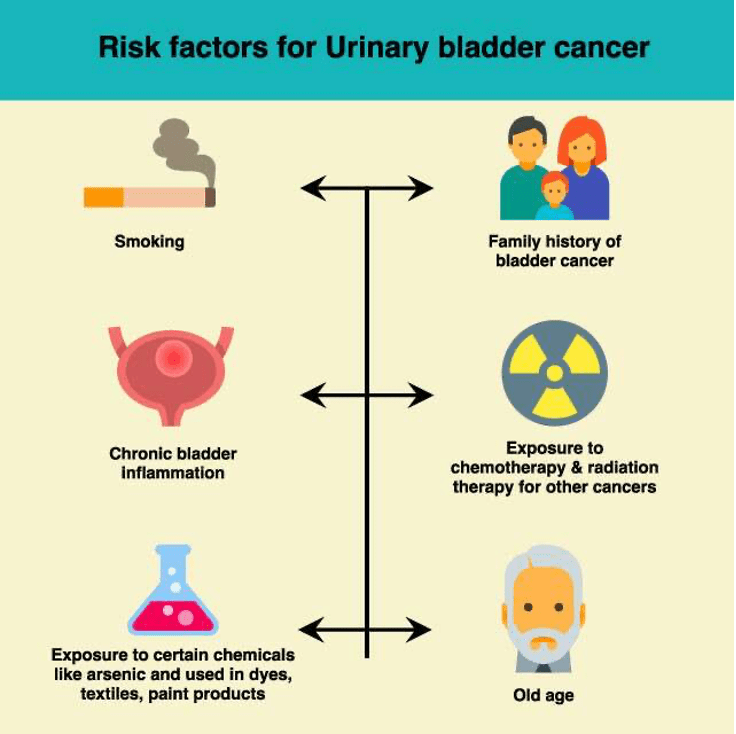
Answer: B) Obesity
Explanation: Bladder cancer is influenced by various risk factors, including smoking, radiation exposure, certain occupational exposures, and chronic inflammation of the bladder lining. Smoking is the most significant risk factor for bladder cancer, as the chemicals in tobacco can accumulate in the bladder and cause cellular damage. Occupational exposure to carcinogenic chemicals, such as those found in dyes, rubber, and chemicals, is also a known risk aka aromatic amines & polycyclic aromatic hydrocarbon. Radiation and certain chemotherapy treatments can predispose individuals to bladder cancer as well, and chronic inflammation from recurrent infections or conditions like schistosomiasis has been associated with increased risk.
Option B is correct because obesity is not generally considered a predisposing factor for bladder cancer, although it is a risk factor for several other cancers, including kidney and colorectal cancer.
Option A is incorrect because smoking is a major risk factor for bladder cancer.
Option C is incorrect because radiation and certain iatrogenic (treatment-related) exposures can increase the risk of bladder cancer.
Option D is incorrect as occupational exposure to carcinogenic substances is a well-established risk factor.
Option E is incorrect because chronic inflammation, particularly due to recurrent infections, is associated with an elevated risk of bladder cancer.
Question 16:
Explanation: The most common type of bladder cancer in the UK is transitional cell carcinoma (also known as urothelial carcinoma), which originates in the urothelial cells lining the bladder. Squamous cell carcinoma is the second most common type and is often associated with chronic irritation or inflammation of the bladder, such as that caused by recurrent infections or bladder stones. While squamous cell carcinoma is not as prevalent as transitional cell carcinoma, it remains the second leading cause of bladder cancer in the UK, particularly in patients with chronic inflammatory conditions affecting the bladder.
Option B is incorrect because adenocarcinomas are rare in the bladder and make up a very small percentage of bladder cancers (~2%).
Option C is incorrect as transitional cell carcinoma is the most common, not the second most common.
Option D is incorrect because small cell lung cancer is unrelated to bladder cancer and does not contribute to bladder cancer cases.
Option E is incorrect as non-invasive papillary carcinoma is a subtype of transitional cell carcinoma and is considered part of the most common category rather than a separate second leading cause.
Question 17:
Answer: D) Decreased urine output
Explanation: In the context of suspected acute kidney injury (AKI), fluid resuscitation is generally indicated if decreased urine output is associated with signs of hypovolemia, suggesting that the kidneys may be under perfused due to insufficient circulating blood volume. In such cases, fluid resuscitation can help restore kidney perfusion and potentially improve kidney function if the AKI is pre-renal in nature.
Option A is incorrect because pitting oedema usually indicates fluid overload, not dehydration or hypovolemia, and fluid resuscitation would likely worsen the patient’s condition.
Option B is incorrect as a high jugular venous pressure suggests volume overload rather than a need for fluid resuscitation.
Option C is incorrect because tall T waves on an ECG suggest hyperkalaemia, an electrolyte imbalance seen in AKI, rather than hypovolemia; this would not typically indicate the need for fluid resuscitation. Instead, this would be treated via calcium gluconate (to protect the heart from elevated K+ levels) & insulin-glucose infusion to help move K+ into cells.
Option E is incorrect because pulmonary oedema is another sign of fluid overload; adding more fluids in this situation could exacerbate respiratory issues. Pulmonary oedema needs to be treated via diuretics and if the patient’s condition continues to deteriorate then the patient should be started on dialysis.
Question 18:
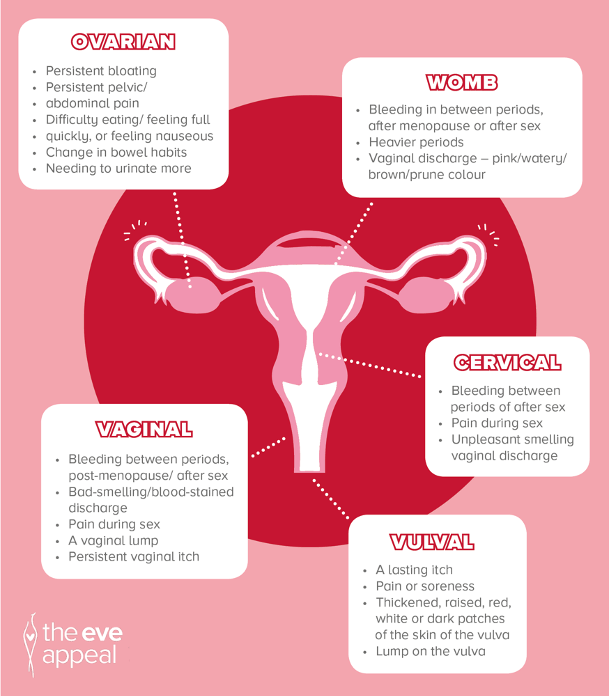
Answer: E) Fluid accumulation in pelvic pouches
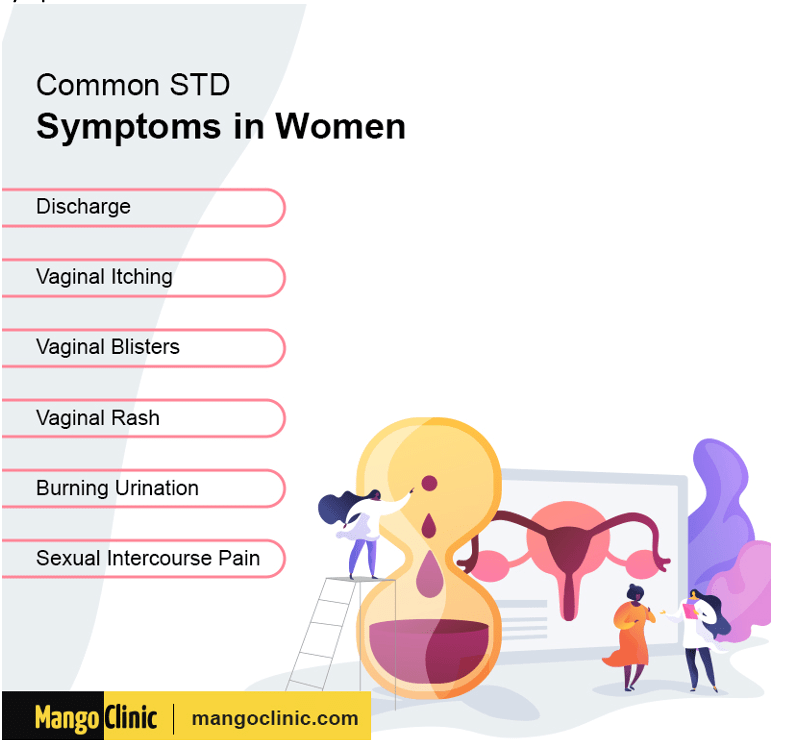
Explanation: The common symptoms of sexually transmitted infections (STIs) in females typically include dysuria (painful urination), dyspareunia (pain during intercourse), changes in vaginal discharge, and intermenstrual bleeding. These symptoms are often associated with infections such as chlamydia, mycoplasma and gonorrhoea, which can cause inflammation and affect the reproductive tract.
Option E is not a common symptom of STIs in females. While pelvic inflammatory disease (PID) can lead to fluid accumulation in the pelvic pouches due to complications from untreated STIs, this symptom is not typically reported as an initial or direct symptom of STIs. It is a potential consequence of untreated infections rather than a common presenting symptom.
Question 19:
Answer: C) BK causing bladder cancer
Explanation: Renal transplant patients are particularly susceptible to infections due to immunosuppressive therapy, and one of the significant viral infections they may experience is from the BK virus (BKV). BK virus is known to cause nephropathy in transplant recipients, but it can also lead to complications like haemorrhagic cystitis and has been associated with an increased risk of bladder cancer.
Option A is incorrect because hepatitis B (HEP B) can lead to hepatocellular carcinoma, but it is not the primary viral concern in the context of bladder cancer in kidney transplant patients.
Option B is incorrect as HPV is primarily linked to cervical and other anogenital cancers rather than liver cirrhosis.
Option D is incorrect because BK virus is not associated with prostate cancer.
Option E is incorrect; while hepatitis C (HEP C) can also lead to hepatocellular carcinoma, the context here focuses on BK virus and its implications in bladder cancer among renal transplant patients.
Question 20:
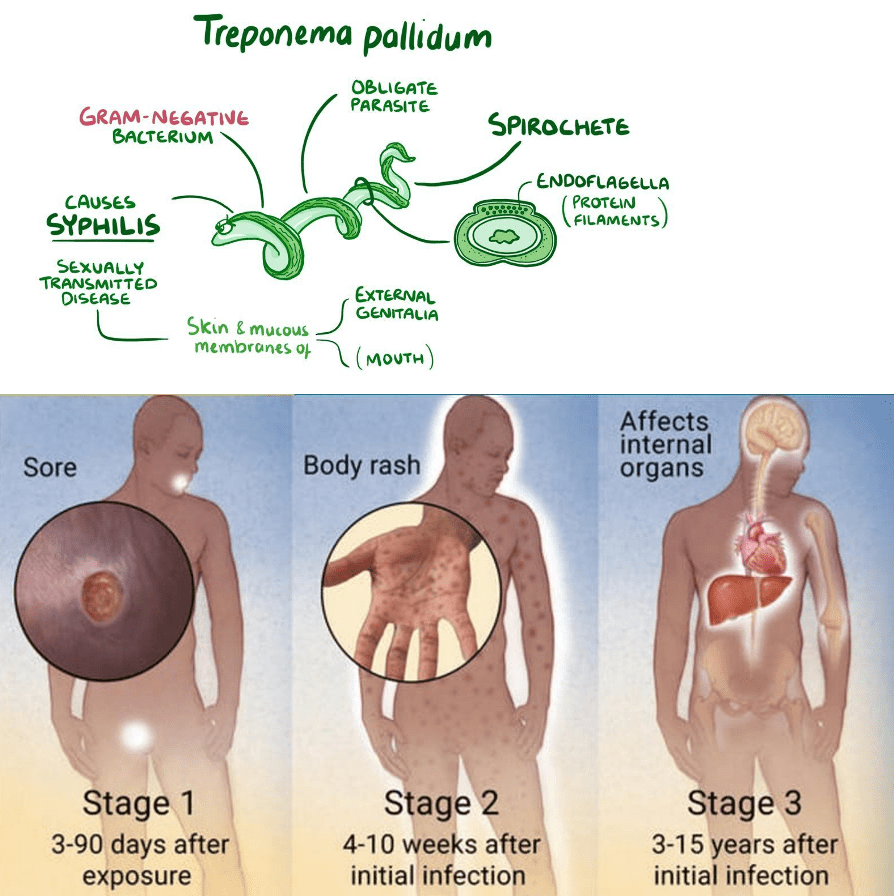
Answer: B) Treponema Pallidum
Explanation: A chancre is a painless ulcer that is most commonly associated with primary syphilis, which is caused by the bacterium Treponema pallidum. Swabbing the chancre can help in diagnosing syphilis through serological tests or PCR techniques that detect Treponema pallidum.
Option A is incorrect because Mycoplasma dentalium is typically diagnosed through urine or genital swabs but not specifically via a chancre swab.
Option C is incorrect as Neisseria gonorrhoeae is diagnosed from swabs of urethral or cervical discharge rather than a chancre.
Option D is incorrect because Chlamydia trichomatis is also diagnosed through swabs of urine or genital discharge, not directly from a chancre.
Option E is incorrect because non-specific urethritis is diagnosed based on symptoms and other tests rather than from a chancre swab.
Question 21:
Answer: D) Hyperthyroidism
Explanation: While hyperthyroidism can have some effects on pregnancy, it is generally not considered a significant direct cause of recurrent miscarriages, especially if it is mild and well-managed. Instead, hypothyroidism has a much greater risk of miscarriages along with insulin-dependant diabetes. The other conditions listed are more strongly associated with recurrent pregnancy loss.
Option A is incorrect because thrombophilia, a condition that affects blood clotting, can lead to placental issues, and is associated with recurrent miscarriages.
Option B is incorrect as antiphospholipid syndrome is a well-known autoimmune condition that can lead to increased risk of miscarriage due to thrombosis affecting placental blood flow.
Option C is incorrect because cervical weakness (cervical incompetence) can lead to miscarriage, especially in the second trimester whereby the cervix dilates too early. Regular measurements of the length of the cervix in such patients using ultrasounds is of paramount importance. Patients should also be given progesterone to maintain the lining of the uterus.
Option E is incorrect because chromosomal abnormalities are a common cause of recurrent pregnancy loss, particularly when there are issues with the embryo’s genetic material.

Question 22:
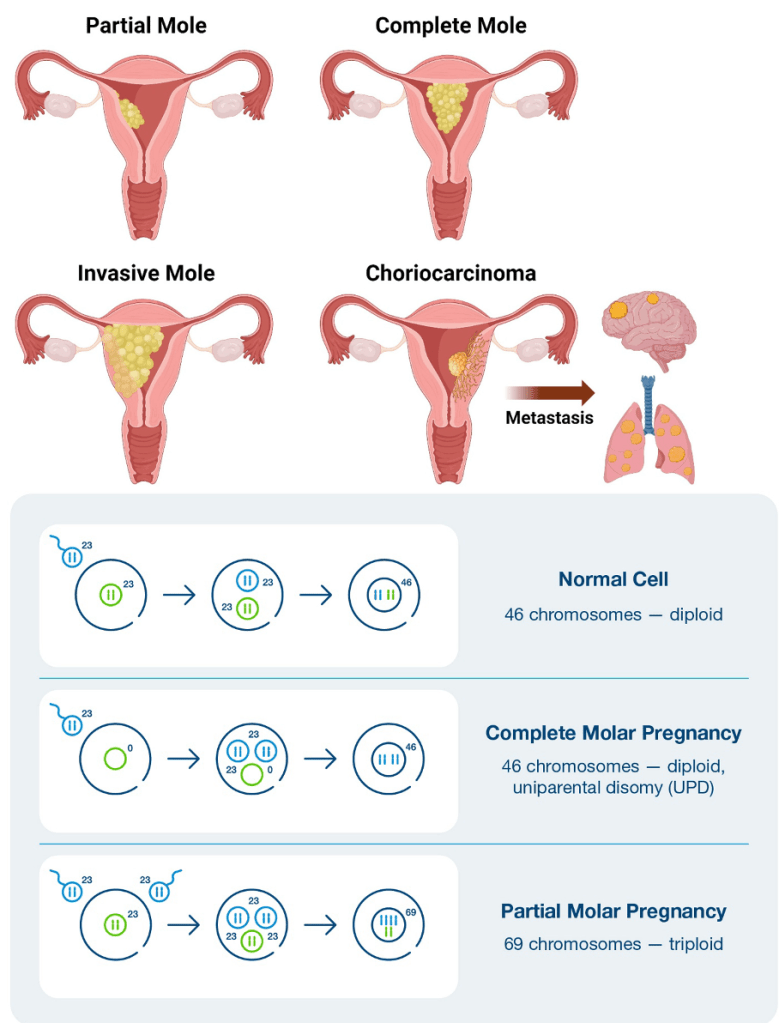
Answer: A) Complete = Sperm fertilises an empty egg which duplicates. Partial = 2 sperm fertilise a haploid egg
Explanation: A complete molar pregnancy occurs when a sperm fertilises an empty ovum, & then duplicates its chromosomes, resulting in the duplication of paternal chromosomes, leading to an absence of maternal genetic material. In contrast, a partial molar pregnancy involves the fertilisation of a normal ovum by two sperm, resulting in triploidy, which includes both maternal and paternal genetic material.
Option B is incorrect because a complete mole has no maternal genes / only paternal genes, while a partial mole includes both maternal and paternal genes.
Option C is incorrect as complete moles are usually diploid, whereas partial moles are typically triploid.
Option D is incorrect because neither type usually has identifiable foetal structures on ultrasound; partial moles may show some foetal tissue but often are associated with abnormal features.
Option E is incorrect as both types of molar pregnancies generally have elevated levels of ß-hCG compared to normal pregnancies.
Question 23:
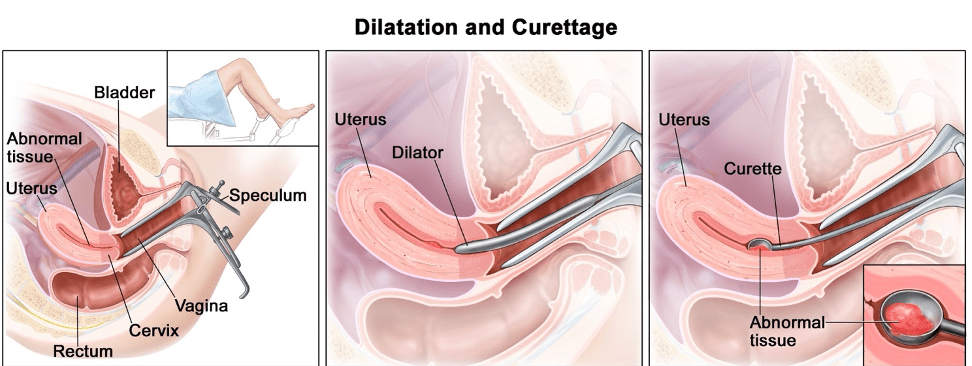
Answer: E) Surgical curette
Explanation: The first line treatment for a molar pregnancy, including complete hydatidiform moles, is surgical evacuation of the uterine contents via curettage. This procedure helps remove the molar tissue and reduces the risk of complications, such as the development of gestational trophoblastic neoplasia.
Option A is incorrect because hysterectomy is not routinely necessary for the treatment of molar pregnancies unless there are complications, or the patient has completed childbearing.
Option B is incorrect as chemotherapy is reserved for cases where there is persistent gestational trophoblastic disease following the evacuation (i.e., elevated ß-hCG).
Option C is incorrect because radiotherapy is not used in the treatment of molar pregnancies.
Option D is incorrect because a unilateral salpingo-oophorectomy is unrelated to the treatment of a molar pregnancy.
Question 24:
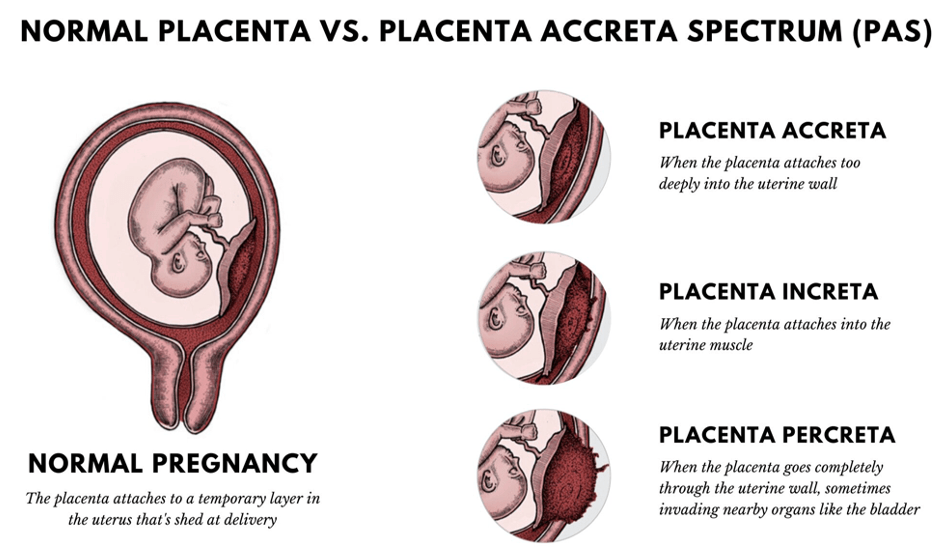
Answer: C) Placenta percreta
Explanation: Placenta percreta is characterised by the placenta invading endometrial tissue so far to the point where it is penetrating through the entire uterine wall and potentially invading adjacent organs, such as the bladder. This condition poses significant risks during delivery and may require surgical intervention.
Option A is incorrect because placenta praevia involves the placenta covering the cervical opening but does not imply invasion into surrounding tissues. A planned vaginal delivery is needed since there is a major risk of haemorrhage.
Option B is incorrect as placenta accreta refers to abnormal adherence of the placenta to the uterine wall without penetrating through it. The placenta often invades too deeply, especially at a previous scar, e.g., from a caesarean section.
Option D is incorrect because placenta increta involves the placenta invading into the myometrium but not beyond the uterine wall.
Option E is incorrect since a velamentous placenta refers to the abnormal insertion of foetal vessels into the membranes and does not indicate invasive behaviour. In this case, the umbilical cord inserts into the membrane of the placenta (between the amnion and the chorion) rather than directly into the placenta, meaning there is a significantly increased risk of haemorrhage.
Question 25:
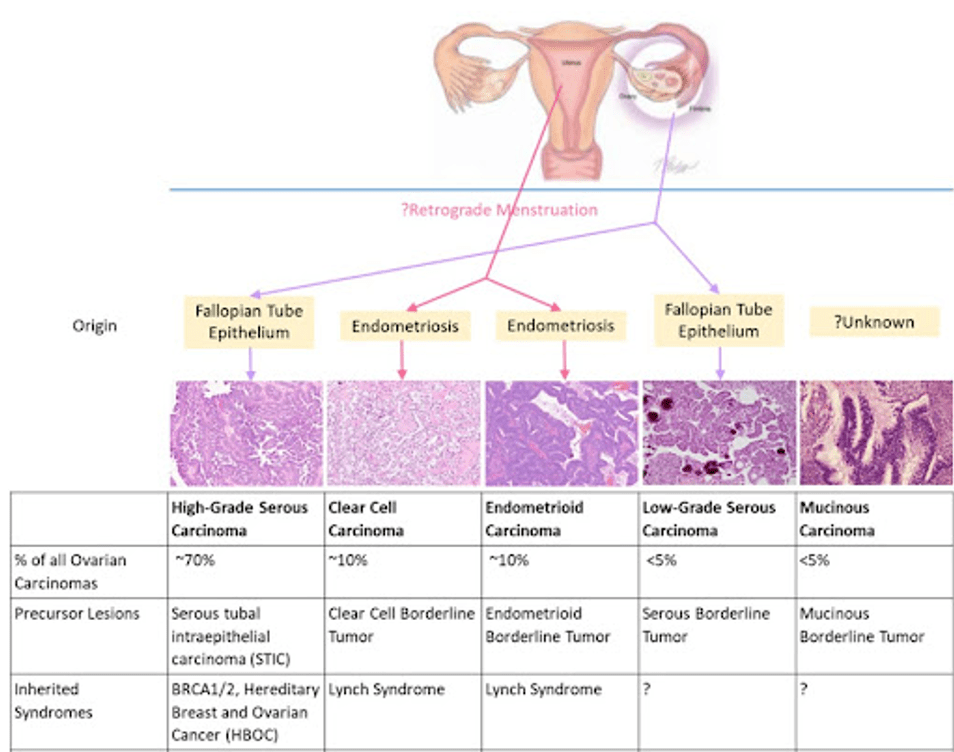
Answer: B) Brenner adenocarcinoma
Explanation: Brenner adenocarcinoma is characterised by the presence of transitional (urothelial) tissue. It is a rare type of ovarian tumour that is thought to originate from the transitional epithelium of the urinary tract.
Option A is incorrect because serous adenocarcinoma is the most common type of ovarian cancer and does not contain urothelial tissue; it is characterised by serous (watery) fluid and typically arises from the surface epithelium of the ovary.
Option C is incorrect as mucinous adenocarcinoma involves mucin-secreting epithelial cells associated with the bowel.
Option D is incorrect since endometrioid adenocarcinoma arises from endometrial-type epithelium and is related to endometriosis but does not contain urothelial tissue.
Option E is incorrect because clear cell adenocarcinoma aka serous adenocarcinoma is characterised by clear cells and is often associated with endometriosis but does not involve urothelial tissue.
Question 26:
Answer: B) Germ cell cancers
Explanation: Germ cell cancers, which include dysgerminomas and non-dysgerminomatous germ cell tumours, generally have a very good prognosis, particularly when diagnosed early. These tumours are often highly responsive to chemotherapy and can be cured in many cases.
Option A is incorrect because squamous epithelial ovarian cancers typically have a poorer prognosis compared to germ cell tumours, especially when diagnosed at an advanced stage. The majority of patients with advanced epithelial ovarian cancer only live 3 years post treatment. However, if all signs of atypia are removed then survival rate increases to 8-12 years.
Option C is incorrect as stromal cancers, such as granulosa cell tumours, have a generally favourable prognosis but are not as favourable as germ cell cancers overall.
Option D is incorrect because although endometrial cancer type 1 generally has a better prognosis compared to type 2, it may not surpass the favourable outcomes of germ cell cancers.
Option E is incorrect because endometrial cancer type 2 is associated with poorer prognosis compared to type 1, being more aggressive and typically diagnosed at a later stage.

Question 27:
Answer: D) Smoking
Explanation: Smoking is not considered a significant risk factor for type I endometrial cancer. In fact, it is more commonly associated with type II endometrial cancer, which has different characteristics and risk factors. Type I endometrial cancer is associated with high levels of unopposed oestrogen.
Option A is incorrect because obesity is a well-established risk factor for type I endometrial cancer due to its effect on oestrogen levels.
Option B is incorrect as polycystic ovary syndrome (PCOS) is associated with anovulation and increased oestrogen levels, contributing to the risk of type I endometrial cancer.
Option C is incorrect since Lynch Syndrome (hereditary nonpolyposis colorectal cancer) is associated with an increased risk of type I endometrial cancer among other cancers.
Option E is incorrect because diabetes, especially type II diabetes, is associated with obesity and increased oestrogen exposure, both of which are risk factors for type I endometrial cancer.
Question 28:
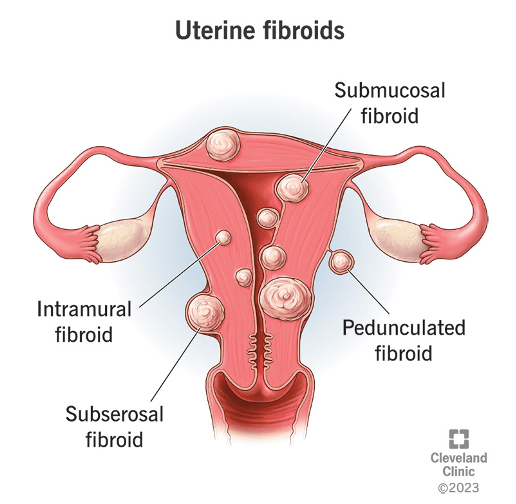
Answer: C) Uterine fibroids
Explanation: Uterine fibroids, also known as leiomyomas, are benign smooth muscle tumours of the uterus. They are particularly prevalent in women of African descent and can cause symptoms such as heavy menstrual bleeding and pelvic pain. There are 4 main types of fibroids aka leiomyomas: submucosal, subserosal, intramural & cervical
Option A is incorrect because endometriosis involves the growth of endometrial-like tissue outside the uterus and is not characterised by smooth muscle tumours.
Option B is incorrect as polycystic ovary syndrome (PCOS) is an endocrine disorder affecting ovarian function and is not related to uterine tumours.
Option D is incorrect because polyps are growths that protrude from the lining of the uterus (the endometrium), typically made of endometrial tissue rather than smooth muscle.
Option E is incorrect as adenomyosis involves the presence of endometrial tissue within the uterine muscle, which is different from the smooth muscle tumours described.

Question 29:
Answer: E) High FSH levels
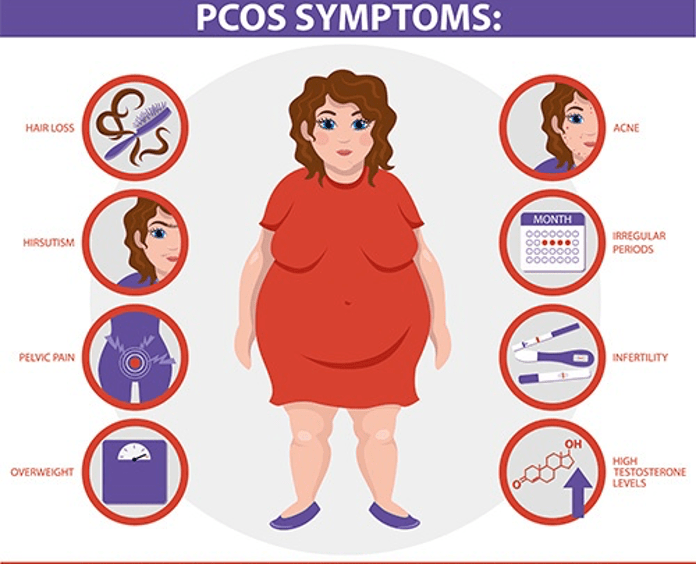
Explanation: In polycystic ovary syndrome (PCOS), women typically exhibit low to normal levels of follicle-stimulating hormone (FSH), rather than high levels. The hormonal imbalance is characterised more by elevated luteinizing hormone (LH) levels relative to FSH levels. This disrupts normal ovarian function and contributes to the irregular menstrual cycles characteristic of the syndrome.
Option A is incorrect because hyperinsulinemia is commonly associated with insulin resistance in PCOS. This condition leads to increased insulin levels in the bloodstream, which can stimulate ovarian androgen production, contributing to symptoms such as weight gain and excessive hair growth (hirsutism).
Option B is incorrect as hyperandrogenism is a hallmark of PCOS. Women with PCOS often have elevated levels of androgens (male hormones), which can lead to symptoms like acne, hirsutism, and menstrual irregularities. The overproduction of androgens is a key feature of the disorder.
Option C is incorrect because women with PCOS may exhibit high oestrogen levels. This is often due to increased conversion of androgens to oestrogens in adipose (fat) tissue. Elevated oestrogen levels can contribute to irregular menstrual cycles and other symptoms associated with PCOS.
Option D is incorrect as low levels of sex hormone-binding globulin (SHBG) are typical in PCOS. Lower SHBG levels lead to higher levels of free (active) androgens in the bloodstream, exacerbating symptoms of hyperandrogenism, such as hirsutism and acne.
Question 30:
Answer: B) Klinefelter’s Syndrome
Explanation: Premature ovarian insufficiency (POI) is characterised by the loss of normal ovarian function before the age of 40. Various genetic and autoimmune conditions are known to be associated with POI, but Klinefelter’s Syndrome primarily affects males and is characterised by hypogonadism and infertility due to an extra X chromosome (47,XXY). Therefore, it does not relate to ovarian insufficiency at all.
Option A is incorrect because Turner’s Syndrome is a condition that affects females and is characterised by the absence or structural abnormalities of one of the X chromosomes. Women with Turner’s Syndrome often experience ovarian failure (reduced follicular pool), leading to POI.
Option C is incorrect as galactosaemia is a metabolic disorder caused by the inability to metabolise galactose (due to defective/absent lactase). It has been associated with ovarian dysfunction, and affected females may experience POI.
Option D is incorrect because Fragile-X Syndrome is a genetic condition linked to intellectual disability and can also lead to premature ovarian insufficiency in women. The FMR1 gene mutation associated with Fragile-X Syndrome can affect ovarian function by upregulating the CGG codon.
Option E is incorrect because autoimmune disorders, such as Myasthenia Gravis & hypothyroidism, have been associated with premature ovarian insufficiency. Autoimmune conditions can lead to ovarian damage and contribute to the development of POI.

Question 31:
Answer: A) The child will experience rapid growth & exhibit gigantism
Explanation: Congenital Adrenal Hyperplasia (CAH) encompasses a group of genetic disorders that impair the adrenal glands’ ability to produce hormones, particularly cortisol. The most common form, 21-hydroxylase deficiency, results in an excess of androgens, which can impact growth patterns. Option A is correct because although children with CAH may initially show rapid growth due to excess adrenal androgens, this growth does not typically lead to gigantism. Instead, excessive androgen exposure can result in premature closure of growth plates, ultimately limiting final adult height resulting in a short stature.
Option B is incorrect as females with CAH often experience menstrual irregularities, including scant menstruation or amenorrhea, due to hormonal imbalances and abnormal adrenal androgen levels.
Option C is incorrect because boys with CAH are not at an increased risk for prostatic enlargement or prostatic cancer during childhood however, they are at much greater risk following puberty. The primary concerns for boys relate to early sexual maturation and potential adrenal crisis.
Option D is incorrect, as both boys and girls with CAH can present with symptoms of adrenal crisis, such as lethargy, vomiting, diarrhoea, dehydration, and hyperkalaemia due to insufficient mineralocorticoids.
Option E is incorrect, as children with CAH have low levels of glucocorticoids and mineralocorticoids, leading to hyponatremia (low sodium levels) due to impaired sodium regulation.

Question 32:
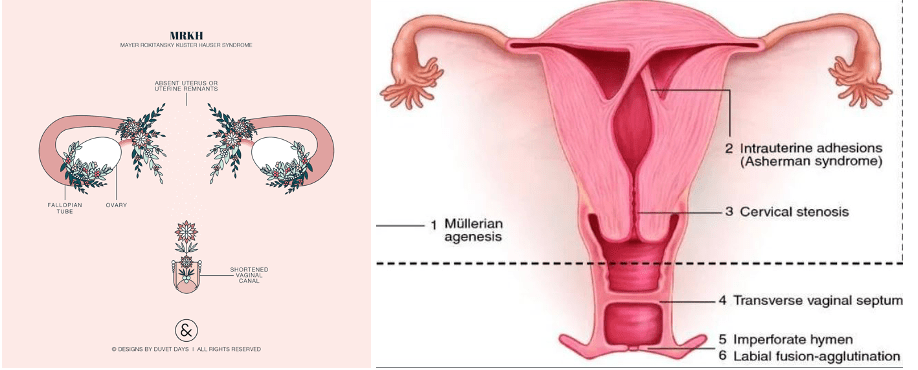
Answer: C) Vertical vaginal septum
Explanation: A vertical vaginal septum is a congenital condition in which a partition exists within the vagina, but it does not interfere with menstrual function since both the uterus and cervix remain intact. Therefore, individuals with this condition will still have normal menstrual cycles, although some may experience pain or difficulty with tampon use or intercourse. It may also causes problems during parturition (labour).
Option A is incorrect because an imperforate hymen blocks the outflow of menstrual blood, resulting in primary amenorrhea. Although the individual menstruates, the blood cannot exit, leading to hematocolpos (blood accumulation) and associated symptoms like abdominal pain.
Option B is incorrect as a transverse vaginal septum can obstruct menstrual flow if it completely blocks the vaginal canal, causing similar symptoms of amenorrhea and pain due to the retained blood.
Option D is incorrect because Mayer-Rokitansky-Küster-Hauser Syndrome involves the absence or underdevelopment of the uterus and upper vaginal tract, which leads to primary amenorrhea since no menstruation can occur in the absence of a functional endometrium.
Option E is incorrect as cervical agenesis involves the absence of the cervix, which prevents menstrual blood from exiting. Although the uterus may be present and functional, menstrual blood would accumulate, leading to amenorrhea and potentially severe abdominal pain.
Question 33:
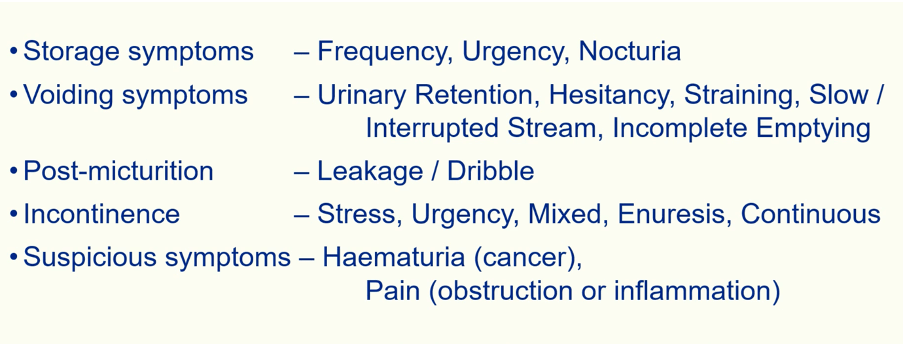
Answer: D) Nocturia
Explanation: Storage symptoms in the lower urinary tract refer to issues related to the bladder’s ability to store urine properly, leading to sensations or urges that impact comfort or control over urination. Nocturia, the need to wake up during the night to urinate, is a classic storage symptom indicating that the bladder is unable to hold urine effectively through the night.
Option A is incorrect because hesitancy is classified as a voiding symptom, involving difficulty in initiating urination due to problems with bladder outlet obstruction or detrusor muscle control.
Option B is incorrect as dribbling, or post-void dribbling, is a post-micturition symptom that occurs after urination, typically due to incomplete emptying or weakened pelvic floor muscles.
Option C is incorrect because straining is a voiding symptom in which an individual needs to apply pressure to begin or complete urination, often due to obstruction or weakened detrusor muscle function.
Option E is incorrect as incomplete emptying, the sensation of not fully emptying the bladder after urination, is categorised as voiding symptom and is usually due to issues like bladder outlet obstruction or detrusor underactivity rather than storage dysfunction.
Question 34:
Answer: A) Nitrofurantoin
Explanation: Nitrofurantoin is generally ineffective in patients with significant renal impairment, specifically those with an estimated glomerular filtration rate (eGFR) below 45 mL/min. This is because nitrofurantoin requires sufficient renal function for effective urinary concentration, and lower kidney function prevents it from reaching therapeutic levels in the urine. As a result, it is not recommended for treating UTIs in patients with renal failure.
Option B is incorrect because trimethoprim can still be effective in patients with moderate renal impairment, though dose adjustments may be needed.
Option C is incorrect because pivmecillinam, a beta-lactam antibiotic used for treating UTIs, does not rely on high renal function for efficacy and can still be effective in patients with reduced kidney function.
Option D is incorrect because ceftriaxone is largely excreted through the liver, meaning it is effective even in patients with significant renal impairment and does not require dose adjustments in most cases.
Option E is incorrect as ciprofloxacin, a fluoroquinolone, remains effective in renal failure, though dose adjustments may be necessary based on the degree of impairment.
Question 35:
Answer: D) Orchidectomy through inguinal incision
Explanation: Orchidectomy through inguinal incision is the primary treatment for testicular cancer. The testicle is removed through an incision in the groin (inguinal area) to prevent the cancer from spreading through the scrotal lymphatics. This procedure ensures both diagnosis and treatment. The testes and the scrotum have different lymphatic drainage routes. The testes primarily drain to the para-aortic lymph nodes, which are located around the aorta in the back of the abdomen (also called the retroperitoneal lymph nodes), while the scrotum drains to inguinal nodes. Making a cut in the scrotum could increase the risk of spreading cancer cells to the wrong lymph nodes, so the inguinal approach is preferred to isolate the cancer.
A) is incorrect as chemotherapy is often used as additional treatment after the primary surgery (orchidectomy), especially in cases of non-seminoma cancers or when the cancer has spread. It is not the first line of treatment.
B) is incorrect as radiation therapy is more commonly used for seminoma-type testicular cancers after the orchidectomy. While effective for seminoma, radiation is not always the primary treatment.
C) is incorrect as watchful waiting might be used in some cases for very early-stage cancer or small, non-aggressive tumours, but it is not a common or recommended approach for most testicular cancers, which are treated surgically.
E) is not the best answer as radical retroperitoneal lymph node dissection is used for further treatment if the cancer has spread to the lymph nodes in the back of the abdomen (retroperitoneal region). It is often performed after chemotherapy for metastatic cancer, not as the first treatment.
Question 36:
Answer: A) Fuhrman grade
Explanation: The Fuhrman grading system is used to describe how aggressive the cancer cells look under a microscope, based on nuclear size and shape. It is not part of TNM staging, but it helps in predicting the behaviour of the cancer. It is part of the grading and not staging system
B) Lymph node involvement is incorrect as the N in the TNM system refers to whether the cancer has spread to nearby lymph nodes. Spread to lymph nodes suggests a more advanced stage of the disease.
C) Metastasis is incorrect as the M in the TNM system refers to whether the cancer has spread to distant organs such as the lungs, bones, or liver. M1 indicates distant metastasis.
D) Tumour size is incorrect as this is part of the TNM staging system under the “T” category, which refers to the size and extent of the primary tumour. Larger tumours (T3, T4) indicate more advanced stages of cancer.
E) Invasion of nearby tissues is incorrect as the T component of the TNM system includes whether the tumour has invaded nearby tissues, such as the renal vein, perinephric fat, or beyond Gerota’s fascia (renal fascia surrounding the kidneys and fat).
Question 37:
Answer: B) Red-orange patch on the glans
Explanation: Zoon balanitis is a non-infectious inflammatory condition that occurs in older, uncircumcised men and involves the glans and foreskin. It is characterized by well-defined, glistening red-orange patches on the glans or foreskin. These patches are often described as “kissing lesions”, where affected areas on both sides of the foreskin touch. It is associated with chronic irritation but is not usually painful, though the appearance can be distressing.
A) Painful urination is incorrect as dysuria is more associated with urinary tract infections or sexually transmitted infections (STIs) rather than Zoon balanitis. UTIs can involve the bladder or urethra and cause pain during urination due to irritation or infection of the urinary tract lining. STIs can infect the urethra, causing inflammation and discomfort. Zoon balanitis, on the other hand, is a non-infectious inflammatory condition affecting the foreskin and glans of the penis, usually seen in uncircumcised men. It doesn’t typically involve the urinary tract or cause painful urination. Since Zoon balanitis affects the skin of the foreskin and glans but not the urethra or urinary system, it doesn’t cause dysuria.
C) is incorrect as Urethral discharge is more indicative of STIs like gonorrhoea or chlamydia while Zoon balanitis does not usually cause urethral discharge.
D) Foul-smelling discharge from the foreskin is incorrect as this is a symptom typical of bacterial infections or smegma buildup in cases of balanoposthitis (inflammation of both the foreskin and glans) can cause foul-smelling discharge due to the buildup of smegma (a white, cheese-like substance made of dead skin cells, oils, and moisture). It can also be due to bacterial or fungal infections under the foreskin. Conditions like candidiasis (thrush) or bacterial infections can produce this type of discharge not Zoon balanitis.
E) is incorrect as testicular swelling is a symptom of conditions like epididymo-orchitis, which is inflammation of the epididymis and testicle. This can be caused by bacterial infections, STIs like chlamydia, or even viral infections like mumps. Testicular swelling often presents with pain, redness, and sometimes fever. However, Zoon balanitis affects only the foreskin and glans of the penis, with no involvement of the testicles.
Question 38:
Answer: C) Ischaemia of the glans penis
Explanation: Paraphimosis occurs when the foreskin is retracted behind the glans and cannot return to its normal position. This causes constriction of blood flow, leading to potential ischaemia (lack of blood flow) to the glans penis. If untreated, this can cause necrosis (tissue death) of the glans, requiring surgical intervention. The most dangerous complication of untreated paraphimosis is ischaemia of the glans, which can lead to serious damage if not promptly addressed.
A) is incorrect as testicular cancer is a malignancy of the testicle, often associated with germ cell tumours. Paraphimosis involves the foreskin and glans, not the testicles, so it does not increase the risk of testicular cancer.
B) is incorrect as infertility is more commonly associated with conditions like varicocele (enlarged veins in the scrotum) or testicular torsion, which can impair sperm production. Paraphimosis, while serious, does not affect fertility directly unless severe infection or necrosis of penile tissue occurs.
D) is incorrect as prostate cancer is a malignancy of the prostate gland, common in older men. Paraphimosis has no effect on the prostate and does not increase the risk of prostate cancer.
E) is incorrect as urinary incontinence is the inability to control urination and is often related to prostate issues or bladder dysfunction. While paraphimosis may cause pain or difficulty urinating due to swelling of the foreskin and glans, it is not typically associated with urinary incontinence.
Question 39:
Answer: A) Haematuria
Explanation: Haematuria, or blood in the urine, is the most common presenting symptom of bladder cancer. It may be visible or non-visible (microscopic haematuria) and often occurs without any pain. This is a key warning sign prompting further evaluation, especially in individuals over 40.
B) is not the best answer as painful urination can occur due to bladder cancer, especially if a tumour irritates the bladder wall or causes obstruction. However, it is more commonly associated with urinary tract infections (UTIs) or other benign conditions.
C) is not the best answer as increased urinary frequency may occur if the bladder is irritated by a tumour or if it affects bladder capacity, but this symptom is more often associated with conditions like benign prostatic hyperplasia (BPH) or cystitis rather than directly indicating bladder cancer.
D) is not the best answer as urinary incontinence (involuntary loss of urine), can be caused by many conditions, including bladder cancer, but is not a typical presenting symptom. It often results from other urinary tract issues or age-related changes.
E) is not the best answer as while all options may occur in some patients, haematuria remains the primary and most common presenting symptom of bladder cancer, making this answer too broad.
Question 40:
Answer: A) Adenocarcinoma
Explanation: Adenocarcinoma is the most common type of prostate cancer, accounting for about 95% of all prostate cancer cases. It arises from the glandular cells of the prostate, which are responsible for producing prostate fluid. This type is prevalent in the general population and is usually the type diagnosed when prostate cancer is suspected through elevated PSA (prostate-specific antigen) levels or other symptoms.
B) is incorrect as transitional cell carcinoma originates from the urothelium and is more common in the bladder than in the prostate. While it can occur in the prostate, it is not the most common type of prostate cancer.
C) is incorrect as sarcoma a rare form of prostate cancer that originates from mesenchymal tissue (such as muscle, fat, or connective tissue) within the prostate. It is much less common than adenocarcinoma.
D) is incorrect as small cell carcinoma of the prostate is a rare and aggressive type of cancer that is not common and usually associated with poor prognosis. It often arises from a neuroendocrine differentiation of prostate cancer.
E) is incorrect as neuroendocrine carcinoma refers to a group of rare tumours that can occur in the prostate, often aggressive and associated with a worse prognosis. They account for a small percentage of prostate cancers.
Question 41:
Answer: B) It refers to the accumulation of plasma proteins in the glomeruli due to endothelial damage.
Explanation: Hyalinosis occurs when the endothelial cells of the glomeruli are injured, allowing plasma proteins to leak into the surrounding tissues. This accumulation leads to a characteristic glassy or homogeneous appearance under microscopic examination, indicative of chronic injury and is a key feature seen in glomerulosclerosis alongside sclerosis (scarring of the glomerulus). Glomerulosclerosis involves thickening and scarring of the glomeruli due to chronic injury, often linked to diabetes and hypertension.
A) It is the process of normal tissue repair after injury is incorrect as hyalinosis is associated with pathological changes in tissues and is not indicative of normal healing processes. It results from injury and subsequent protein leakage rather than typical repair mechanisms.
C) It indicates the presence of cancer cells in the glomeruli is incorrect as this refers to cancer-related changes, which would be indicative of neoplastic processes rather than hyalinosis, which involves protein deposition.
D) It is the inflammatory response to bacterial infection in the kidneys is incorrect. While inflammation may be a response to infection, hyalinosis is not specifically an inflammatory response. It represents changes related to chronic injury, typically from non-infectious processes.
E) It describes the degeneration of nerve tissues in the kidneys is incorrect as hyalinosis specifically relates to changes in the glomeruli and does not involve nerve tissues while this option is referring to neuropathy or nerve damage.
Question 42:
Answer: E) They decrease the reabsorption of sodium and glucose, leading to osmotic diuresis.
Explanation: SGLT2 inhibitors work by blocking the sodium-glucose cotransporter 2 in the proximal renal tubule, preventing glucose reabsorption. This results in increased urinary glucose excretion and sodium loss, promoting osmotic diuresis. The resulting decrease in intraglomerular pressure and improved tubular function help protect the kidneys from diabetic damage.
A) They reduce blood glucose levels only is incorrect as while SGLT2 inhibitors do lower blood glucose levels, their role in kidney function preservation extends beyond glucose control such as causing the afferent arteriole to vasoconstrict.
B) They increase insulin secretion from the pancreas is incorrect. SGLT2 inhibitors primarily affect the kidneys and do not increase insulin secretion. Their mechanism is focused on renal glucose handling rather than pancreatic function.
C) They cause vasodilation of renal arteries is incorrect as SGLT2 inhibitors do not primarily cause vasodilation, their main action occurs in the renal tubules rather than directly affecting the vascular structures of the kidneys.
D) They directly repair damaged kidney tissues is incorrect. SGLT2 inhibitors do not directly repair kidney tissues; instead, they work to prevent further damage and improve kidney function through their diuretic effects.
Question 43:
Answer: D) CDC originates in the medullary collecting ducts and is associated with poor prognosis.
Explanation: Collecting Duct Carcinoma (CDC) is a rare and aggressive type of renal cell carcinoma that originates from the medullary collecting ducts of the kidney. Its prognosis is generally poor because it is often diagnosed at an advanced stage. CDC is notorious for its rapid progression and resistance to standard treatments like chemotherapy and radiotherapy.
A) is incorrect as Clear cell RCC is the most common type of renal cell carcinoma, accounting for about 80% of cases. It is associated with mutations in the VHL gene (von Hippel-Lindau), a tumour suppressor gene, and tends to have a worse prognosis than other types of RCC. Histologically, clear cell RCC gets its name from the “clear” appearance of the cancer cells due to the high glycogen and lipid content inside the cells. The most common type of renal cell carcinoma (RCC) is clear cell carcinoma, which accounts for about 80% of cases. Collecting duct carcinoma (CDC) is a rare and aggressive type of RCC, accounting for less than 1% of all cases.
B) is incorrect as CDC generally affects middle-aged or older adults, not younger patients, and it has a very unfavourable prognosis due to its aggressive nature, Wilm’s tumour is the cancer that affects younger patients.
C) is incorrect as CDC arises from the collecting ducts in the renal medulla, not the renal cortex. The renal cortex is where clear cell carcinoma and papillary carcinoma typically arise particularly in the proximal convoluted tubule.
E) is incorrect as CDC does not respond well to chemotherapy. Treatment options are often limited, and the survival rate is generally low.
Question 44:
Answer: A) The failure of one or both testicles to descend into the scrotum
Explanation: Cryptorchidism refers to a condition where one or both testicles fail to descend into the scrotum during foetal development. Normally, the testes develop inside the abdomen and descend into the scrotum just before birth. If this descent doesn’t happen, the condition is called cryptorchidism or undescended testicles. It’s more common in premature infants but can also occur in full-term infants. It can increase the risk of infertility and testicular cancer if not corrected.
B) is incorrect as swelling of the testicles due to infection is referred to as epididymo-orchitis, not cryptorchidism. Epididymo-orchitis is an inflammatory condition affecting the testicles and epididymis.
C) is incorrect as the statement is describing testicular torsion, a condition where the spermatic cord twists, cutting off blood flow to the testicle, leading to ischaemia. Testicular torsion is a medical emergency, but it is not the same as cryptorchidism.
D) is incorrect as fluid collection around the testicle is called a hydrocele, not cryptorchidism and is due to a layer of fluid being trapped between the tunica vaginalis and tunica albuginea.
E) is incorrect as inflammation of the epididymis is called epididymitis, which can occur with or without inflammation of the testicle (orchitis).
Question 45:
Answer: B) Fuhrman Grading
Explanation: Fuhrman Grading is used specifically to grade the aggressiveness of renal cell carcinoma based on nuclear size, shape, and nucleolar prominence. It is a four-tier grading system (Grade 1 to Grade 4) with higher grades (e.g., grade 4) indicating irregular nuclei, poikilocytosis (abnormally shaped cells), and anisocytosis (unequal-sized cells), which signal aggressive behaviour and poor outcomes. Tumours with higher Fuhrman grades tend to grow faster and are more likely to metastasize.
A) is incorrect as Marsden Grading is used for testicular cancer, not RCC. It helps categorize the spread and aggressiveness of testicular tumours.
C) is incorrect as Gleason Score is used for prostate cancer grading, assessing the architectural pattern of cancer cells in biopsy samples. It provides a score that helps predict prognosis and the likelihood of metastasis in prostate cancer.
D) is incorrect as TNM Staging is a general system used for staging and not grading of cancers, it describes the Tumour size (T), Node involvement (N), and Metastasis (M) of many cancers, including RCC.
E) is incorrect as Robson Classification is an older system that was once used to stage RCC, focusing on tumour spread rather than cellular characteristics. It has been largely replaced by TNM staging.
Question 46:
Answer: A) Refractory hyperkalaemia
Explanation: Refractory hyperkalaemia is a life-threatening condition associated with AKI and dialysis is used as normal medical management has failed to work (refractory). When potassium levels rise dramatically, the heart is at risk of arrhythmias, which can be fatal. Usual treatment includes calcium gluconate to stabilize the heart, followed by methods to remove potassium such as insulin with glucose. When these methods fail and refractory (medical management has failed) pulmonary oedema is present, dialysis is used as they are both an emergency.
B) is incorrect as mild proteinuria is a common finding in both chronic kidney disease (CKD) and AKI, but it is not considered an emergency unless accompanied by other severe symptoms.
C) is incorrect as hypocalcaemia can occur in CKD and AKI due to impaired conversion of vitamin D, but it is generally treated with calcium supplementation and vitamin D analogues. It is not immediately life-threatening.
D) is incorrect as low-grade fever might suggest an infection, which could be concerning in a kidney patient, but on its own, it is not a medical emergency unless it escalates.
E) is not the best answer as peripheral oedema is often seen in CKD and AKI due to fluid retention but is not considered immediately life-threatening. Severe fluid overload, however, can lead to pulmonary oedema, which is an emergency.
Question 47:
Answer: E) Persistent reduction in eGFR (<60) for at least 3 months
Explanation: Persistent reduction in eGFR for at least 3 months is the clinical definition of CKD. Chronic kidney disease involves a long-term decline in kidney function, reflected by a reduced estimated glomerular filtration rate (eGFR) below 60, ACR (albumin to creatinine ratio) greater than 3mg/mmol and/or signs of kidney damage (e.g., proteinuria) lasting at least 3 months.
A) is incorrect as a rapid decline in kidney function over days is characteristic of acute kidney injury (AKI), not CKD. AKI occurs suddenly and is often reversible with proper treatment.
B) is not the best answer as sudden onset of haematuria (blood in urine) can be a sign of various conditions, including urinary tract infections, kidney stones, or bladder cancer. It is not a defining feature of CKD.
C) is incorrect as the presence of kidney stones (nephrolithiasis) can lead to acute episodes of pain and obstruction but does not define CKD. However, repeated stone formation can eventually damage the kidneys.
D) is incorrect as Temporary increase in creatinine levels due to dehydration may indicate pre-renal AKI, where dehydration leads to reduced blood flow to the kidneys. Once hydration is restored, kidney function typically returns to normal.
Question 48:
Answer: C) cardiovascular disease
Explanation: Cardiovascular disease is the leading cause of death in patients with CKD. CKD contributes to increased vascular calcification, hypertension, and dyslipidaemia, all of which accelerate the risk of heart disease. As kidney function declines, the risk of myocardial infarction (heart attack), heart failure, and stroke increases significantly.
A) is incorrect as although infections can be a risk in patients with CKD due to weakened immunity, it is not the most common cause of death. Infections are more frequent in advanced CKD stages but often come secondary to other complications.
B) is not the best answer as electrolyte imbalances such as hyperkalaemia can be life-threatening and require emergency treatment (e.g., dialysis), but they are not the most common cause of death in CKD patients. Electrolyte issues often accompany other conditions, like cardiovascular problems, that lead to fatal outcomes.
D) is not correct as renal cell carcinoma is more common in patients with end-stage kidney disease, especially those on long-term dialysis, but it is not the most frequent cause of death in CKD.
E) is incorrect as pulmonary embolism can be a complication in CKD patients due to immobility, but it is not the most common cause of death.
Question 49:
Answer: C) Testicular torsion
Explanation: The “bell clapper deformity” refers to the abnormal attachment of the testis, which allows it to twist on its own blood supply. This causes severe pain and is a urological emergency that requires immediate surgical intervention to prevent testicular necrosis.
A) is incorrect as a varicocele refers to dilated veins in the scrotum and is typically painless, unlike the acute pain of torsion.
B) is incorrect as hydrocele is the accumulation of fluid around the testicle, often painless or causing mild discomfort.
D) is incorrect as epididymo-orchitis is an infection or inflammation of the testis and epididymis, typically more gradual in onset and associated with fever.
E) is incorrect as cryptorchidism is the absence of one or both testes from the scrotum, usually noticed at birth as they haven’t descended properly, and is not related to acute pain.
Question 50:
Answer: B) Renal anaemia
Explanation: Renal anaemia is a major consequence of CKD. As the kidneys fail, they produce less erythropoietin, leading to decreased red blood cell production. Anther major consequence of CKD is CKD mineral and bone disease due to hypocalcaemia due to reduced activation of vitamin D (from calcidiol to calcitriol).
A) is incorrect as CKD often causes hypocalcaemia, not hypercalcemia, due to reduced vitamin D activation.
C) is incorrect as although patients with CKD may have cardiovascular risks, pulmonary embolism is not a direct consequence.
D) is not the best answer as hyperkalaemia is more common in advanced stages, due to reduced potassium excretion and can lead to arrhythmias.
E) is incorrect as CKD can cause hypertensive complications, but hypertensive retinopathy is more related to high blood pressure itself, not directly to kidney failure.
Question 51:
Answer: C) It allows for dialysis without a machine, multiple times a day
Explanation: Continuous Ambulatory Peritoneal Dialysis (CAPD) is a type of peritoneal dialysis that allows patients to perform dialysis manually, without a machine, several times a day. A sterile solution is introduced into the peritoneal cavity, and wastes diffuse across the peritoneum into the fluid, which is later drained.
A) is incorrect as the statement describes Automated Peritoneal Dialysis (APD), which is typically done overnight using a machine.
B) is incorrect as the statement describes haemodialysis, which uses an artificial kidney machine (dialyzer) to filter the blood.
D) is incorrect as CAPD involves both diffusion and convection. Diffusion removes small solutes, while convection helps remove larger molecules.
E) is incorrect as CAPD does not require hospitalization; it can be done at home unlike haemodialysis.
Question 52:
Answer: D) Ectopic pregnancy
Explanation: Culdocentesis is a procedure where a needle is inserted into the Pouch of Douglas aka Rectouterine pouch to check for blood or fluid, often used in the evaluation of suspected ruptured ectopic pregnancy.
A) is incorrect as Culdocentesis is not used for diagnosing ovarian cancer. It involves aspirating fluid from the rectouterine pouch.
B) is incorrect renal cyst rupture would be evaluated through imaging techniques, not culdocentesis.
C) is incorrect as testicular torsion is evaluated via physical exam and ultrasound, not culdocentesis.
E) is incorrect as prostate cancer is diagnosed using PSA levels, biopsy, and imaging
Question 53:
Answer: C) Autosomal Dominant Polycystic Kidney Disease (ADPKD)
Explanation: ADPKD is the best answer in this case because of the patient’s family history of kidney disease, the presence of multiple bilateral renal cysts, and the typical age of onset (adulthood). ADPKD is an inherited disorder that causes cyst formation in the kidneys due to mutations in the PKD1 or PKD2 genes, which are responsible for the integrity of the kidney’s structure. Over time, these cysts enlarge, compressing normal kidney tissue and leading to hypertension, flank pain, haematuria, and eventually chronic kidney disease (CKD) or end-stage renal disease (ESRD). Cysts may also develop in other organs like the liver. The autosomal dominant inheritance means that only one mutated gene is required to pass on the disease. Most patients begin to show symptoms in adulthood, typically in their 30s-40s, which aligns with this patient’s presentation.
A) is incorrect as Simple renal cysts are fluid-filled sacs that are commonly found in people as they age and are typically asymptomatic unless they grow very large or become infected. Simple renal cysts are often incidental findings and do not cause the progressive kidney dysfunction seen in ADPKD.
B) is incorrect as Autosomal Recessive Polycystic Kidney Disease (ARPKD) is a genetic condition that usually manifests in infancy or early childhood, not adulthood. Children with ARPKD often have bilateral enlarged kidneys with numerous cysts in the collecting ducts, but these cysts are much smaller than those seen in ADPKD. In ARPKD, the cysts lead to kidney failure at a very young age, and affected newborns may present with Potter syndrome due to low amniotic fluid (oligohydramnios). The patient in this case, being 45 years old and with symptoms manifesting later in life, fits better with ADPKD, not ARPKD.
D) is incorrect as acute Pyelonephritis is an infection of the kidneys typically caused by ascending bacterial infections from the bladder (a lower UTI). Common symptoms include fever, flank pain, nausea/vomiting, and dysuria (painful urination). Although flank pain is a symptom in both ADPKD and pyelonephritis, pyelonephritis is an acute condition with signs of infection (e.g., fever, elevated white blood cell count), which are absent in this case. Pyelonephritis also does not cause the development of multiple cysts or lead to chronic kidney failure.
E) is incorrect as although nephrolithiasis (kidney stones) can also cause flank pain and haematuria, it is a distinct condition from ADPKD. Kidney stones are solid deposits of minerals and salts such as Calcium phosphate or oxalate, uric acid or struvite that form within the kidney. While kidney stones can cause sudden and severe pain (renal colic), they do not cause the progressive cyst formation seen in ADPKD. Patients with ADPKD can sometimes develop kidney stones, but the primary pathology in ADPKD is the formation of multiple cysts, not stones.
Question 54:
Answer: B) Bacterial vaginosis
Explanation: Bacterial vaginosis (BV) is caused by an imbalance in the normal vaginal flora leading to a decrease or the absence of lactobacillus which is responsible for maintaining a low pH in the vagina to prevent overgrowth of harmful pathogens. This leads to an overgrowth of Gardnerella vaginalis and other anaerobic bacteria. Symptoms typically include malodorous discharge (fishy smell), but itching, burning, or pain is usually absent. BV is not considered an STI but is associated with sexual activity.
A) is incorrect as Candida vulvovaginitis is associated with thick, white, “cottage cheese-like” discharge, along with significant itching and irritation. Additionally, Candida infections do not usually have a strong odour, which is a key feature in this patient’s presentation.
C) is incorrect as Trichomoniasis is caused by Trichomonas vaginalis, a protozoan parasite. Trichomoniasis typically presents with frothy, yellow-green discharge, a strawberry red cervix and is often associated with vulvar itching, burning, and irritation. While foul odour can be a symptom, the characteristic discharge is different from the thin, grey discharge seen in bacterial vaginosis. Trichomoniasis is an STI and requires specific treatment (metronidazole).
D) is incorrect as Chlamydia cervicitis presents as mucous-like discharge from the cervix that is often yellow or green in colour. It is more common to have post-coital bleeding (bleeding after intercourse), along with symptoms like pelvic pain or dysuria. The discharge in this case does not match the typical presentation of Chlamydia, and there is no mention of recent sexual contact, which is more suggestive of an STI.
E) is incorrect as Gonorrhoea causes a purulent (pus-like) discharge and is a common STI. In women, it can cause cervicitis (inflammation of the cervix), pelvic pain, and dysuria. The discharge from gonorrhoea tends to be thick and purulent, not thin and grey as in this patient. Gonorrhoea can also cause systemic infections if untreated, but the absence of other symptoms and the fishy odour strongly suggests BV instead.
Question 55:
Answer: D. Fitz-Hugh-Curtis syndrome
Explanation: Fitz-Hugh-Curtis syndrome is a complication of PID where the infection spreads to the liver capsule, causing perihepatitis. This leads to upper right quadrant pain (often mimicking gallbladder or liver issues) and can present with pain that radiates to the right shoulder. It is most often associated with Chlamydia trachomatis or Neisseria gonorrhoeae. The hallmark finding is the formation of “violin string” adhesions between the liver and the peritoneum, which are visualized during laparoscopic surgery. While PID typically causes lower abdominal pain, Fitz-Hugh-Curtis syndrome adds upper quadrant discomfort due to the inflammation near the liver.

A) is incorrect as Epididymo-orchitis is an inflammation of the epididymis and the testis (orchitis) in males, usually caused by STIs like gonorrhoea or chlamydia. It presents with scrotal pain, swelling, and sometimes fever, but it is not a condition seen in females since they lack an epididymis and scrotum. It does not involve upper right quadrant pain and is not a complication of PID in females.
B) is incorrect as Cervical agenesis a congenital abnormality where the cervix fails to develop properly during embryogenesis due to a lack of canalisation. This condition would not be related to PID or to the development of upper right quadrant pain. Women with cervical agenesis typically present with primary amenorrhea (failure to menstruate) and reproductive difficulties rather than infection-related symptoms.
C) is incorrect as hematometra is the accumulation of blood in the uterus, often due to obstruction in the outflow of menstrual blood, such as a vaginal septum or cervical blockage. Symptoms include lower abdominal pain and amenorrhea. While it causes pelvic pain, it would not explain the right upper quadrant pain seen in this patient, nor would it be a common complication of PID.
E) is incorrect as bacterial vaginosis is a vaginal condition caused by an imbalance in the normal vaginal flora, often associated with an overgrowth of Gardnerella vaginalis and anaerobic bacteria. BV presents with thin, grey, malodorous discharge but is not associated with systemic symptoms like fever or upper abdominal pain. It is not a complication of PID and does not explain the patient’s upper right quadrant pain.
Question 56:
Answer: B) Nitrofurantoin for 5 days
Explanation: Nitrofurantoin is a commonly recommended first-line antibiotic for uncomplicated UTIs (typically occur in healthy, non-pregnant women with no structural or functional abnormalities of the urinary tract that can be caused By E. coli). A 5-day course of nitrofurantoin is effective, with minimal risk of side effects, and targets E. coli, Staphylococcus saprophyticus, Proteus, Pseudomonas and klebsiella but E. coli is the most common cause of UTIs. Nitrofurantoin is preferred because it concentrates well in the bladder, isn’t absorbed in the blood so acts locally instead of systemically and is less likely to contribute to bacterial resistance in other parts of the body.
A) is incorrect because amoxicillin is not typically first-line for uncomplicated UTIs. It may be used for complicated cases or if nitrofurantoin and trimethoprim are not options, as it has a broader spectrum – acting systemically, which could disrupt normal flora and contribute to resistance.
C) is incorrect because ciprofloxacin, a fluoroquinolone, is generally reserved as a last choice for complicated UTIs or cases where first-line agents cannot be used. Fluoroquinolones are associated with significant side effects (e.g., tendonitis, QT prolongation and increased risk of C. difficile infection), and overuse has led to rising resistance rates.
D) is not the best answer as although trimethoprim is one of the first-line options, it should only be given for 3 days for uncomplicated UTIs, not 14. A longer duration is unnecessary and may lead to adverse effects or resistance.
E) is incorrect because ceftriaxone is an injectable antibiotic (IV) used in severe or complicated cases, not uncomplicated UTIs or if ciprofloxacin is not working, as an OPAT (Outpatient IV Antibiotic Therapy). It is usually administered for patients with pyelonephritis or in cases where oral antibiotics are ineffective or inappropriate.
Question 57:
Answer: E) A 30 year old male with an indwelling catheter and symptoms of urinary tract infection.
Explanation: A UTI in a male patient with an indwelling catheter is classified as a complicated UTI. Indwelling catheters increase the risk of infection due to biofilm formation, where bacteria adhere to the catheter surface, making infections more challenging to treat and more likely to involve antibiotic-resistant organisms. And most males with a UTI often have a complicated UTI due to the general anatomy of the male urethra which is a lot longer compared to a female’s urethra.
A) is incorrect because a healthy female with no prior UTI history and symptoms like dysuria is likely to have an uncomplicated UTI. Uncomplicated UTIs are defined by the absence of structural or functional abnormalities and affect otherwise healthy, non-pregnant women.
B) is not the best answer because recent antibiotic treatment alone does not classify a UTI as complicated unless the infection involves resistant organisms or significant comorbidities. However, if symptoms persist despite appropriate treatment, further investigation may be warranted to rule out a complicated UTI.
C) is incorrect because a female with urinary urgency and no other health conditions is typically classified as having an uncomplicated UTI. No additional risk factors or complications make it complex.
D) is incorrect because oral contraceptives and mild urinary symptoms in an otherwise healthy woman do not meet the criteria for a complicated UTI. Risk factors for complicated UTIs typically include anatomical abnormalities, pregnancy, or comorbidities such as diabetes.
Question 58:
Answer: A) Calcium oxalate stones
Explanation: Calcium oxalate followed by Calcium phosphate stones are the most common type of kidney stones. They form when there is a high level of calcium or oxalate in the urine. Contributing factors include dehydration, high dietary oxalate intake (from foods like spinach or nuts), low citrate, high sodium, and conditions that increase calcium excretion, such as hyperparathyroidism. They appear radio-opaque on non-contrast X-rays and CTs meaning they are visible and appear white on these modalities. CT KUB (kidney, ureter and bladder) is the best imaging modality to diagnose stones. Treatment options for kidney stones include ESWL (shockwave lithotripsy), PCNL (percutaneous nephrolithotomy), and ureteroscopy. These procedures aim to break down and remove kidney stones.
B) is incorrect because uric acid stones are less common than calcium oxalate stones. They form when urine is persistently acidic, which can occur with high protein intake, gout, or metabolic syndromes. Uric acid stones are radiolucent, meaning they do not show up on standard X-rays, requiring other imaging methods.
C) is incorrect because struvite stones, also known as “infection stones,” are associated with urinary tract infections caused by urease-producing bacteria (e.g., Proteus or pseudomonas). They are less common and are more often found in women with recurrent UTIs and can lead to staghorn calculi.
D) is incorrect because cystine stones are rare and form due to cystinuria, an autosomal recessive condition that causes excessive cystine in the urine. Cystine is less soluble, which leads to stone formation.
E) Incorrect because magnesium ammonium phosphate stones are struvite stones.
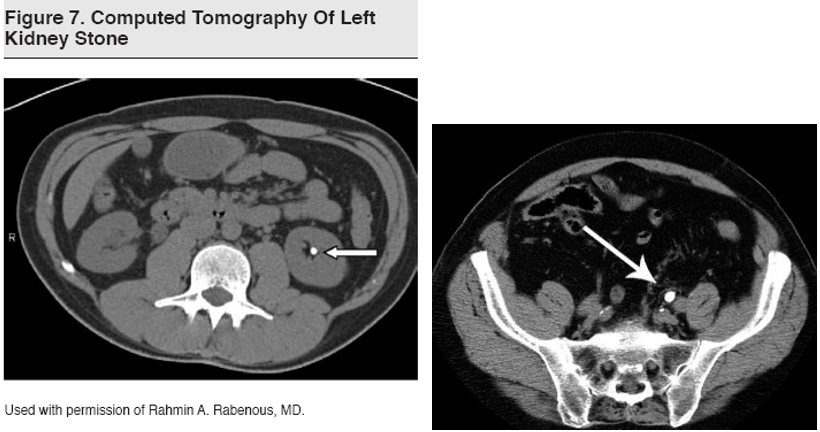
Question 59:
Answer: C) Horseshoe kidney
Explanation: Horseshoe kidney is a congenital anomaly where the lower poles of both kidneys are fused, forming a U-shape or “horseshoe.” They are usually located lower than normal kidneys as the Inferior Mesenteric Artery prevents them from ascending to their normal position. This anomaly occurs during foetal development. Horseshoe kidneys are located lower in the abdomen due to their fusion, which can cause issues with kidney drainage and increases the risk of kidney stones and infections. Although typically asymptomatic, patients may have urinary tract complications or abdominal pain.
A) is incorrect because crossed renal ectopia occurs when one kidney crosses to the opposite side and is located on the same side as the other kidney. In most cases, the ectopic kidney is fused with the other kidney, but the poles are not specifically involved as in a horseshoe kidney.
B) is incorrect because unilateral renal agenesis refers to the absence of one kidney from birth. This condition may go unnoticed due to the compensatory hypertrophy of the remaining kidney, allowing for normal kidney function.
D) is incorrect because bilateral renal agenesis is the absence of both kidneys, which is incompatible with life. This condition is associated with Potter syndrome, which includes characteristic facial features and pulmonary hypoplasia.
E) is incorrect because simple renal cysts are non-cancerous fluid-filled sacs that form within the kidneys, commonly with aging, but are not related to congenital anomalies like renal fusion.


Question 60:
Answer: A) Bilateral renal agenesis
Explanation: Bilateral renal agenesis is a congenital absence of both kidneys, leading to a lack of urine production in the foetus. This results in oligohydramnios (low amniotic fluid levels) and associated complications, including Potter syndrome, which involves characteristic facial features such as a flattened nose, low-set ears, and limb deformities. The absence of amniotic fluid also restricts lung development, often leading to life-threatening pulmonary hypoplasia.
B) is incorrect because crossed renal ectopia does not typically lead to oligohydramnios or Potter syndrome. It is an anomaly where one kidney is located on the opposite side, sometimes fused with the other kidney.
C) is incorrect because horseshoe kidney involves a fused lower pole but does not cause oligohydramnios or Potter syndrome. Most cases are asymptomatic and do not impact amniotic fluid levels.
D) is incorrect because renal dysplasia involves abnormal development of kidney tissue, which can lead to reduced kidney function but does not typically cause oligohydramnios or Potter syndrome.
E) is incorrect because complex renal cysts are a type of cyst with potential calcifications or septations and are usually assessed according to the Bosniak classification but are unrelated to Potter syndrome or amniotic fluid abnormalities.

Question 61:
Answer: C) A bulge that extends into the scrotum
Explanation: An inguino-scrotal hernia is a type of inguinal hernia that extends further down, where the hernia sac descends fully through the inguinal canal and into the scrotum. This type of hernia is more visually obvious because it often appears as a large swelling that can reach the scrotum, causing a scrotal bulge. Inguino-scrotal hernias are more prone to complications, especially if they become irreducible (cannot be pushed back into the abdomen), which increases the risk of strangulation due to a lack of blood and oxygen supply which is a medical emergency. During male foetal development, the processus vaginalis is an embryonic channel that extends from the abdomen to the scrotum, allowing the testicles to descend. Normally, this channel closes shortly after birth. If it fails to close, it leaves a potential pathway for abdominal contents like bowel to protrude, leading to an inguinal hernia. An inguinal hernia stays within the inguinal canal causing the groin to bulge, while an inguino-scrotal hernia extends down into the scrotum creating a more prominent bulge in the scrotum.
Question 62:
Answer: A) Congenital absence of the uterus and upper two-thirds of the vagina
Explanation: MRKH syndrome is a congenital disorder where the uterus and upper two-thirds of the vagina are absent, though the ovaries and external genitalia are typically normal. This is usually due to the absence of the Mullerian ducts. Individuals with MRKH syndrome may have normal secondary sexual characteristics but require specialized care for reproductive health.
B) is incorrect as although a unicornuate uterus is also a Müllerian anomaly, it involves the development of only one half of the uterus and not no uterus like in MRKH.
C) is incorrect as a transverse vaginal septum is a separate congenital condition involving a membrane across the vaginal canal whereby there is a lack of canalisation between the urogenital sinus (which forms the lower 1/3 of the vagina) and the mullerian ducts (which form the uterus and upper 2/3 of the vagina).
D) is incorrect as congenital adrenal hyperplasia (CAH) is an autosomal recessive disorder affecting adrenal hormone production, often leading to ambiguous genitalia in females characterised by the enlargement of the clitoris and fusion of the labial folds, while maintaining normal genitalia in affected males. The primary cause of CAH is a deficiency of the 21-hydroxylase enzyme.
E) is incorrect as a bicornuate uterus results from incomplete fusion of the Müllerian ducts but does not involve the absence of the uterus and upper vagina as in MRKH.
Question 63:
Answer: B) Normal menstruation but potential difficulty with tampon insertion
Explanation: A longitudinal vaginal septum divides the vaginal canal into two halves and failure of its canalisation can cause issues like difficulty inserting tampons or discomfort during intercourse, but menstruation typically remains unaffected.
A) is incorrect as amenorrhea (absence of the menstrual cycle) is not typically associated with a longitudinal vaginal septum, as it usually does not obstruct menstrual flow, it may be associated with a transverse vaginal septum, cervical agenesis or an imperforate hymen.
C) is incorrect because retained menstrual blood (hematocolpos) is more characteristic of a transverse vaginal septum or an imperforate hymen or cervical agenesis.
D) is incorrect as although some individuals may be asymptomatic, the septum often presents challenges like tampon or sexual discomfort, unlike a single normal canal.
E) is incorrect because infertility is not a usual presentation unless there are associated structural uterine anomalies.
Question 64:
Correct Answer: B)
B) The left renal vein crosses between the abdominal aorta and the superior mesenteric artery (SMA), leading to compression and increased venous pressure.
- Correct: This is the accurate explanation of Nutcracker Syndrome. The left renal vein’s anatomical position places it between the abdominal aorta and the SMA, and any narrowing of the space between these vessels causes compression, resulting in venous congestion and increased pressure. This leads to symptoms such as hematuria (blood in the urine), flank pain, varicocele in males, and pelvic congestion syndrome in females.
Explanation:
A) Compression of the right renal artery between the aorta and the superior mesenteric artery (SMA), leading to venous congestion.
- Incorrect: Nutcracker Syndrome involves the left renal vein, not the right renal artery. The condition is named for the “nutcracker” effect caused when the left renal vein is compressed between the aorta and the superior mesenteric artery (SMA). The compression leads to increased venous pressure, resulting in symptoms such as hematuria, flank pain, and varicocele in men.
C) The left kidney has a shorter renal vein compared to the right, leading to susceptibility to compression by nearby structures.
- Incorrect: In reality, the left renal vein is longer than the right renal vein and crosses over to reach the inferior vena cava. This long course actually makes it more susceptible to compression, rather than a shorter vein being involved in the cause of Nutcracker Syndrome.
D) The right renal vein drains into the inferior vena cava at an acute angle, making it more prone to compression by abdominal organs.
- Incorrect: The right renal vein typically drains directly and more vertically into the inferior vena cava and does not pass between major abdominal arteries like the left renal vein does. Therefore, it is not typically subject to compression in the same manner as the left renal vein.
E) Nutcracker Syndrome arises solely from congenital malformations of the renal vessels, causing severe compression of both renal veins.
- Incorrect: While anatomical variations can play a role in exacerbating Nutcracker Syndrome, it is primarily caused by the anatomical positioning of the left renal vein between the aorta and SMA. Congenital malformations alone do not fully explain the syndrome or its laterality.

Question 65:
Correct Answer: C)
C) Discontinue the NSAID and provide alternative pain management strategies.
- Correct: NSAIDs are known to be nephrotoxic and can worsen CKD, especially when used chronically. The first step in management would be to discontinue the NSAID and switch to safer pain management options, such as acetaminophen or non-pharmacological strategies (e.g., physical therapy) to protect kidney function.
Explanation:
A) Continue current medications but increase water intake to improve kidney perfusion.
- Incorrect: While adequate hydration is important, this option fails to address the critical issue of NSAID use, which can directly exacerbate kidney function decline due to their nephrotoxic potential. NSAIDs should be discontinued, particularly in patients with CKD. Simply increasing water intake is not sufficient to mitigate the risk.
B) Stop the ACE inhibitor to prevent further decline in kidney function.
- Incorrect: ACE inhibitors are generally protective in CKD, especially in patients with diabetes and proteinuria. They reduce proteinuria and slow the progression of kidney disease. Discontinuing the ACE inhibitor without a clear reason (such as hyperkalemia or a sudden worsening of kidney function) would not be appropriate.
D) Initiate high-protein dietary supplementation to support kidney function.
- Incorrect: High protein intake can actually worsen CKD by increasing the filtration load on the kidneys, accelerating disease progression. Patients with CKD are typically advised to maintain a moderate protein intake, not high.
E) Refer for dialysis due to the progression of kidney disease.
- Incorrect: This patient is at Stage 3 CKD with an eGFR of 38 mL/min/1.73 m², which does not warrant immediate dialysis. Dialysis is generally reserved for patients with Stage 5 CKD (eGFR < 15 mL/min/1.73 m²) or when symptoms of uremia, refractory hyperkalemia, or severe volume overload are present.
Question 66:
Correct Answer: A)
A) Prerenal AKI due to volume depletion.
- Correct: This is the most likely diagnosis, given the patient’s history of severe vomiting and diarrhoea leading to significant fluid loss. The clinical presentation of hypotension,low urinary output and elevated BUN-to-creatinine ratio suggests decreased renal perfusion as the primary cause of AKI.
Explanation:
B) Intrinsic AKI due to acute tubular necrosis (ATN) from ischemia.
- Incorrect: While severe prerenal AKI can progress to ATN if untreated, there is no evidence at this stage to suggest irreversible ischemic injury. Early management with rehydration can often reverse prerenal causes before they progress to ATN.
C) Postrenal AKI due to urinary tract obstruction.
- Incorrect: Postrenal AKI occurs due to physical obstruction in the urinary tract (e.g., kidney stones, enlarged prostate). This patient’s symptoms do not suggest urinary retention, flank pain, or signs of obstruction, making this diagnosis unlikely.
D) Intrinsic AKI due to acute interstitial nephritis (AIN) from a drug reaction.
- Incorrect: AIN is typically caused by hypersensitivity reactions to medications (e.g., antibiotics, NSAIDs) and presents with features such as rash, fever, and eosinophilia, none of which are mentioned in this patient’s case.
E) Prerenal AKI caused by hepatorenal syndrome.
- Incorrect:whilst it is pre-renal AKI, Hepatorenal syndrome occurs in patients with severe liver disease, leading to renal vasoconstriction. There is no indication in this patient’s history of liver disease or cirrhosis, making this an unlikely cause of his AKI.
Question 67:
Correct Answer: C)
C) Peritoneal dialysis is a continuous process that often allows for greater patient mobility and independence compared to intermittent hemodialysis.
- Correct: Peritoneal dialysis involves the continuous exchange of dialysate within the peritoneal cavity, which offers greater flexibility and independence for patients, especially those with chronic kidney disease, compared to the intermittent and center-based nature of hemodialysis.
Explanation:
A) Hemofiltration is preferred over hemodialysis for rapid removal of water-soluble toxins due to its superior diffusion capacity.
- Incorrect: Hemofiltration primarily relies on convection rather than diffusion for solute removal. Hemodialysis is more effective for removing small, water-soluble molecules due to its reliance on diffusion across a semi-permeable membrane.
B) Hemodialysis primarily relies on convection to clear solutes, while hemofiltration uses diffusion as its main method of solute clearance.
- Incorrect: This statement incorrectly reverses the primary mechanisms. Hemodialysis uses diffusion to move solutes across a concentration gradient, while hemofiltration uses convection, moving solutes along with water during ultrafiltration.
D) Hemofiltration is often chosen over hemodialysis for patients with chronic kidney disease requiring outpatient therapy.
- Incorrect: Hemodialysis, not hemofiltration, is the standard of care for most patients with chronic kidney disease in outpatient settings. Hemofiltration is more often used in intensive care settings, often for critically ill patients with acute kidney injury due to its gentler removal of fluid and solutes.
E) Hemodialysis cannot be used to treat acute kidney injury in critically ill patients due to its rapid fluid shifts and associated risks.
- Incorrect: Hemodialysis can be used to treat acute kidney injury, including in critically ill patients. However, hemodialysis may need to be modified (e.g., using slow, continuous methods) in such cases to avoid complications from rapid fluid and electrolyte shifts. Hemofiltration is another option that may be used due to its slower and more continuous approach.
Question 68:
Correct Answer: B)
B) The seminal vesicles contribute the largest volume of semen, which is deposited into the prostatic urethra via the ejaculatory ducts.
- Correct: The seminal vesicles produce the majority of seminal fluid, providing nutrients and substances that promote sperm viability and motility. During ejaculation, semen from the seminal vesicles and sperm from the vas deferens enter the prostatic urethra through the ejaculatory ducts.
Explanation:
A) Semen is primarily produced in the epididymis and is deposited directly into the spongy (penile) urethra.
- Incorrect: The epididymis is responsible for sperm maturation and storage, not the primary production of semen. Semen contains sperm, but most of its volume comes from the seminal vesicles and the prostate. Deposition of semen into the urethra occurs in the prostatic portion, not directly into the spongy (penile) urethra.
C) The majority of semen is produced in the testes and is deposited into the prostatic urethra through the ductus deferens.
- Incorrect: While the testes produce sperm cells, they do not produce the majority of the semen’s fluid volume. The vas deferens (ductus deferens) carries sperm from the epididymis to the urethra but does not produce or deposit large amounts of fluid. The seminal vesicles and prostate contribute significantly to semen volume.
D) The prostate gland is responsible for the majority of semen production and deposits it directly into the membranous urethra.
- Incorrect: While the prostate contributes some volume to semen and plays a role in fluid activation, it does not produce the majority of seminal fluid. It also releases its secretions into the prostatic urethra, not the membranous urethra.
E) Semen is formed mainly in the bulbourethral glands and is deposited into the urethra during arousal but not ejaculation.
- Incorrect: The bulbourethral (Cowper’s) glands produce a small amount of pre-ejaculatory fluid that lubricates the urethra but do not contribute significantly to the volume of semen or its deposition during ejaculation.
Question 69:
Correct Answer: A) low grade non invasive transitional cell carcinoma, TCC
- Correct: Mutations in the P21 RAS gene, a key regulator of the MAPK signaling pathway, are frequently implicated in the development of urothelial carcinoma (TCC) of the bladder. These mutations promote tumorigenesis by activating pathways that lead to increased cell proliferation and survival, characteristic features of TCC. Urothelial carcinoma is the most common type of bladder cancer, and P21 RAS mutations are a known driver in its pathogenesis.
Explanation:
B) Squamous cell carcinoma.
- Incorrect: Squamous cell carcinoma of the bladder is more commonly associated with chronic irritation, such as from urinary infections, stones, or catheter use, and not directly with mutations in the P21 RAS gene. While squamous cell carcinoma may share some molecular alterations with other cancers, RAS mutations are not a primary factor in its pathogenesis.
C) Adenocarcinoma.
- Incorrect: Adenocarcinoma of the bladder is a rare subtype and is typically associated with chronic inflammation or conditions such as bladder exstrophy. It is not commonly linked to mutations in the P21 RAS gene, which are more characteristic of urothelial carcinoma.
D) Small cell carcinoma.
- Incorrect: Small cell carcinoma of the bladder, although aggressive, has a distinct pathogenesis, often linked to neuroendocrine differentiation and is associated with other molecular alterations such as those affecting the p53 and RB pathways. P21 RAS mutations are not a typical driver of this cancer type.
E) high grade invasive transitional cell carcinoma
- Incorrect: whilst it is transitional cell carcinoma it is low grade caused by P21 RAS yet in this answer options it mentions high grade invasive transitional cell carcinoma. This type of carcinoma is invasive and flat, and is typically caused by mutation in TP53 genes which causes the cancer to grow deep into the muscular wall.
Question 70:
Correct Answer: C) T3a N0 M0
- Correct: T3a indicates that the tumor has spread beyond the prostatic capsule but without involvement of the seminal vesicles. N0 indicates no regional lymph node involvement, and M0 indicates no distant metastasis. This matches the described extracapsular extension without other spread.
Explanation:
A) T1c N2 M0
- Incorrect: T1c indicates a prostate cancer that is found by needle biopsy (often due to elevated PSA) but is not palpable or visible on imaging. This stage does not fit the scenario described, as there is evidence of extracapsular extension.Furthermore there is no lymph node involvement therefore it cannot be N2 which suggests more than 1 lymph node involvement around the pelvis.
B) T2 N1 M1
- Incorrect: T2 stage indicates that the tumor is confined within the prostate gland, with no spread beyond the capsule. In this patient, there is extracapsular extension, making this staging inappropriate.Furthermore there is no lymph node involvement therefore it cannot be N1 which suggests 1 lymph node involvement around the pelvis. It also cannot be M1 as there is no distant metastasis e.g in bones, liver and brain (rare).
D) T3b N1 M0
- Incorrect: T3b indicates that the tumor has invaded the seminal vesicles, which is not described in this patient. N1 indicates lymph node involvement, which the patient does not have, so this staging is not correct.
E) T4 N3 M0
- Incorrect: T4 indicates tumor invasion into adjacent structures other than the seminal vesicles (e.g., bladder neck, rectum, pelvic wall). This is more advanced than the extracapsular extension described for this patient, so it does not apply here. Additionally N3 suggests that there is more than 1 lymph node involvement outside the pelvis.
Question 71:
Correct Answer: D) Hydrocele
D) Hydrocele
- Correct: A hydrocele is a collection of fluid within the tunica vaginalis of the scrotum. It is usually painless, transilluminates with light, does not reduce on lying down, and is not associated with systemic symptoms. This fits the patient’s presentation perfectly.
Explanation:
A) Varicocele
- Incorrect: Varicocele is characterized by a “bag of worms” feel due to dilated veins of the pampiniform plexus. It usually becomes more prominent when standing and reduces when lying down. It does not transilluminate and is often associated with a dragging sensation, unlike the scenario described.
B) Epididymo-orchitis
- Incorrect: Epididymo-orchitis typically presents with scrotal pain, tenderness, and swelling, often accompanied by fever and erythema of the overlying skin. It is an inflammatory condition and would not transilluminate like a hydrocele.
C) Inguinoscrotal hernia of the gut
- Incorrect: An inguinoscrotal hernia may present as a swelling that increases with straining and may contain bowel, sometimes causing a gurgling sound. It does not transilluminate and often reduces when the patient is lying down or with gentle pressure.
E) Spermatocele
- Incorrect: A spermatocele is a cystic dilation of the epididymal duct and typically presents as a painless, cystic mass near the head of the epididymis. While it may transilluminate, it is often smaller than a hydrocele and has a different texture and location, typically being found posterior to the testis rather than causing generalised scrotal swelling. Furthermore when palpating this mass it would impossible to feel above its most superior point
Question 72:
Correct Answer: B) Nitrofurantoin for 5-7 days
- Correct: Nitrofurantoin is a commonly used antibiotic for uncomplicated lower UTIs in pregnant women. It is considered safe during the second trimester (but generally avoided in the first trimester and near term due to potential risks of hemolytic anemia in neonates). It is effective against common UTI pathogens such as E. coli.
Explanation:
A) Ciprofloxacin for 3 days
- Incorrect: Fluoroquinolones, such as ciprofloxacin, are generally avoided in pregnancy due to potential adverse effects on fetal cartilage development. It is not recommended for treating UTIs in pregnant women.
C) Trimethoprim-sulfamethoxazole (TMP-SMX) for 3 days
- Incorrect: TMP-SMX should generally be avoided during pregnancy, particularly during the first trimester due to the risk of neural tube defects and in the third trimester due to risk of neonatal jaundice. While it can be used cautiously in specific circumstances, it is not the first-line treatment for uncomplicated UTIs in pregnancy.
D) Doxycycline for 5 days
- Incorrect: Tetracyclines, such as doxycycline, are contraindicated in pregnancy due to risks of teeth discoloration and bone growth inhibition in the developing fetus. They are not appropriate for treating UTIs in pregnant women.
E) Amoxicillin-clavulanate for 3 days
- Incorrect: Although amoxicillin-clavulanate is a safe option in pregnancy, it is less effective for UTIs caused by E. coli due to increasing resistance. While it can be used in some cases, nitrofurantoin remains a more preferred option for uncomplicated lower UTIs in this scenario.
Question 73:
Correct Answer: D) Conservative management with hydration, analgesia, and medical expulsive therapy
D) Conservative management with hydration, analgesia, and medical expulsive therapy
- Correct: For a 5 mm ureteral stone, conservative management is appropriate. This includes adequate hydration, pain relief (e.g., NSAIDs), and potentially medical expulsive therapy such as alpha-blockers (e.g., tamsulosin) to facilitate stone passage. Many stones of this size pass spontaneously with supportive measures.
Explanation:
A) Immediate extracorporeal shock wave lithotripsy (ESWL)
- Incorrect: ESWL is a non-invasive procedure used to fragment stones, typically for stones in the kidney or upper ureter that are smaller and causing persistent symptoms despite conservative management. However, it is generally not the first-line approach for a 5 mm stone that may still pass spontaneously.
B) Ureteral stenting to relieve obstruction
- Incorrect: Ureteral stenting is used to relieve obstruction and maintain drainage in the presence of significant hydronephrosis or infection, neither of which are present in this patient. This patient’s stone is non-obstructive, so stenting is not warranted at this stage.
C) Percutaneous nephrolithotomy (PCNL)
- Incorrect: PCNL is a surgical approach typically reserved for large stones (greater than 2 cm) or complex stones not manageable with less invasive methods. It is not appropriate for a 5 mm ureteral stone, which has a reasonable chance of passing spontaneously.
E) Open surgical removal of the stone
- Incorrect: Open surgical removal is rarely performed for renal or ureteral stones in the modern era due to the availability of minimally invasive techniques. It is typically reserved for very complex or refractory cases and is not appropriate for a 6 mm stone that may pass with conservative therapy.
Question 74:
Correct Answer: C) Autosomal dominant polycystic kidney disease (ADPKD)
Correct: ADPKD is a genetic disorder that often presents in adulthood with multiple renal cysts, leading to kidney enlargement. The family history of kidney disease, hypertension, and cystic kidneys make ADPKD the most likely diagnosis.
Explanation:
A) Renal cell carcinoma (RCC)
- Incorrect: RCC typically presents as a solid mass within the kidney and may be associated with hematuria, flank pain, and systemic symptoms such as weight loss. However, the presence of bilaterally enlarged kidneys with multiple cysts strongly suggests a polycystic condition rather than cancer.
B) Autosomal recessive polycystic kidney disease (ARPKD)
- Incorrect: while it is polycystic kidney disease, due to the patient’s age it is likely to be autosomal dominant, ARPKD usually presents in infancy or early childhood with enlarged kidneys and hepatic fibrosis. Adult-onset cystic disease with a strong family history is more consistent with ADPKD.
D) Multicystic dysplastic kidney disease
- Incorrect: This is typically a congenital disorder seen in childhood, with a nonfunctional kidney full of cysts. It does not present bilaterally in adulthood with the findings described here.
E) Simple renal cyst
- Incorrect: Simple renal cysts are typically isolated and asymptomatic. The presence of multiple cysts, family history, and symptoms such as hypertension and hematuria point to a more complex disease like ADPKD.
Question 75:
A) Gonococcal urethritis with septic arthritis
B) Human papillomavirus (HPV) infection
C) Chlamydia trachomatis infection causing sexually acquired reactive arthritis (SARA)
D) Syphilis with secondary systemic symptoms
E) Herpes simplex virus (HSV) infection
Correct Answer: C) Chlamydia trachomatis infection causing sexually acquired reactive arthritis (SARA)
C) Chlamydia trachomatis infection
Correct: Chlamydia is a common cause of sexually acquired reactive arthritis (SARA), characterized by the triad of urethritis, conjunctivitis, and asymmetric arthritis, typically of large joints such as knees and ankles. This patient’s presentation aligns with SARA, which is triggered by a preceding Chlamydia infection. ( tip to remember SARA: can’t see, can’t pee, can’t climb up a tree)
Explanation:
A) Gonococcal urethritis with septic arthritis
- Incorrect: Gonococcal infection can cause disseminated gonococcal infection (DGI), which may lead to arthritis. However, this condition more typically presents with a migratory arthralgia pattern and often involves skin lesions. The triad of urethritis, conjunctivitis, and arthritis more strongly suggests a reactive (not septic) arthritis linked to Chlamydia.
B) Human papillomavirus (HPV) infection
- Incorrect: HPV 6 and 11 infection primarily causes genital warts and is not known to cause systemic symptoms such as urethritis, conjunctivitis, and arthritis. It is unrelated to reactive arthritis.
C) Chlamydia trachomatis infection
Correct: Chlamydia is a common cause of sexually acquired reactive arthritis (SARA), characterized by the triad of urethritis, conjunctivitis, and asymmetric arthritis, typically of large joints such as knees and ankles. This patient’s presentation aligns with SARA, which is triggered by a preceding Chlamydia infection. ( tip to remember SARA: cant see, can’t pee, cant climb up a tree)
D) Syphilis with secondary systemic symptoms
- Incorrect: Secondary syphilis can present with a wide range of systemic symptoms but does not typically cause reactive arthritis characterized by the triad seen here. Syphilis more commonly presents with a generalised rash, lymphadenopathy, and mucocutaneous lesions.
E) Herpes simplex virus (HSV) infection
- Incorrect: HSV primarily causes painful vesicular lesions on the genitalia and may lead to urethritis. However, it does not typically cause reactive arthritis with conjunctivitis, making it unlikely in this scenario.
Question 76:
Correct Answer: B) Overactive bladder (OAB)
OAB is characterized by symptoms of urinary urgency, frequency, and nocturia, often with urgency incontinence. The absence of pain, hematuria, or other concerning findings, along with a negative urinalysis, supports the diagnosis of OAB.
Explanation:
A) Stress urinary incontinence (SUI)
- Incorrect: SUI is characterized by involuntary urine leakage during physical activities that increase intra-abdominal pressure, such as coughing, sneezing, or lifting heavy objects. This patient denies such leakage, making stress incontinence unlikely.
C) Bladder cancer
- Incorrect: Bladder cancer often presents with painless hematuria, though urgency or frequency may occur in advanced cases. This patient has no hematuria and no other symptoms suggestive of malignancy, making this diagnosis unlikely.
D) Renal stone
- Incorrect: Renal stones typically cause severe, colicky flank pain that may radiate to the groin and is often accompanied by hematuria. The patient’s symptoms of urgency and frequency without pain or hematuria are not typical of a renal stone.
E) Urinary tract infection (UTI)
- Incorrect: UTIs can present with urgency, frequency, and nocturia, but they are usually accompanied by dysuria (painful urination), and a positive urinalysis with leukocytes, nitrites, or blood. In this case, the negative urinalysis makes UTI less likely.
Question 77:
Correct Answer: B) Epispadias
Correct: Epispadias is a rare congenital condition where the urethral opening is located on the dorsal side of the penis. The condition often presents with a broad, flat appearance of the penis and can be associated with bladder exstrophy. It is distinguished from hypospadias by the location of the urethral opening. It also causes a lack of dorsal curvature
Explanation:
A) Hypospadias
- Incorrect: Hypospadias is a congenital defect where the urethral opening is located on the ventral (underside) of the penis, often along the shaft or at the base. This is the opposite of epispadias, where the opening is on the dorsal (top) side of the penis.it also presents with a lack of ventral curvature.
C) Paraphimosis
Incorrect: paraphimosis is when the foreskin is retracted and cannot go back to its original state covering the glans penis, this can be very dangerous and tends to require immediate surgery as it can cause penile necrosis due to ischemia.
D) Testicular torsion
- Incorrect: Testicular torsion is a surgical emergency characterized by the twisting of the spermatic cord, leading to acute scrotal pain and swelling. It does not involve abnormalities in the structure of the penis.
E) Phimosis
- Incorrect: Phimosis refers to a condition where the foreskin cannot be retracted over the glans penis, often due to tightness. It is not related to the positioning of the urethral opening, so it does not match the described symptoms of dorsal urethral placement. However Phimosis is physiologically typical in boys up to age 6-7
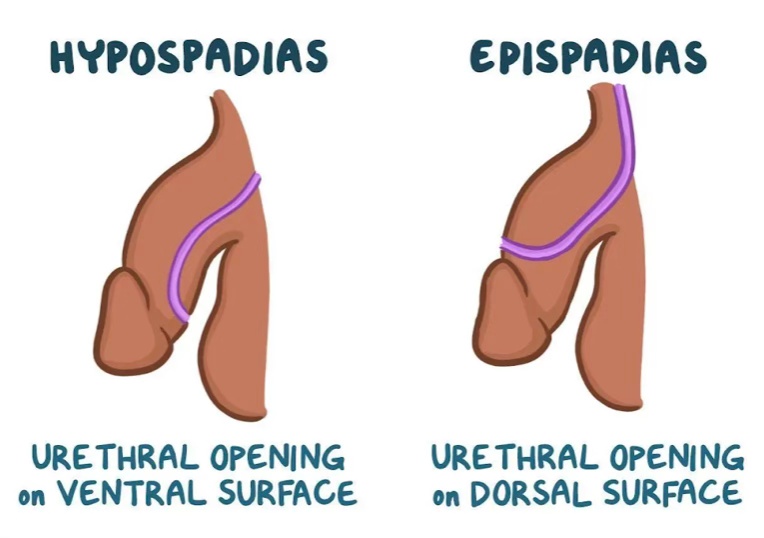
Question 78:
Correct Answer: A) Congenital adrenal hyperplasia causing a 21-hydroxylase deficiency, leading to a block in cortisol and aldosterone synthesis
A) 21-hydroxylase deficiency, leading to a block in cortisol and aldosterone synthesis
- Correct: 21-hydroxylase deficiency is the most common cause of congenital adrenal hyperplasia (CAH), characterized by impaired cortisol and aldosterone production. The block in cortisol and aldosterone synthesis leads to compensatory overproduction of adrenal androgens, causing virilization (enlarged clitoris, fused labia) and early signs of puberty in females. Elevated 17-hydroxyprogesterone is a hallmark of this condition due to the accumulation of precursors in the pathway. CAH is an Autosomal recessive condition.
Explanation:
B) 11β-hydroxylase deficiency, leading to excess mineralocorticoids and androgens
- Incorrect: 11β-hydroxylase deficiency results in impaired cortisol synthesis, leading to a buildup of 11-deoxycorticosterone (DOC), which has mineralocorticoid activity. This condition can cause hypertension, virilization, and ambiguous genitalia, but it typically presents with elevated blood pressure, unlike 21-hydroxylase deficiency, where blood pressure tends to be low due to aldosterone deficiency.
C) 3β-hydroxysteroid dehydrogenase deficiency, leading to impaired steroidogenesis and ambiguous genitalia
- Incorrect: 3β-hydroxysteroid dehydrogenase deficiency causes a broad impairment in steroid hormone production, including cortisol, aldosterone, and sex steroids. However, this condition typically leads to more severe phenotypic outcomes, including salt-wasting crises, and a lack of cortisol and aldosterone production. It also presents with both ambiguous genitalia and early signs of adrenal insufficiency, but it is less common than 21-hydroxylase deficiency.
D) congenital adrenal hyperplasia causing 17α-hydroxylase deficiency, resulting in low cortisol, sex steroids, and high aldosterone
- Incorrect: 17α-hydroxylase deficiency leads to low cortisol and sex steroids (like androgens and estrogens) and elevated aldosterone, which causes hypertension and hypokalemia. It can cause ambiguous genitalia in females but is more likely to present with clinical features of hypertension and low sexual development rather than virilization.
E) 17,20-lyase deficiency, leading to impaired androgen synthesis and ambiguous genitalia
- Incorrect: 17,20-lyase deficiency disrupts the conversion of pregnenolone and progesterone into androgens, leading to impaired androgen synthesis. In females, this results in underdevelopment of sexual characteristics and ambiguous genitalia. However, this is a rarer form of CAH and does not present with elevated 17-hydroxyprogesterone levels, as seen in 21-hydroxylase deficiency.

Question 79:
Correct Answer: B) Insulin resistance and hyperinsulinemia leading to elevated ovarian androgen production
Correct: In PCOS, insulin resistance is a key pathophysiological mechanism that leads to hyperinsulinemia. This condition stimulates the ovaries to produce excess androgens (testosterone), which causes symptoms like hirsutism, acne, and irregular cycles. Insulin resistance also contributes to the development of metabolic syndrome, commonly seen in PCOS patients.
Explanation:
A) Increased secretion of prolactin leading to hyperandrogenism
- Incorrect: Elevated prolactin can cause menstrual irregularities and galactorrhea but does not directly cause elevated androgen levels in PCOS. Prolactin-induced hyperandrogenism is rare and typically associated with prolactinomas, which would also present with other symptoms like galactorrhea.
C) Hypothalamic dysfunction resulting in altered GnRH pulse frequency
- Incorrect: While abnormal GnRH pulse frequency (increased LH
ratio) is a characteristic feature of PCOS, it is secondary to other pathophysiological factors such as insulin resistance and elevated androgen levels. Hypothalamic dysfunction is not the primary cause of PCOS.
D) Ovarian resistance to FSH, causing an imbalance in follicle maturation
- Incorrect: In PCOS, there is typically an imbalance in the LH
ratio, with elevated LH levels rather than ovarian resistance to FSH. This imbalance impairs follicular maturation, leading to the formation of multiple small cysts in the ovaries. Ovarian resistance to FSH is not the main cause in PCOS.
E) Decreased cortisol clearance resulting in elevated adrenal androgen levels
- Incorrect: While cortisol abnormalities can be involved in other endocrine disorders like Cushing’s syndrome, they are not the primary cause of PCOS. Elevated adrenal androgens are typically not the main source of hyperandrogenism in PCOS, which is primarily driven by ovarian overproduction of androgens due to insulin resistance.
Question 80:
Correct Answer: C) Elevated follicle-stimulating hormone (FSH), decreased estradiol, and low progesterone
Correct: As women approach menopause, ovarian function declines, leading to a decrease in estradiol production. FSH levels rise due to the reduced feedback inhibition from estradiol, as the body attempts to stimulate the ovaries to produce more estradiol. Low progesterone levels are seen because ovulation becomes infrequent and eventually ceases, leading to a lack of corpus luteum formation. So to summarise perimenopause = High LH and FSH and LOW oestrogen and progesterone,
Explanation:
A) Elevated estradiol, decreased FSH, and normal progesterone
- Incorrect: Elevated estradiol is unlikely during the menopausal transition, as estradiol levels generally decrease as the ovaries become less responsive. In the perimenopausal phase, estradiol can fluctuate, but it is typically low, not elevated. Additionally, FSH is expected to be elevated during perimenopause due to decreased feedback from estradiol.
B) Elevated luteinizing hormone (LH), elevated estradiol, and low progesterone
- Incorrect: While LH levels may be elevated during the perimenopausal transition, estradiol would not be elevated in the way it is in pre-menopause. Estradiol is typically low, and progesterone is low because ovulation becomes irregular or ceases, but the primary pattern involves elevated FSH rather than elevated LH.
D) Decreased LH, decreased estradiol, and high progesterone
- Incorrect: Decreased LH is not a typical finding in perimenopause. In fact, LH levels usually increase due to the declining feedback from estradiol. Additionally, high progesterone would not be expected in menopause since ovulation becomes infrequent or ceases, and the corpus luteum does not form to produce progesterone.
E) Decreased estradiol, elevated FSH, and low Lh
- Incorrect: While this option is close, the most accurate reflection of menopause and the perimenopausal transition is an elevated FSH, decreased estradiol, and elevated LH, FSH becomes significantly elevated as ovarian reserve declines, and estradiol levels are generally lower but can fluctuate. However, FSH and LH elevation is key in distinguishing menopause.
Question 81:
Correct Answer: C) Endometriosis, characterized by ectopic endometrial tissue outside the uterus
Correct: Endometriosis is the most likely diagnosis in this case. It involves the presence of endometrial tissue (the tissue that lines the uterus) outside the uterus, typically affecting the ovaries, fallopian tubes, and pelvic peritoneum. Symptoms include dysmenorrhea, deep pelvic pain during intercourse (dyspareunia), and infertility. MRI or laparoscopy is typically used for diagnosis, revealing ectopic endometrial implants, cysts (chocolate cysts), or adhesions.Typically the pain goes away each menstruation due to the tissue being broken down and passed away each menstruation.
Explanation:
A) Endometrial hyperplasia, characterized by abnormal proliferation of the endometrial lining
- Incorrect: Endometrial hyperplasia involves the abnormal proliferation of the endometrial glands and stroma, usually due to prolonged estrogen exposure. While it may cause abnormal bleeding or heavy periods, it does not typically present with pelvic pain, infertility, or ectopic endometrial tissue outside the uterus, which is characteristic of endometriosis.
B) Leiomyomas, characterized by smooth muscle tumours within the uterus
- Incorrect: Leiomyomas (fibroids) are benign smooth muscle tumours within the uterus. They often cause symptoms such as heavy menstrual bleeding, pelvic pressure, and sometimes infertility, but they do not cause pelvic pain during intercourse or deep dyspareunia. Additionally, fibroids are typically seen as well-defined masses on imaging, unlike the scattered endometrial-like tissue seen in endometriosis.
D) Endometrial polyps, characterized by localised growth of endometrial tissue within the uterine cavity
- Incorrect: Endometrial polyps are localised overgrowths of endometrial tissue within the uterine cavity. They are usually asymptomatic but may cause irregular bleeding. They do not present with the deep pelvic pain or infertility typically associated with endometriosis, and the endometrial tissue in polyps is contained within the uterus, not outside it.
E) Adenomyosis, characterized by endometrial tissue invading the myometrium
- Incorrect: Adenomyosis involves the invasion of endometrial tissue into the myometrium (muscle layer of the uterus). It often causes heavy menstrual bleeding and pelvic pain, particularly during menstruation, but the pain is typically more diffuse and not associated with deep pain during intercourse. Unlike endometriosis, adenomyosis does not present with ectopic endometrial tissue outside the uterus. Imaging may show a diffusely enlarged uterus, but it does not show the scattered ectopic tissue characteristic of endometriosis.
Question 82:
Correct Answer: A) The basal layer is where the stem cells of the epithelium reside, making it the primary site for initial oncogenic mutations
- Correct: The basal layer of the cervical epithelium contains the stem cells that are responsible for the regeneration of the epithelium. These cells are the first to undergo mutations when infected by high-risk human papillomavirus (HPV). As these mutated cells divide, they begin to migrate upward through the layers of the epithelium, resulting in dysplastic changes that progress from the basal layer to the apical layer. This upward progression of cellular changes is a hallmark of CIN. Furthermore the apical layer of cells get shredded so you won’t see the changes.
Explanation:
B) The apical layer of the epithelium is more exposed to carcinogens, so mutations tend to start from the top and progress downward
- Incorrect: The apical (surface) layer of the epithelium is not the site where oncogenic mutations typically begin. Carcinogenesis in cervical cancer, particularly in CIN, starts in the basal layer, as this is where stem cells are located. The apical layer does not have the same potential for initiating genetic changes due to its differentiation status.
C) The basal cells are the most differentiated and thus have the highest potential for undergoing genetic changes leading to CIN
- Incorrect: The basal cells are least differentiated, not the most differentiated. This undifferentiated nature is what makes them susceptible to HPV infection and subsequent mutations. Differentiated cells (e.g., those near the surface of the epithelium) are less likely to undergo the initial stages of transformation due to their already specialized function and lack of division.
D) The immune system targets the basal cells first, leading to a gradual accumulation of mutations as the cells migrate upward
- Incorrect: While the immune system plays a role in responding to HPV infection, it is not the immune system’s targeting of basal cells that causes mutations. Mutations arise primarily from the direct effects of HPV on the DNA of basal cells. The immune response might affect the persistence of the infection but does not explain why the mutations occur first in the basal layer.
E) The basal layer is closest to the blood supply, making it more susceptible to the initial effects of HPV infection and subsequent transformation
- Incorrect: While the basal layer is indeed closer to the blood supply, this is not the reason why mutations occur there first. The basal cells are more susceptible to HPV infection due to their role as stem cells, which are actively dividing and therefore more likely to harbor genetic mutations. The blood supply is important for nourishing the epithelium but is not directly responsible for the initiation of carcinogenesis.
Question 83:
Correct Answer: A) GTD typically involves the formation of a hydatidiform mole, whereas GTN involves malignancy that has the potential for invasion and metastasis and a constantly high beta- HCG levels even after removal of miscarriage.
- Correct: Gestational trophoblastic disease (GTD) is a broad term that encompasses conditions such as hydatidiform moles, which are benign growths of trophoblastic tissue that typically do not invade beyond the uterus. On the other hand, gestational trophoblastic neoplasia (GTN) represents a malignant progression, where the trophoblastic tissue can invade the uterine wall and metastasize, usually to the lungs, liver, or brain. This distinction is key to differentiating between the two conditions.Furthermore GTN causes a high beta-HCG level even after removal of the miscarriage, therefore this answer option is correct.
Explanation:
B) GTD is characterized by a persistently low beta-hCG level after miscarriage, whereas GTN typically shows a dramatic rise in beta-hCG levels
- Incorrect: In both GTD and GTN, beta-hCG levels are typically elevated. However, while beta-hCG may decrease after the removal of a hydatidiform mole (a benign form of GTD), persistent high beta-hCG levels or a rise in beta-hCG after treatment is more suggestive of GTN, which represents a malignant progression.
C) In GTD, the uterus usually appears normal on ultrasound, whereas in GTN, the ultrasound shows a characteristic “snowstorm” pattern
- Incorrect: The “snowstorm” pattern is characteristic of a complete hydatidiform mole (a form of GTD), not GTN. In GTD, the ultrasound may show a heterogeneous mass or vesicular pattern (incomplete mole) or the classic “snowstorm” appearance (complete mole). GTN typically presents with a mass or irregular mass in the uterus, but it does not have a “snowstorm” pattern; rather, it shows evidence of invasive disease.
D) GTD is associated with irregular bleeding but no symptoms of metastasis, whereas GTN is typically confined to the uterus without risk of distant spread
- Incorrect: While GTD can cause irregular bleeding due to the presence of a molar pregnancy, it is GTN that has the potential for metastasis and spread beyond the uterus. GTN, which includes conditions such as choriocarcinoma, can invade the uterine wall and spread to distant organs, whereas GTD (molar pregnancies) are typically confined to the uterus and may resolve without metastasis.
E) GTD is associated with a high risk of invasive disease and distant metastasis, whereas GTN is a self-limiting condition that resolves spontaneously without treatment
Incorrect: This statement is incorrect because it reverses the roles of GTD and GTN. GTN is the condition with the potential for invasive disease and metastasis. GTD, particularly in the form of a hydatidiform mole, is a benign condition that can often be treated with uterine evacuation and does not typically result in metastasis.
